Cytokines and the Care of the Older Adult
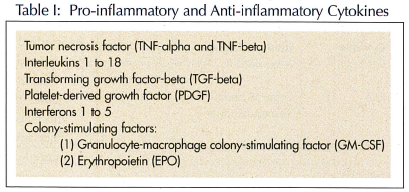
Cytokines are low-molecular-weight extracellular signalling proteins secreted by specific cells. They can alter the behavior of cells in their close proximity (commonly referred to as a paracrine action) and can control various aspects of cellular growth and differentiation.1-3 They may also act in an endocrine or autocrine manner, where the substance secreted stimulates the secretory cell itself. They are secreted by a vast range of cells, most often by white blood cells, but also by virtually all other nucleated cells.4 Those secreted by lymphocytes are termed lymphokines. Cytokines secreted by monocytes are termed monokines. Other types of cytokines are categorized as growth factors and colony-stimulating factors, which regulate the proliferation of blood cells and growth of body tissue. Action of cytokines is mediated through receptor binding on target cells. Soluble receptor molecules exist for some cytokines that bind to cytokines and transport it to the target cell.5 Cytokines have a multitude of functions, with most centered around immune and inflammatory responses. The peripheral effects of cytokines may be growth stimulating or inhibiting, and pro- or anti-inflammatory6-8 (Table I).
ACTIONS OF CYTOKINES
Central cytokine actions include changes in body temperature, mood, sleep, fatigue level, social exploration, and appetite.9-14 Studies involving interleukin-6 (IL-6) knock-out animals suggest that IL-6 plays an important role in stimulating the behavioral changes associated with sickness, including anorexia and a decrease in social interactions.14 Tumor necrosis factor-alpha (TNF-alpha) causes anorexia leading to extensive weight loss and tissue wasting (cachexia) in patients with chronic infection or inflammation.15-17 Interferon-alpha also stimulates sickness behavior, including myalgia, fatigue, and fever.3 Transforming growth factor-beta (TGF-beta) stimulates proliferation of cells during wound repair.18 Platelet-derived growth factor (PDGF) is also involved in tissue repair and can turn on cell division in a variety of tissue. Granulocyte-macrophage colony-stimulating factor (GM-CSF) stimulates white blood cell production and is produced by activated T cells.19 Erythropoietin (EPO) stimulates the production of red blood cells and is produced by the kidney.20 Normally, EPO is produced as a result of hypoxia detected by an oxygen sensor. It then acts back on an effector receptor. There is normally a rise in levels in anemia.
Tissue destruction or infection leads to a nonspecific rise of C-reactive protein (CRP) and serum amyloid protein following an acute-phase stimulus. CRP increases after acute and chronic infection, in arthritic and other inflammatory disorders, tissue necrosis, neoplasia, cardiovascular disease, insulin resistance syndromes, oral estrogen intake, smoking, and coffee consumption.21 Conditions that lower CRP levels include liver disease, weight loss, exercise, moderate alcohol intake, and lipid-lowering agents that inhibit hepatic hydroxymethyl glutaryl coenzyme A. The earliest mediators of the acute-phase reaction include cytokines interleukin-1’s (IL-1’s) and TNF-alpha. They both induce a second wave of cytokines that includes IL-6 and chemokines. IL-6 is an important anti-inflammatory and immunoregulatory cytokine. It is required for controlling local and systemic inflammatory responses. IL-6 is released from macrophages and T lymphocytes. Chemokines regulate the influx of leukocytes to the site of inflammation. The bioactivity of TNF-alpha and IL-1beta is inhibited by naturally occurring antagonists such as IL-1 receptor antagonist (Ra), and soluble TNF receptors (sTNFR) as well as the anti-inflammatory cytokine IL-10. Westendorp22 has suggested that the balance between pro-inflammatory and anti-inflammatory cytokines favors either a long life or reproductive success. Thus, persons with high levels of IL-10 will have few children but live a long time. Examples of pro- and anti-inflammatory cytokines appear in Table I.
