Reimbursement Politics
Unlike the rest of the U.S. economy, reimbursement for healthcare is not a simple matter of supply and demand. Reimbursement decisions are based to an increasing extent on politics. Not surprisingly, this nonmarket approach has resulted in quality concerns in healthcare. Less-than-optimum healthcare outcomes are in part due to the lack of capital and incentives available from the current reimbursement system—a reimbursement system that unfortunately has become a matter of politics, forcing physicians and other providers to manipulate or “game” the system in order to obtain more appropriate reimbursement for patient care services they provide.
SUSTAINABLE GROWTH RATE FORMULA
Perhaps nowhere in healthcare has reimbursement been based more on politics than with regard to physician reimbursement. Since Medicare’s inception, the federal government has been involved in reimbursement decisions. In the early years of Medicare, when financial constraints were not a major Medicare driver, physician reimbursement was based on usual and customary charges. Later, when funding became an issue, reimbursement was instead dictated to physicians from the federal government. Physician charges are now subject to the Sustainable Growth Rate (SGR) Formula. This formula ties physician payment updates to a number of factors:
• Growth in input costs
• Growth in fee-for-service enrollment
• Growth in the volume of physician services relative to growth in the national economy
The result of this formula is that the more services utilized for reasons of demand, the less the reimbursement to physicians in subsequent years, in hopes that this will decrease utilization and expenditures.
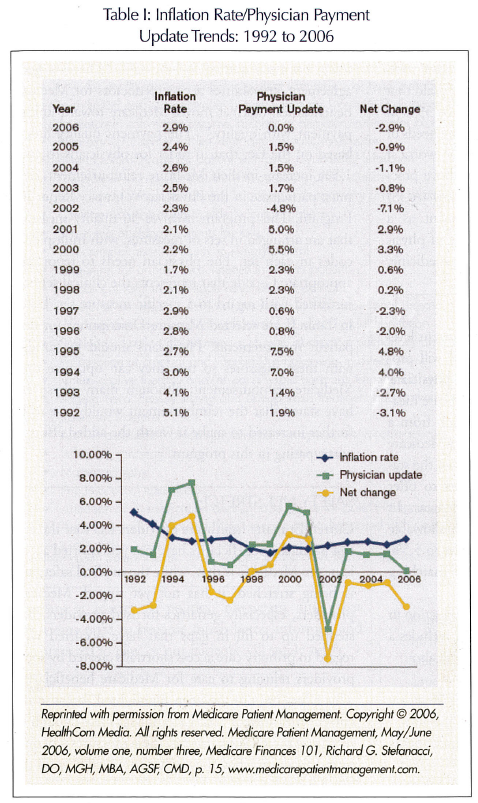 As a result of the SGR formula, there will be a substantial negative payment update from 2006 to at least the year 2011. Despite the SGR formula, the Medicare Payment Advisory Commission (MedPAC) reimbursement recommendations to Congress are based on other factors, such as beneficiary access to services. Table I demonstrates the trends of the physician payment updates against inflation rates over the last 15 years. The net effect on physician practice profitability is the difference between physician reimbursement and input costs. This net difference for a practice is actually greater than the difference using a general inflation number, since physician practice costs are increasing at a rate greater than inflation. Professional liability insurance continues to lead as the fastest growing input cost. However, even using the lower general inflation number, which has averaged 2.76% each year for the last 15 years, physician payment updates have averaged only 2.28% during this same period, resulting in a net average decrease.1 It’s important to note that physician practice profitability may be used to increase physician income, but is also an important source of potential capital to reinvest back into the practice for health information technology, additional care team members, and other resources to optimize care quality.
As a result of the SGR formula, there will be a substantial negative payment update from 2006 to at least the year 2011. Despite the SGR formula, the Medicare Payment Advisory Commission (MedPAC) reimbursement recommendations to Congress are based on other factors, such as beneficiary access to services. Table I demonstrates the trends of the physician payment updates against inflation rates over the last 15 years. The net effect on physician practice profitability is the difference between physician reimbursement and input costs. This net difference for a practice is actually greater than the difference using a general inflation number, since physician practice costs are increasing at a rate greater than inflation. Professional liability insurance continues to lead as the fastest growing input cost. However, even using the lower general inflation number, which has averaged 2.76% each year for the last 15 years, physician payment updates have averaged only 2.28% during this same period, resulting in a net average decrease.1 It’s important to note that physician practice profitability may be used to increase physician income, but is also an important source of potential capital to reinvest back into the practice for health information technology, additional care team members, and other resources to optimize care quality.
