Chronic Ischemic, Venous, and Neuropathic Ulcers in Long-Term Care
OVERVIEW
Lower-extremity ulcers deriving from ischemia, venous, and neuropathic disease are common conditions in long-term care (LTC). Eighteen percent of adults over the age of 40 possess either ischemic disease or neuropathic disease; this prevalance doubles in residents with diabetes.1 Older residents are at higher risk for ulceration, osteomyelitis, and amputation.2 Management of lower-extremity ulcers in LTC requires different considerations than those in a hospital or ambulatory setting, since frailty and functional status typically is more of a concern in LTC. Patient compliance, comorbid medical problems, and nutrition issues are important components of providing adequate wound care for older adults. Nursing care in LTC provides better compliance with very specific and often complicated wound care management.
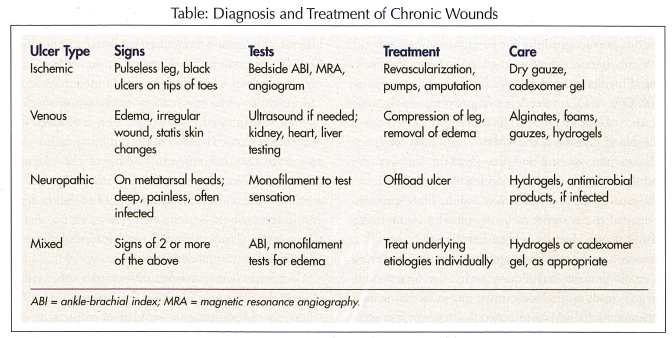
The three commonly encountered types of lower-extremity ulcers in LTC are ischemic, venous, and neuropathic ulcers. There can also be a mix of two or more of these ulcer etiologies. This review emphasizes the specific management of these unique ulcers including diagnosis, wound management, and definitive medical or surgical treatment (Table). Some issues of care such as proper nutrition, nicotine cessation, and appropriate control of diabetes are similar. The health care provider must make the appropriate diagnosis and specific treatment plan, and should avoid placing nonhealing ulcers into a diagnosis of a pressure ulcer by default.3 Despite support by nursing staff and attention to wound care, residents often heal slowly, with some ulcers never healing. Residents often possess multiple comorbid illnesses, marked functional decline, cognitive issues, and nutrition issues that thwart appropriate wound healing. Nursing time and support are instrumental to successful wound healing, with increased direct nursing time improving wound healing.4 Infection is always a risk with chronic ulcers, and particularly so in long-term care. Residents may be at risk of infection with resistant organisms from the hospital or LTC facility.
There are other sources of lower-extremity ulcers in LTC. If an ulcer does not heal or does not appear to be one of the common types of ulcers, providers should consider other etiologies. Skin cancer can arise in the extremity and can behave like any of the above ulcers. If a resident has an ulcer that does not heal, a biopsy might be in order if it has an unusual appearance or if it is in an unusual location. Small-vessel ulcers (from rheumatoid arthritis or autoimmune illness) can occur, but are much less common than other types of ulcers.5
ISCHEMIC WOUNDS
Ischemic ulcers result from peripheral vascular disease (PVD) in the extremities. While these ulcers typically present in the lower extremities, they can also appear in the upper extremities. More than half of residents in LTC may have moderate-to-severe degrees of PVD, as measured by the ankle-brachial index (ABI) test.6 Residents with PVD develop ulcers resulting from either embolic events or thrombosis from atherosclerosis. Embolic ischemic ulcers present as “blue toes” in residents at risk for an embolic event.7 Residents with thrombosis are most at risk for having ischemic disease, and those with vascular risk factors such as a history of smoking, hypertension, diabetes and hyperlipidemia also face risk.8 Residents with PVD and thrombosis develop initial ulcers as a result of trauma, infection, or injury. In wheelchair-based residents, the risk of trauma can be particularly serious. Foot care is important for all residents with known PVD, and some type of foot protection should be used at all times.