CYTOKINES AND THEIR ASSOCIATION WITH DISEASE STATES
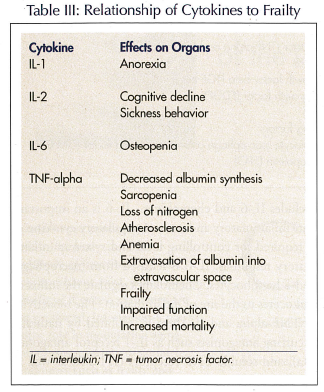
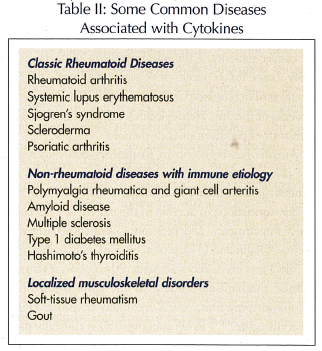 A number of conditions are largely associated with the activated cytokine cascade, and produce musculoskeletal symptoms that lead to decreased functional status or poor quality of life (Table II). Rheumatoid disorders are classical diseases of the cytokine cascade. Similar disorders, such as osteoporosis and Paget’s disease, primarily affect the musculoskeletal system. Other disorders, which include metastatic carcinoma and multiple myeloma, cause secondary effects in the musculoskeletal system. Immune disorders of the endocrine system, such as Type 1 diabetes mellitus or thyroid disorders, also have secondary effects on the musculoskeletal system. Recently, there has been an increased awareness that the cytokine response to nonspecific inflammation may be a component of the pathophysiology of frailty (Table III), functional decline, and death in older persons.23,24 Thus, an increasing number of conditions are being recognized as primary immune complex diseases that may or may not present with musculoskeletal manifestations.
A number of conditions are largely associated with the activated cytokine cascade, and produce musculoskeletal symptoms that lead to decreased functional status or poor quality of life (Table II). Rheumatoid disorders are classical diseases of the cytokine cascade. Similar disorders, such as osteoporosis and Paget’s disease, primarily affect the musculoskeletal system. Other disorders, which include metastatic carcinoma and multiple myeloma, cause secondary effects in the musculoskeletal system. Immune disorders of the endocrine system, such as Type 1 diabetes mellitus or thyroid disorders, also have secondary effects on the musculoskeletal system. Recently, there has been an increased awareness that the cytokine response to nonspecific inflammation may be a component of the pathophysiology of frailty (Table III), functional decline, and death in older persons.23,24 Thus, an increasing number of conditions are being recognized as primary immune complex diseases that may or may not present with musculoskeletal manifestations.
CYTOKINES AND CACHEXIA
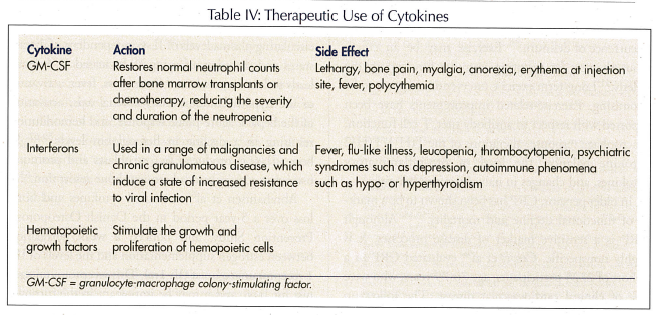
 Recently, a body of evidence has emerged that suggests that inadequate caloric intake is associated with an excess production of cytokines. The syndrome of cachexia, the cytokine-induced wasting of protein and energy stores, is related to a number of disease conditions, including cancer,25 end-stage renal disease,26 chronic pulmonary disease,27 congestive heart failure,28 rheumatoid arthritis,29 and AIDS.30 Disease states directly associated with cytokines result in feeding suppression and lower intake of nutrients. Interleukin-1 beta and TNF act on the glucose-sensitive neurons in the ventromedial hypothalamic nucleus (a “satiety” site) and the lateral hypothalamic area (a “hunger” site).31 The data suggest that cytokine levels are commonly associated with disease conditions characterized by cachexia that may play a role in appetite suppression, mortality, and weight loss. Cytokine-induced anorexia is the most common cause of poor caloric intake observed in the acute care setting,32 and affects community-dwelling older persons as well. Therapeutic use of cytokines is becoming more common (Table IV).
Recently, a body of evidence has emerged that suggests that inadequate caloric intake is associated with an excess production of cytokines. The syndrome of cachexia, the cytokine-induced wasting of protein and energy stores, is related to a number of disease conditions, including cancer,25 end-stage renal disease,26 chronic pulmonary disease,27 congestive heart failure,28 rheumatoid arthritis,29 and AIDS.30 Disease states directly associated with cytokines result in feeding suppression and lower intake of nutrients. Interleukin-1 beta and TNF act on the glucose-sensitive neurons in the ventromedial hypothalamic nucleus (a “satiety” site) and the lateral hypothalamic area (a “hunger” site).31 The data suggest that cytokine levels are commonly associated with disease conditions characterized by cachexia that may play a role in appetite suppression, mortality, and weight loss. Cytokine-induced anorexia is the most common cause of poor caloric intake observed in the acute care setting,32 and affects community-dwelling older persons as well. Therapeutic use of cytokines is becoming more common (Table IV).
