Atypical Neuropsychiatric Symptoms in the Elderly
INTRODUCTION
Neurologic and psychiatric symptoms are common in geriatric patients, as exemplified by depression and dementia, which affect 10-15%1 and 6%2 of elderly persons, respectively. Often, such symptoms will represent primary neurologic or psychiatric syndromes, but clinicians must be aware that neuropsychiatric symptoms may also be secondary to other medical illnesses, medications, or metabolic abnormalities, and may present in varied and unusual ways.
This article examines atypical neuropsychiatric symptoms that are secondary to medical or other causes. Our goal is to introduce the clinician to several causes of such symptoms, and to reinforce the principle that when neuropsychiatric symptoms emerge in the elderly, it is clinically imperative that a wide differential diagnosis be considered in symptom evaluation. Five cases are presented here that exemplify the evaluation of medication side effects, psychosis, movement disorders, depression, and anxiety in the elderly person.
Case 1: A Patient Presenting with Restlessness
An 82-year-old female nursing home resident with a history of osteoarthritis, coronary artery disease, and mild cognitive impairment developed a depressive syndrome marked by sadness, tearfulness, insomnia, and decreased appetite. She was diagnosed with major depression and started on a selective serotonin reuptake inhibitor (SSRI). Within a week she became restless, frantically pacing the halls of the facility. She could not sit still for meals, her insomnia worsened, and she developed a fine tremor. She was diagnosed with agitated depression, and the SSRI dose was increased, further exacerbating her agitation and restlessness. The SSRI was discontinued, with improvement in the restlessness, but the other depression symptoms persisted. A medication-induced akathisia was diagnosed. Mirtazapine was prescribed to treat the depressive disorder, and the symptoms began to lift after 3 weeks.
MEDICATION SIDE EFFECTS
Medication side effects can result in neuropsychiatric symptoms such as motor restlessnesss, tremor, anxiety, sedation, and psychosis, among many other symptoms. Whenever such symptoms present, temporal relationships between the symptoms and medication changes (both psychotropic and nonpsychotropic) should be explored. Added medications can either cause a symptom directly, as in this case example, or can lead to metabolic changes or drug-drug interaction, which may in turn lead to behavioral changes. Examples of this would be an SSRI causing electrolyte changes, which in turn could cause restlessness or delirium, or a mood stabilizer altering the metabolism of digitalis, resulting in confusion and cognitive changes due to digitalis toxicity. Because elderly patients are more prone to cognitive and other medication side effects, low initial dosing and slower titration should be considered in initiating any psychotropic medications whenever possible.
Case 2: A Patient Presenting with Psychosis
A 68-year-old female with no previous psychiatric history, who had recently sold her business, began to develop bilateral lower-extremity numbness, tingling, and pain. Evaluation revealed a sensory peripheral neuropathy, and she was given oxycodone for pain. Relief was not obtained, and a fentanyl patch was added. She developed visual hallucinations of her recently deceased dog and of a man pacing in her room. She accused her husband of infidelity with a 28-year-old woman, and she became increasingly irritable and belligerent. Psychiatric consultation was requested.
PSYCHOSIS
Psychosis in the elderly is common, but can present in unusual ways, often heralding an underlying medical condition. Surveys have found that 4% of elderly persons living in communities suffer with delusional thinking, 21% admitted to a nursing home have delusions, and up to one-third of persons with Alzheimer’s disease develop paranoid delusions.3 The presentation of psychosis associated with such primary psychiatric disorders as schizophrenia and psychotic depression in the elderly can be similar to the presentation of psychosis in younger people; this may include abnormalities of thought form (blocking, tangentiality) and thought content (perceptual distortions, delusions, or hallucinations). The context and course of the psychosis may differ in older versus younger people, however.