Health care providers typically diagnose ischemic wound disease based on a history of vascular disease and the appearance of the ulcer. LTC residents with ischemic disease often experience cold feet and claudication with walking. Residents with ischemic ulcers often have severe vascular disease, and experience rest pain and pain around the ulcer.3 The signs of ischemic disease include dependent redness in the foot that turns pale with elevation. Providers can feel a cold extremity without pulses. The ischemic wound typically starts in the tips of the toes. It can also present on the heel in mixed ulcers with a pressure component, or in any location of the foot or leg with trauma. The ulcer often appears black and necrotic. Providers may smell an odor, depending upon the presence of an underlying infection. The combination of both the appearance and the presence of ischemic disease often lead to a clinical diagnosis of ischemic ulceration.9
Providers can utilize diagnostic tests to confirm ischemic disease if an intervention is contemplated. The use of diagnostic tests for ischemic ulcers must be made within the context of the wishes of the resident and the overall prognosis. If the resident or the family does not wish to pursue aggressive intervention, such as surgical revascularization, providers may elect to forgo diagnostic tests. Providers can test for PVD at the bedside using the ABI. One calculates the ABI using a sphygmomanometer and a Doppler probe. The provider obtains the systolic blood pressure as the reference, and then compares it against the systolic blood pressure in the dorsalis pedis and the posterior tibial artery using the Doppler probe. The ratio of the lower-extremity systolic blood pressure compared to the upper-extremity blood pressure is the ABI.10 If one observes a value less than 0.7, there is a poor chance of wound healing. Providers can also utilize other noninvasive techniques, such as transcutaneous oxygen readings.11 Noninvasive magnetic resonance angiography (MRA) can be used if surgery or intervention is contemplated. The use of angiography is typically reserved for residents who could potentially undergo revascularization or stenting.
Treatment of ischemic ulcers involves improving blood flow to the lower extremity. Improving flow is the most important aspect of care for LTC residents and other older adults. Providers typically attempt to arrest the progression of ischemic disease by risk factor modification, such as treating hypertension, diabetes, hyperlipidemia, and nicotine dependence. For LTC residents who are typically older and have more functional disabilities, risk factor modification may not have the long-term impact that it does on younger patients. Nonsurgical management of ischemic wounds has included pumps that augment flow into the lower extremity.12 Therapists can use stationary arterial boots to augment blood flow. Residents can also undergo arterial augmentation with portable pumps. While the pumps can be helpful for some, they may also increase pain.
Pharmaceutical management of ischemic disease has been limited. Cilostazol has indications for ischemic pain but not ulceration. Open-label usage of cilostazol has shown some improvement for the treatment of ulcers; however, the trials are small and without control groups.13,14
Providers can seek surgical consultation for ischemic wounds with low arterial flow (ie, low ABI). Angioplasty of the ischemic artery is a option to consider for some residents.15 The two primary measures of surgical intervention include revascularization and amputation. One should consider revascularization in order to salvage the limb in a resident with good functional status. One might consider amputation for those wounds that do not heal in residents who are not candidates for revascularization. The level of the amputation must be at a level that can support healing of the surgical wound. Decisions on revascularization or amputation must be made with the functional status of the resident in mind and should be done early in the process. Early intervention allows adequate time for rehabilitation and can prevent some deconditioning.
Care for ischemic wounds differs from other types of wounds. The use of moisture (eg, hydrogels, normal saline) should typically be avoided in most ischemic wounds.3 Providers should ensure an environment that will decrease the risk of infection. The use of cadexomer iodine gel around wound edges is a potential option. Often, the wound is allowed to remain dry with a dry gauze to keep it protected. The use of antibacterial agents (eg, low-concentration acetic acid, Dakin’s solution, topical antibiotics) should be used only in select circumstances, such as a deep wound. Topical antimicrobial agents (eg, bacitracin, triple antibiotic ointment) can be cytotoxic to cells, and should be used sparingly.16
VENOUS WOUNDS
Venous wounds are frequently encountered in ambulatory residents in LTC.17 Residents with venous wounds often have peripheral edema, which is the source of the ulcer. This edema can stem from venous insufficiency, medications, or organ dysfunction (ie, heart, liver, and kidney). The fluid resulting from the swelling causes relative ischemia to the skin by compressing the capillaries. The edema often presents in the lower extremity and worsens as the day progresses. Some residents who sit a great deal or are wheelchair-based may also have dependent edema. A provider who finds edema surrounding a wound should consider a venous wound, and treat as such.