CYTOKINES AND ANEMIA
Anemia is one feature of frailty. Based on the World Health Organization definition of anemia in people over age 65 years (hemoglobin level less than 12 g/dL for women, and 13 g/dL for men), anemia is commonly prevalent in nursing homes and may be as high as 50%, according to the National Geriatrics Research Consortium. The pathophysiology of anemia of chronic disease, which is commonly seen in the geriatric population, has been associated with IL-1, TNF-alpha, and IL-6.33 Other types of anemia include iron deficiency anemia, B12 deficiency, chronic renal disease, idiopathic, and myelodysplastic syndrome (less common).
Inhibition of erythropoiesis by the direct inhibition of EPO, and uptake of iron into the red blood cell is observed. IL-1, TNF-alpha, TGF-beta, and IL-6 have been shown to inhibit the hypoxia induction of EPO.34 In cancer patients,35 the administration of IL-6 on a daily basis for 6 weeks was associated with a 7% decrease of hemoglobin in 3 days, and a 19% drop after 4 weeks of therapy. Hemoglobin levels normalized after 1 month of cessation of IL-6 therapy.
Anemia has been shown to independently increase the risk of mortality in the elderly,36,37 and to lead to congestive heart failure and worsen angina pectoris.38,39 Other associations of anemia in the elderly are: (1) cognitive impairment; (2) depression; (3) functional impairment; (4) falls; and (5) loss of activity of daily living.40-42
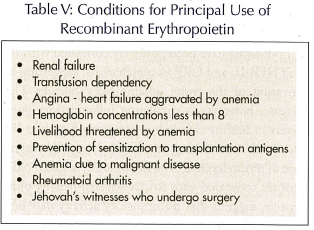 EPO acts on its receptor, which then activates intracellular mechanisms leading to the stimulation of a colony-forming unit, which eventually transforms into an erythrocyte.43,44 Recombinant EPO is clinically useful in a range of conditions including chronic renal failure. Conditions with chronic cytokine production affect reticulocytosis by inhibiting the effects of EPO on bone marrow.45 The principal use is in renal failure and other conditions (Table V). Side effects include increased blood pressure, thrombosis of vascular access sites, flu-like symptoms, seizures, and skin reactions.
EPO acts on its receptor, which then activates intracellular mechanisms leading to the stimulation of a colony-forming unit, which eventually transforms into an erythrocyte.43,44 Recombinant EPO is clinically useful in a range of conditions including chronic renal failure. Conditions with chronic cytokine production affect reticulocytosis by inhibiting the effects of EPO on bone marrow.45 The principal use is in renal failure and other conditions (Table V). Side effects include increased blood pressure, thrombosis of vascular access sites, flu-like symptoms, seizures, and skin reactions.
CYTOKINES AND AGING
Aging is accompanied by 2-4-fold increases in plasma/serum levels of inflammatory mediators, such as cytokines and acute-phase proteins.46 A wide range of factors seems to contribute to this low-grade inflammation, including an increased amount of fat tissue, decreased production of sex steroids, smoking, subclinical infections (eg, asymptomatic bacteriuria), and such chronic disorders as cardiovascular diseases and Alzheimer’s disease. Furthermore, there is some evidence that aging is associated with a dysregulated cytokine response following stimulation. The aging process itself might be an intrinsic factor in the development of anemia, possibly through the age-related dysregulation of certain proinflammatory cytokines, such as IL-6.46 Although the mechanism underlying the association between increased IL-6 and anemia has not been fully elucidated, it has been suggested that, as with other cytokines, it involves direct inhibition of EPO production or interaction with the EPO receptor.
Polymorphisms in the promoter regions of pro- and anti-inflammatory cytokine genes influence the level of cytokine production and the aging process.47 Thus, a genotype for high pro-inflammatory cytokine production results in high cytokine production, and may accelerate the rate of tissue loss. Conversely, polymorphisms in the genes for anti-inflammatory cytokines may result in a slowing of tissue loss. Cytokines are potent anorectic agents. Many older persons have mild inflammatory disorders that lead to anorexia.48 There is also evidence that cytokines play a role in the pathogenesis of anorexia and sarcopenia, thus accelerating the development of frailty in older persons.49 Increased cerebral secretion of cytokines due to a wide range of physically stressful events plays an important role in the occurrence of delirium.50 Exercise may be an efficacious therapy for restoring immune function in the elderly.51 Long-term exercise interventions appear to be promising. Exercise-related improvements have been reported with respect to antibody titer, T cell function, macrophage response, alterations of the T(H)1/T(H)2 cytokine balance, the level of pro-inflammatory cytokines, and changes in naive/memory cell ratio.
