Who Controls the Prescription?
As physicians, we have been taught that our job is to make the correct diagnosis and then write the right prescription, assuming that our prescription would be filled. Enter Medicare Part D with its aim to increase access to medications for seniors. But has this actually occurred? A recently completed survey showed that 94% of physicians are confused about Medicare Part D, especially with regard to accessing specific prescriptions.1 This difficulty has resulted in 70% of physicians spending at least 20% more time on administrative tasks related to Medicare Part D.1 Clearly, Medicare Part D has not produced an easier path to access medications for prescribers.
Medicare Part D has placed several different players in the process of obtaining prescription medications for our senior patients. These players include prescribers, patients, pharmacy providers, prescription plans, and the federal government, which includes the Centers for Medicare & Medicaid Services (CMS). Each player has different incentives and motivating factors that are important to understand. In addition, the environment is changing in such a way that the strength of each party in ensuring that the prescription gets filled is shifting.
PRESCRIBERS
Historically, prescribers have had the final word in what gets dispensed to patients. Decisions are based on the practice of medicine dictating the best medication on a clinical basis, but are also based, to some degree, on personal preference. Physicians would write a prescription and assume that it would be filled. As a direct result of Medicare Part D, this has shifted to other groups having a much greater say in what medication gets dispensed. In fact, the role of the physician in directing the specific medication that is dispensed has been decreasing, and is likely to continue to decrease in prominence.
PATIENTS
The patient or responsible party makes decisions on which medications are dispensed on the basis of value judgments. This means that when a patient or responsible party is faced with a coverage decision for a specific medication, the decision is between that medication and a less expensive equivalent medication, if available within the formulary. If the patient or responsible party does not see the value in paying for the branded prescription over the less expensive alternative, then the medication is changed from what the physician had ordered. In long-term care (LTC) facilities, the patient is oftentimes unable to pay for certain ordered medications, so it then falls upon the facility to act as the responsible party to cover the cost of the medication to assure that an ordered medication is made available in a timely manner. This situation became more prevalent as a result of Medicare taking the place of Medicaid for the dually eligible. As a result of the more restrictive Medicare Part D formularies, these issues will arise much more than they had in the past under Medicaid.
PHARMACY PROVIDERS
Over the years, pharmacy providers have increased in power, having Pharmacy and Therapeutics (P&T) Committees that develop their own formularies. These formularies tend to include those medications felt to be most appropriate for a drug or health plan or for a health facility. Now with the introduction of Medicare Part D, prescription drug plans have power over the pharmacy providers to ensure that their formularies are all-controlling. The CMS has been pushing down the ability of pharmacy providers, and especially LTC pharmacy providers, to direct which products are preferred within a formulary and therefore are subsequently dispensed. By calling into question rebates provided by pharmaceutical companies, and thus mandating that all rebates be reported to and taken into account by prescription plans so that said rebates reach the Medicare beneficiary, CMS has shifted the market power to some degree away from LTC pharmacy providers.
PRESCRIPTION PLANS
With the implementation of Medicare Part D, prescription drug plans have a responsibility to assure that all medically necessary prescriptions are available, while at the same time fulfilling their responsibility to their shareholders to ensure profitability. This has resulted in prescription plans aggressively using utilization tools such as prior authorization, step therapy, and quantity limits, and drug tiering to direct access to preferred agents. These forces may prove to be much more powerful than a physician’s pen in obtaining specific medications. As a result of these incentives and pharmacy management tools, prescription plans will be a more powerful entity in this process of controlling who directs which prescription to be dispensed.
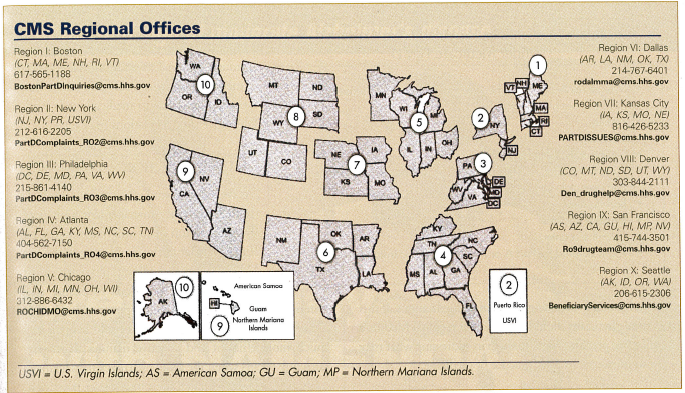
While some of these utilization management tools being used by prescription plans will result in improved medication use, others may represent inappropriate barriers to access medications. Unfortunately, prescription plans are siloed in being responsible only for direct medication costs; as a result, their incentive is to drive toward less utilization—rather than for overall improvement in care. Their incentives should not drive them to implement barriers to accessing appropriate medications. If this occurs, physicians should turn to their regional Medicare office (see previous page) for help in addressing what may be an intrusion on their practice of medicine.
FEDERAL GOVERNMENT
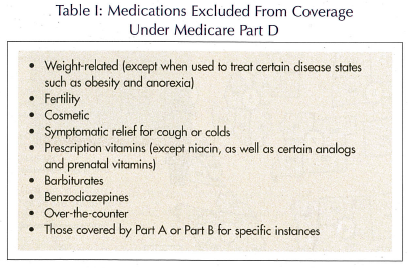
The federal government, including the CMS, has an ability to dictate what the standard minimum formulary recommendations need to be. This has resulted in some products 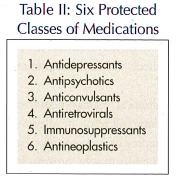 having forced inclusion on a Medicare Part D formulary, while others have been excluded. The federal government applied a list of medications that are excluded from being covered under Medicare Part D (Table I), while at the same time mandating that plans substantially cover all the medications in six classes listed in Table II. This results in the federal government, either through legislation or CMS’s regulations, having a primary role in the determination of access to certain drugs within Part D plans. Changes in this area can only occur through political pressure being applied through national associations such as the American Geriatrics Society to assure that appropriate access to medications is available, given the regulations in effect.
having forced inclusion on a Medicare Part D formulary, while others have been excluded. The federal government applied a list of medications that are excluded from being covered under Medicare Part D (Table I), while at the same time mandating that plans substantially cover all the medications in six classes listed in Table II. This results in the federal government, either through legislation or CMS’s regulations, having a primary role in the determination of access to certain drugs within Part D plans. Changes in this area can only occur through political pressure being applied through national associations such as the American Geriatrics Society to assure that appropriate access to medications is available, given the regulations in effect.
FUTURE DIRECTION
As we move toward ePrescribing, it is likely that pharmacy management tools used by prescription plans will become stricter. Envision that at the time a prescription is written, the prescribing physician must answer specific questions to ensure that criteria dictated by the prescription plan are met before a medication can be dispensed. This could happen in a much more efficient and effective manner than what currently occurs when the same pharmacy management tools are applied well after the prescription is written. Through ePrescribing, prescription plans will have a much greater influence than they do today in the determination of the specific medication that is dispensed. Physicians—especially those caring for older adults within LTC facilities—will need to become very involved in this evolving process to assure that physicians maintain their role in the practice of medicine, and to ensure that prescribing does not move inappropriately beyond them to untrained administrators who may not have the same motivation to deliver high quality and effective medical care. Physicians can do this by being active in prescription drug plan P&T Committees, as well as by developing collaborative relationships with consultant pharmacists to ensure that all medically necessary prescriptions are available to all older adults, and especially to the frail elderly who reside in LTC facilities.
Please send any questions or experiences about Medicare Part D you would like to share with readers to: BSpivack@Waveny.org