Providers often diagnose venous wounds on a clinical basis. The symptoms and signs of venous ulcers have a recurrent pattern of arising in the same location around areas of edema in the lower leg. Pigmentation changes can be seen in the skin, and the borders of venous ulcers appear irregular, with multiple ulcers in the same region. Providers often see a large amount of exudate resulting from edema. While residents experience pain with venous ulcers, it is often less painful than ischemic or small-vessel ulcers. Diagnostic tests are usually not required for venous disease and ulceration. If required, impedance plethysmography or venous ultrasound can be performed to evaluate possible venous insufficiency.3 If applicable, other sources of the edema such as renal, cardiac, and/or hepatic disease should be evaluated.
Proper control of edema enables adequate healing of venous ulcers and aids rapid recovery. Before providers initiate aggressive edema control, they should evaluate for possible ischemic disease by either examination or testing, if needed. Assuming the arterial flow is adequate, edema control can be initiated by using lifestyle modification, compression devices, and medication.18 Dietary modification includes salt reduction, while avoiding unintentional weight loss. A second lifestyle modification includes the resident elevating the limb, which helps with mild disease. The resident should strive for elevation of the limb 30 minutes 2-3 times per day. Deconditioning can be one of the worst sequela of limb elevation. It is important to keep the resident active and ambulatory despite the edema. Pharmacological therapy involves the use of diuretics in judicious doses, which can reduce leg edema.19 This should be used as a last step for edema management for residents in LTC. Discontinuing medications that cause edema (eg, calcium blockers, thiazolidinediones, nonsteroidal anti-inflammatory drugs [NSAIDs], COX-2 inhibitors) may be another consideration.
The use of compression garments provides the most practical method of edema control. The use of constant pressure is often needed to reduce edema and to help heal a venous ulcer.20 With an active venous ulcer, providers should institute use of compression wraps to the extremity. Either a single wrap or multilayer wraps can reduce edema. Compression wraps conform to the individual leg and accommodate the wound dressings. A triple-layer compression wrap uses three layers to improve compression, and can be used in combination with compression hose for excellent edema control.21 The practical limitations residents face would be comfort and compliance of compression. Frail residents may have difficulty putting the hose on, and staff may have difficulty with noncompliant residents. Residents may also feel uncomfortable or hot in compression hose. The use of antiembolic stockings or support hose provides little compression, and is thought to be inadequate for the task of preventing future ulcers.
Wound care for venous ulcers controls the moisture from the exudate. Residents often experience a significant amount of drainage from the venous wound. Without adequate control of the moisture, maceration and enlargement of the wound can occur. Wound products should absorb the excess fluid. Foams and alginate dressings absorb a considerable amount of moisture, and both effectively absorb the excess exudate and avoid maceration. Gauze can be used but must be changed frequently. Hydrocolloid dressings often can be overwhelmed with the exudate in venous wounds. Hydrogels in small amounts can be used. There is current debate about the utility of advanced products over conventional products for wound care in venous wounds.22
NEUROPATHIC WOUNDS
Neuropathic wounds, known as diabetic foot ulcers, are often one of the most debilitating illnesses that providers encounter in LTC. Neuropathic wounds develop as a result of peripheral neuropathy from diabetes or idiopathic causes. In the Medicare population, the costs of caring for lower-extremity ulcers is threefold higher than in residents without ulcers.23 The resident with neuropathy lacks awareness of pressure points in the feet. Paresthesias over specific points of high pressure can lead to ischemia. These pressure points typically occur on the metatarsal heads of the feet.3 Providers can diagnose neuropathic ulcers with only a history and examination. Many residents will report previous ulcers and amputations. The ulcer itself will typically be painless.24 The resident or caregiver may also report symptoms of infection (eg, odor, fever, chills, symptoms of sepsis). Providers will note the location of the ulcer on the metatarsal heads or on a pressure point of the foot. Providers should probe the depth of the ulcer with a sterile instrument. Providers can find underlying pockets of infection (“undermining”), or possibly the presence of osteomyelitis if bone is palpated.25 The presence of neuropathy can be determined with monofilament testing at the beside.26 The presence of comorbid vascular disease in individuals with diabetes is common, and vascular status of the resident should be determined as well.