In older persons, CRP has been shown to be a marker of functional decline and mortality.52-55 Although CRP is a sensitive marker of disease processes, it is highly nonspecific. Cesari et al56 evaluated CRP in a cohort of 2225 participants, age 70-79 years, who were free of clinical cardiovascular disease. The follow-up was for 4 years. Participants with CRP levels in the highest tertile (> 2.5 mg/L) were not at significantly elevated risk of incident coronary heart disease after adjusting for smoking, diabetes, hypertension, body mass index, high-density lipoprotein (HDL) cholesterol, triglyceride levels, and albumin levels. There was statistical evidence for a gender interaction.
Aging itself is associated with complex changes in the immune system. There is a progressive increase in the concentration of glucocorticoids and catecholamines with aging, and decreased production of growth and sex hormones, a pattern suggestive of that seen in chronic stress. Aging has also been associated with increased levels of circulating inflammatory components in the blood including elevated concentrations of TNF-alpha, IL-6,52 IL-1Ra, sTNFR, acute-phase proteins such as C-reactive protein and serum amyloid A, and high neutrophil counts. Plasma levels of TNF-alpha have been positively correlated with IL-6, sTNFR-II, and CRP in centenarians, suggesting an activation of the entire inflammatory cascade. This increase, however, in circulating inflammatory parameters in healthy elderly humans is small and far less than levels seen during acute infections. The magnitude of serum levels of IL-6 in randomly selected older persons, compared with strictly selected healthy older persons, suggests that inflammatory activity may be a marker of health status.57
On the other hand, a study of persons aged 70 years or older found that age was associated with increased circulating plasma levels of IL-6 independent of disease states and disorders of aging.58 Increased IL-6 levels leads to loss of muscle and bone mass, fever, activation of the hypothalamic-pituitary-adrenal axis, activation of the hepatic acute-phase response, and hemodilution resulting in a decline in hemoglobin levels.59-62 In bone, IL-6 is produced by osteoblasts and promotes osteoclast activity and subsequent bone resorption.63
Abrahamsen et al64 measured cytokines and bone loss over a 5-year period in the Danish Osteoporosis Prevention Study, and noticed a weak correlation between estrogen supplementation and the levels of IL-1 receptor anatagonist (IL-1ra). This receptor is an agonist for IL-6, and it may be important in the turnover of bone with aging. It is not clear whether estrogen supplementation slows bone turnover by lowering levels of this antagonist.65 Testosterone has been shown to suppress IL-6 production from bone.66 Parathyroid hormone increases the production of IL-6 from osteoblasts,67 and stimulates the hepatic production of IL-6 and its soluble receptor.68
Some of these changes in cytokine production with aging are inconsistent.69 It is uncertain whether changes in cytokine levels are due to age itself or to underlying disease. On the other hand, elevated IL-6 levels have been shown cross-sectionally to be inversely associated with muscle mass and strength, physical performance, balance, and walking speed, and positively associated with death.55,70-72 Ferruci and colleagues73 showed in a cross-sectional study that IL-6 levels predicted development of disability over the subsequent 4 years. The increase in plasma levels of IL-6 with age may occur as the result of catecholamine hypersecretion and sex-steroid hyposecretion.74
Numerous acquired influences (eg, visceral obesity, smoking, stress) also trigger IL-6 release.75 Subclinical infections such as Chlamydia pneumoniae or Helicobacter pylori, or dental infections and asymptomatic bacteriuria may play a mechanistic role.76 Epidemiologic studies clearly demonstrate that “immunosenescence” contributes to all-cause mortality.77 Pro-inflammatory cytokines are thought to play a pathogenetic role in age-associated diseases such as Alzheimer’s disease, Parkinson’s disease, atherosclerosis, type 2 diabetes, sarcopenia, and osteoporosis. These conditions increase morbidity and lower functional status in affected persons. A causal relation between impaired immune function in aging and increased susceptibility to infections remains to be demonstrated. In general, the data suggest that low-grade inflammatory activity in older populations is caused by a dysregulated cytokine production, which is further exacerbated by age-associated pathology.
SUMMARY
Cytokines are involved in a multitude of actions that affect the aging process with modulation of the immune response, as well as its regulation. They are important in the development of anemia, which then leads to a cascade of events that affect functional outcome and mortality in the elderly. By understanding how cytokines modulate aging and other processes one can provide improved care that can lead to improved outcomes in the geriatric population.
The author reports no relevant financial relationships.