In older individuals, primary psychotic disorders are more common in women (especially after menopause), there are fewer cognitive deficits and negative symptoms, and they may require lower doses of antipsychotic medications.4 Biological changes in elderly people with psychosis have been noted, although specific changes vary depending on the source of the psychotic symptoms. Brain volume changes documented with magnetic resonance imaging (MRI) and positron emission tomography (PET) imaging, and differences in dopamine receptor numbers have all been reported.5
Although psychotic symptoms in the elderly can be the result of late-onset schizophrenia, psychotic depression, or delusional disorder, they are more likely to be the result of underlying medical or neurologic conditions or concurrent medications. Presentations of secondary psychosis can be similar to primary psychosis; however, there are features that, if present, may help distinguish between primary and secondary psychosis. These include frequent visual hallucinations; more concrete or perseverative thought processes, rather than loose associations and idiosyncratic language; cognitive impairment; and presence of medical and neurologic signs and symptoms.6
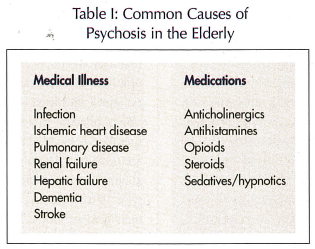 Medical and neurologic conditions associated with development of psychosis in the elderly are many and include infection (UTI, pneumonia, sepsis), cardiac disease (especially acute ischemia), pulmonary disease, renal or hepatic failure, and endocrine abnormalities, including cortisol or thyroid dysfunction (Table I). Neurologic abnormalities associated with psychosis include dementia, tumor, seizure disorders, cerebral vasculitis, infectious encephalitis, paraneoplastic encephalitis, or Huntington’s disease. Many medications are associated with psychosis, the most common including agents with dopaminergic or sympathomimetic activity, anticholinergic or antihistaminergic side effects, opioid analgesics, anti-inflammatory agents including steroids, and sedative hypnotics including alcohol and benzodiazepines.
Medical and neurologic conditions associated with development of psychosis in the elderly are many and include infection (UTI, pneumonia, sepsis), cardiac disease (especially acute ischemia), pulmonary disease, renal or hepatic failure, and endocrine abnormalities, including cortisol or thyroid dysfunction (Table I). Neurologic abnormalities associated with psychosis include dementia, tumor, seizure disorders, cerebral vasculitis, infectious encephalitis, paraneoplastic encephalitis, or Huntington’s disease. Many medications are associated with psychosis, the most common including agents with dopaminergic or sympathomimetic activity, anticholinergic or antihistaminergic side effects, opioid analgesics, anti-inflammatory agents including steroids, and sedative hypnotics including alcohol and benzodiazepines.
The psychotic symptoms in this 68-year-old female began in the context of an evolving neurologic disorder and were aggravated by the use of opioid analgesics. The presence of cerebrospinal fluid (CSF) markers for paraneoplastic syndrome led to further investigation and eventual diagnosis of small cell lung carcinoma that was not seen on a screening chest x-ray. Surgical excision of the lung cancer, decreased opioid analgesics, and low-dose antipsychotic medications led to resolution of her psychotic symptoms. This case highlights the complexity involved with the recognition and evaluation of psychosis in the elderly, which, in addition to primary psychiatric disorders, should include full medical, neurologic, and medication assessment.
Case 3: A Patient Presenting with Abnormal Movements
A 66-year-old right-handed male with a 5-year history of progressive cognitive decline and worsening hyperkinetic movements of 1-year duration presented to the emergency department actively suicidal with a plan of “throwing himself into the wood chopper.” A few months prior, there was worsening perseveration and hyperphagia, delusions, verbal aggression, and repeated suicidal comments. He developed delusions of being “the skinniest person in the world” (weight, 104 kg), and ate constantly, despite difficulty swallowing. Associated symptoms included gait difficulties, generalized weakness, and slurring of speech. Except for two episodes of head trauma in the remote past, his medical history was unremarkable. Family history was significant for Alzheimer’s disease in his mother. On examination, he had brief, jerky, purposeless movements of the head, limbs, and trunk that were involuntary and unsuppressible, mild symmetric rigidity, and upgoing left toe. He perseverated in asking for food. Mood was irritable, affect blunted, thought process tangential, and memory and concentration impaired. His Folstein Mini-Mental State Examination score was 17 out of 30. He endorsed suicidal ideations.
Laboratory evaluation did not reveal any tumors or any metabolic, infectious, toxic, immunological, or vascular causes. An MRI of the brain showed bilateral frontal and anterior temporal atrophy, atrophy of both caudate heads, and diffuse cerebral and cerebellar atrophy. A genetics consultation was requested, and formal genetic testing was performed, revealing the presence of IT15 CAG repeat expansion consistent with Huntington’s disease.