The result of the SGR has been to set Medicare payments at less than commercial insurers, although it is important to note that reimbursement amounts have regional variation. For example, a basic check-up that a typical office charges $50 or $55 for is paid by private insurers at $40 or $45, while Medicare pays only about $35. For a patient visit related to a more involved problem such as diabetes—which may take 15-20 minutes—the office charges of about $70 are paid by Medicare as slightly less than $50 and by private insurers anywhere from $55 to $70, with the average private insurer paying $60.
RECOGNITION OF PRIMARY CARE ISSUES
The Centers for Medicare and Medicaid Services (CMS) in its new Medicare rule specifically increases financial reimbursement for evaluation and management (E & M) services. Under the rule change for this year, Medicare will boost reimbursement for the work component of two of the most common types of patient visits. The change applies to office and other outpatient visits. The intent is to reward for time and effort that physicians spend with patients in evaluating their condition, and for advising and assisting them in managing their health.2 Despite these increases in E & M codes, physician reimbursement continues to lag behind practice inflation.
The American Medical Association (AMA) has said that nearly half of physicians it surveyed—or 45%—will stop seeing Medicare patients as reimbursement continues to lag behind practice cost increases.3 Additionally, if overall primary care reimbursement rates don’t improve, not only will fewer physicians accept Medicare as shown by the AMA survey, but the number of family doctors will also fall behind the needs of our aging population. The attraction of specialized areas of medicine in which Medicare and private reimbursement levels are higher, and the prospect of lucrative careers totally outside of medicine, already lead many potential family doctors to look elsewhere. A report from the American Academy of Family Physicians highlighted the existing concern about the need for more family doctors in general. The report said that the number of family doctors must increase by 39% in the next 14 years to keep up with primary care needs of U.S. residents.4 This shortage is likely to be worse if reimbursement is not allowed to increase above practice inflation. The American Geriatrics Society (AGS) has also identified inadequate reimbursement as a major factor in the well-recognized shortage of physicians and other professionals within geriatric medicine.
LEGISLATIVE CHANGES
HR 6408 is the bill that will maintain the current level of Medicare physician reimbursements, and will provide a 1.5% increase in reimbursements to physicians who agree to report data on certain quality-of-care measures. The legislation will remove $6.5 billion from a stabilization fund established under the 2003 Medicare law to help cover the cost. Congress established the stabilization fund to encourage health insurers to offer Medicare Advantage plans in underserved areas. In addition, the bill will reduce the maximum allowable rate at which states can tax Medicaid providers to 5.5% from 6%, a move that would decrease federal matching funds to states, to help cover the cost.
In addition to the reversal of a scheduled reduction in Medicare physician reimbursements, the bill includes a number of other provisions. The legislation will also:
• Extend for 1 year an exceptions process for Medicare therapy services
• Provide a 1.6% increase in Medicare reimbursements to dialysis facilities
• Establish a Physician Assistance and Quality Initiative Fund available to finance future Medicare physician reimbursement and quality improvement proposals
This legislation was signed into law on December 27, just days before the planned 5.1% reduction in physician Medicare reimbursement would have begun.