Neuropathic wounds are often infected, which presents a concern for osteomyelitis. Osteomyelitis can occur with any lower-extremity ulcer; however, it has a high predisposition for neuropathic ulcers. The ongoing relative ischemia from pressure, as well as the lack of sensation or pain, often enables an infection to progress to a higher stage than in other ulcer types.27 The location of the neuropathic ulcer often precludes direct inspection by the resident. The nursing staff or the personal care attendants can look directly at the wound, and hopefully detect a neuropathic ulcer at an early stage of infection. This potential advantage in LTC is counterbalanced with antibiotic-resistant organisms (eg, gram-negative, staphylococcus aureus, and vancomycin-resistant enterococcus). It is important when treating an osteomyelitis or cellulitis in the facility to see improvement in the wound infection.
Adequate pressure reduction is an essential component for healing of a neuropathic ulcer.28 The use of specific wound shoes to offload the metatarsal heads can be very useful to reduce pressure and ensure healing. Crutches can completely offload the foot but are not practical in frail residents. Total contact casting may be beneficial for some highly functional residents.29 Removable cast walkers help to offload the metatarsal heads and can be removed at night. However, these walkers are heavy and bulky, and so could potentially be a fall risk for residents with strength or balance problems. If the resident restricts ambulation, one might observe deconditioning. The provider must balance the risks of deconditioning or falls with the need to heal the neuropathic ulcer. Residents with cognitive impairment may not be compliant with using a wound shoe or staying off of the wound.
Topical wound treatment should focus on hydrating and packing the wound. For an infected wound, dressings with antimicrobial properties are often used, as mentioned previously.3 These should be used for a short time period. It is important to completely pack the wound and to pack any type of undermining or tunneling. Occasionally, stimulating agents such as collagen can be used.30 Becaplermin gel (recombinant platelet-derived growth factor) is also used for diabetic neuropathic ulcers in patients with adequate blood flow.31 Proper hydration with saline or a hydrogel on gauze is another good option.
MIXED LOWER-EXTREMITY ULCERS
Often, older residents can have lower-extremity ulcers with mixed etiologies. The risk factors of ischemic, neuropathic, and venous ulcers overlap to some degree (particularly in diabetes). Thus, one could have a neuropathic ulcer with an overlying ischemic ulcer component. Or a resident with ischemic heart failure may have a venous ulcer and have vascular disease of the legs compromising the ulcer. In cases of mixed ulcers of the lower extremities, it is important to treat all of the underlying components with the largest emphasis on restoring arterial flow in cases of ischemia. Growth factors have been used in mixed ulcers in case reports32; however, specific treatment recommendations are often lacking. Wound care should emphasize the primary ulcer component or the appearance of the ulcer. It is important to recognize the role of each of the components in a chronic ulcer.
CONCLUSION
Lower-extremity wounds in long-term care are challenging and unique medical problems with a specific method of care. The ulcers of some residents will not heal, and a frank discussion of amputation is often warranted. Some residents will elect to forgo invasive treatment or amputation, and are often treated in a palliative mode without the goal of wound healing. The functional status of the resident and staffing limitations at the facility should factor strongly into all wound treatment plans for residents. In all situations, providers should institute appropriate wound-specific care and adequate pain control. The author reports no relevant financial relationships.