ABNORMAL MOVEMENTS
Abnormal movements in the elderly occur in a wide variety of CNS disorders, neurodegenerative disorders, and systemic conditions. Neuropsychiatric features may occur early or late in the course of the disorder. Abnormal movements may be broadly divided into hypokinetic and hyperkinetic disorders.
Hypokinetic disorders are characterized by reduction or lack of motor activity or increased muscle tone. Parkinson’s disease is the prototype, but a number of other conditions with different etiologies share its parkinsonian features (bradykinesia, rigidity, tremor, postural impairment). Conditions with “parkinsonism” include progressive supranuclear palsy, multiple system atrophy, spinocerebellar degeneration, corticobasal degeneration, parkinsonism-dementia syndromes, and others caused by drugs, toxins, or trauma. Hyperkinetic disorders are characterized by excessive involuntary movements (dyskinesia), such as tremor, chorea, dystonia, myoclonus, or tics.7-9 (It is beyond the scope of this section to discuss movement disorders comprehensively; the goal is to provide a general overview through a case presentation of how to approach a person with underlying abnormal movement presenting with psychiatric symptoms.)
The evaluation of a person presenting with abnormal movements includes a careful history of the course of illness, detailed medication history and family history, and a thorough physical and neurologic examination. Collateral information from caregivers or family members is essential in establishing the chronology and accuracy of symptoms. After identifying the type of abnormal movement, the next step is classifying the type of dyskinesia. The subsequent evaluation and management should be guided by the differential diagnoses and clinical indication.
In the case described, the excess unwanted movements can be classified as hyperkinetic and choreiform. Among the hyperkinetic disorders, there is no evidence from the history or physical examination to suggest myoclonus, tremors, or dystonia. Differential diagnoses for choreiform movements are numerous, but the most frequently encountered types in psychiatric practice are Huntington’s disease and tardive dyskinesia (TD). TD is unlikely since there is no prior psychiatric history or neuroleptic use. Other causes of chorea include drugs (neuroleptics, metoclopramide, antiparkinsonian drugs, amphetamines), metabolic conditions (thyroid dysfunction, electrolyte and glucose abnormalities, Wilson’s disease), infections (encephalitides, Creutzfeldt-Jakob disease [CJD]), toxins (alcohol, heavy metals), immunological, vascular, tumors, or trauma.
There is a history of head trauma in this patient, although its occurrence in the remote past makes it an unlikely etiology for his current symptoms. The choreiform movements, in combination with the mood changes, abnormalities in thought process, existing cognitive impairment, and significant neurologic findings, suggest an underlying neurodegenerative disorder. His clinical features are suspicious for Huntington’s disease, although there is no family history.
Case 4: A Patient Presenting with Depression Symptoms
A 76-year-old man was referred for psychiatric evaluation of depressive symptoms. Usually gregarious, he gradually had become more withdrawn and preferred to stay at home rather than socialize. His sleep pattern had become somewhat disrupted. He couldn’t concentrate on books or television for very long, and his wife saw him as being needier. He denied feeling depressed and had not been tearful. Although more forgetful, he greatly enjoyed visits from his grandchildren. Several trials of antidepressants had had no effect upon the symptoms. Neuropsychological testing revealed difficulties in several cognitive spheres consistent with early Alzheimer’s dementia.
DEPRESSION
The hallmark features of major depression are depressed mood, anhedonia, weight changes, sleep changes, psychomotor agitation, decreased energy, feelings of worthlessness, decreased concentration, and suicidal ideation.11 Symptoms of anxiety are also common in older persons with depression. Many medical illnesses are associated with an increased incidence of depression, and many syndromes may present with depression-like symptoms, but are not depression at all.
Disentangling this conundrum may seem like the proverbial “chicken and egg” problem, but it is important in the overall approach to depressive symptoms, as Case 4 illustrates. Whenever first-episode depressions or an atypical pattern of depressive symptoms occur in the elderly, it is imperative that underlying medical etiologies be explored, and that a thorough medical evaluation take place to rule out other causes of the depressive symptoms.