PHYSICIAN VOLUNTARY REPORTING
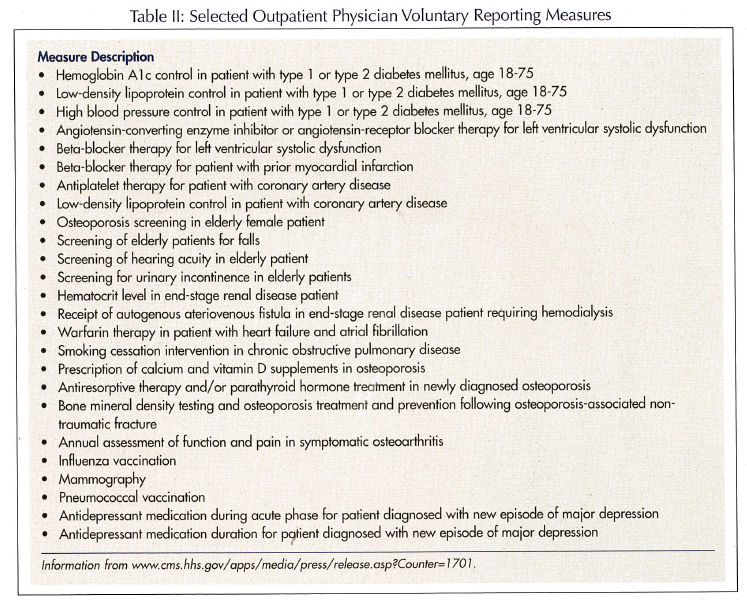 Senate Finance Committee Chair Chuck Grassley (R-Iowa) has been quoted to have said, “This is a good agreement. It stabilizes access to doctors for Medicare beneficiaries, (and) it moves Medicare toward linking payment with quality.”5 The payment quality link is based on the fact that in order for physicians to get a 1.5% increase in their Medicare reimbursement, they must participate in the Physician Voluntary Reporting Program. This program involves 36 quality measures that are arranged in sets of measures, with multiple G-codes in each set. The physician needs to report the appropriate G-code that represents the clinical services furnished with regard to a specific measure set. Listed in Table II are selected Measure Descriptions for outpatient measurements. Physicians should be familiar with these measures so that they can optimize their Medicare reimbursement, although many physicians have stated that the reimbursement would have to be further increased to make it worth the added effort of participating in this program.
Senate Finance Committee Chair Chuck Grassley (R-Iowa) has been quoted to have said, “This is a good agreement. It stabilizes access to doctors for Medicare beneficiaries, (and) it moves Medicare toward linking payment with quality.”5 The payment quality link is based on the fact that in order for physicians to get a 1.5% increase in their Medicare reimbursement, they must participate in the Physician Voluntary Reporting Program. This program involves 36 quality measures that are arranged in sets of measures, with multiple G-codes in each set. The physician needs to report the appropriate G-code that represents the clinical services furnished with regard to a specific measure set. Listed in Table II are selected Measure Descriptions for outpatient measurements. Physicians should be familiar with these measures so that they can optimize their Medicare reimbursement, although many physicians have stated that the reimbursement would have to be further increased to make it worth the added effort of participating in this program.
SAFETY NET STRETCH
Currently, many healthcare providers feel that the reason Medicare beneficiaries have not yet reported access issues to MedPAC is that, while the medical safety net is being stretched, it has not yet ripped. Medicare providers, especially geriatrics-focused providers, had stepped up to fill in gaps that have occurred with regard to primary care access shortfalls created by some providers refusing to care for Medicare beneficiaries. This effect has not yet been highlighted, because the current measures of access are not sensitive enough to recognize these issues; instead, these measures will only sound an alarm when the net has stretched beyond the breaking point.
In order for the net to not break but instead be strengthened, physicians must work with Medicare beneficiaries so that legislators realize that in order to optimize outcomes, capital and incentives are required beyond what the current reimbursement system is providing. Since our current reimbursement system has become a matter of politics, physicians and other providers need to become much better informed and be prepared to play, or our patients will surely suffer.
Correction In the article “Medicare Gets Tough” by Richard G. Stefanacci, DO, MGH, MBA, AGSF, CMD, that appeared in the December 2006 issue, the sentence “Now Medicare beneficiaries with incomes over $80,000 for individuals and twice that for married couples will be subject to monthly premiums above $93.50 for Medicare Part D.” was incorrect. It should read: “Now Medicare beneficiaries with incomes over $80,000 for individuals and twice that for married couples will be subject to monthly premiums above $93.50 for Medicare Part B.”
Please send any questions or experiences about Medicare Part D you would like to share with readers to: BSpivack@Waveny.org