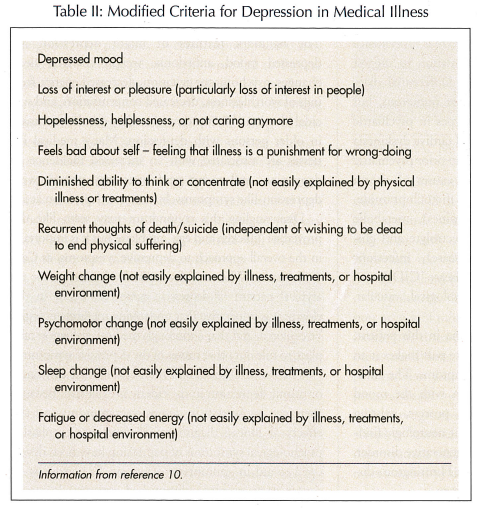
The list of illnesses and medications that can cause or mimic depression in the elderly is extensive. Because there can be overlap in depressive symptoms and the effects of illness, diagnostic schemes that emphasize psychological symptoms of depression have been developed to aid in appropriate diagnosis. In persons with cancer, as an example, diminished appetite, decreased energy, and sleep changes are common but may not represent a depressive disorder. Emphasizing symptoms of social withdrawal, self-pity, pessimism, and suicidal thinking may lead to better diagnostic accuracy in such patients (Table II). Thus, understanding the symptoms of a particular medical illness, the symptoms of depression, and the effect that these may have in a patient are critical in appropriately diagnosing depressive illnesses in the geriatric population. In this case example, the patient’s “depressive” symptoms were better explained on the basis of an evolving dementia, rather than a primary depressive disorder.
Case 5: A Patient Presenting with Anxiety
Symptoms A 68-year-old female with a history of asthma and allergies presented with shortness of breath and anxiety to an outpatient clinic during hayfever season. Pulmonary function tests (PFTs) were consistent with an asthma exacerbation, and she was treated with beta-agonist inhalers and a course of oral steroids. Her PFTs improved, but she continued to feel quite anxious, “jittery,” and tremulous, especially after using her inhalers.
ANXIETY
Anxiety can be defined as a subjective state of fear or apprehension, and is often accompanied by symptoms of autonomic activation. In physiologic terms, the “fight or flight” sensation of anxiety may be driven as a direct response to environmental stimuli, a physiologic response to illness or medication, or may represent a primary anxiety disorder itself. Anxiety symptoms can be viewed as labile or overactive autonomic nervous system activity and can be driven by a multitude of factors.12
New-onset anxiety symptoms in the elderly frequently herald a depressive episode but, as in first-episode depression in the elderly, must be considered the diagnosis of exclusion until other etiologies are examined.
The medical evaluation of new-onset anxiety in the elderly should be geared toward elucidating potential causes of increased autonomic activity. As in this case example, the hypercarbia and hypoxia associated with an exacerbation of chronic obstructive pulmonary disease (COPD) would be expected to result in the potential anxiety symptoms of tachypnea, tachycardia, lightheadedness, and an overwhelming sensation of anxiety.
Treating the anxiety symptoms alone without addressing the underlying medical problem can be fruitless at best, or dangerous at worst, if potential serious medical problems are the driving force behind heightened anxiety. Complicating this picture is the fact that many treatments themselves cause or exacerbate anxiety symptoms, and it is important to explore temporal relationships between onset of therapies and anxiety symptoms. In Case 5, the COPD exacerbation may have caused anxiety symptoms, but so could the selected treatments. The beta agonist properties of an inhaler or the effects of oral prednisone might also serve to exacerbate the anxiety symptoms the patient was experiencing. Thus, physicians need to be aware of the potential anxiety-provoking side effects that medications may induce.
SUMMARY
New-onset neuropsychiatric symptoms are common in the elderly. Whenever such symptoms emerge, a wide differential diagnosis needs to be considered, and a thorough evaluation is necessary to elucidate the cause. Whenever possible, treatments should be aimed at underlying causes, rather than simply targeting symptoms alone.
The authors report no relevant financial relationships.









