Falling into Place: A Practical Approach to Interdisciplinary Education on Falls Prevention in Long-Term Care
INTRODUCTION
Accidental falls are the sixth leading cause of death in people over age 65. The rate of falls is roughly 30-40% for those over age 65 living in the community.1 However, rates are significantly higher for people over age 75, and 50% of people over age 80 fall each year.1 In addition, older adults who are hospitalized or who reside in long-term care (LTC) facilities have a significantly higher rate of falls—at least 1.5 falls per bed per year.2 Roughly one-half of all U.S. nursing home residents fall annually.3
Recently, more attention has been given to this important public health problem. Funding was made available through the National Council on the Aging (NCOA) for a national initiative to increase awareness of the devastating and potentially preventable nature of falls in older adults.4 This has led to the development of national websites and other sources of information to aid the public and providers in preventing injuries related to falls.
Physicians and advanced practitioners are becoming more involved in working with nursing staff on interdisciplinary education in LTC facilities. This partnership enhances and enriches education by bringing nurses, nursing assistants, and primary care providers closer together, and by presenting a consistent, inclusive message about falls prevention to all staff. This special article provides physicians and advanced practitioners with some selected resources and references on educational content that should be considered, at a minimum, for LTC falls prevention. (It does not review all the components of effective falls prevention programs and policies, which can be found in several review articles referenced here.) In addition, specific evidence-based teaching strategies that primary care providers can use in an interdisciplinary nursing home practice are suggested.
REVIEW OF THE LITERATURE
A number of review articles on nursing home falls prevention have been published over the past several years.5-13 In addition, specific efforts to study the effectiveness of various educational programs in LTC have been described.3,14,15 Despite ongoing education, the ability to prevent falls in the LTC setting may be limited at times, due to the complex nature of the resident population and the high number of nonmodifiable risk factors.7
Facility-based falls prevention programs are described in the nursing literature that focus on a quality improvement or systems approach,16 but not on the actual content of and methodology for education on this topic.17,18 Proprietary companies specializing in LTC education and staff development have designed programs on falls prevention; however these entrepreneurial companies often market more expensive products, which may not be affordable or available to nursing homes with fewer staff development resources. Following is a discussion of selected evidence-based topics related to falls prevention in LTC, and recommendations for content and teaching strategies for falls prevention education programs.
RISK FACTORS
Risk factors for falls are generally broken down into intrinsic and extrinsic categories (Table I). Intrinsic risk factors are those related to the individual faller, such as disease states, changes associated with aging, and medications. Extrinsic risk factors are hazards associated with the environment or type of activity. Both are important in nursing home residents, as this population tends to have more intrinsic risk factors; yet they are also more sensitive to environmental risk, and potentially less able to resist external hazards. Overall, research suggests that focusing on intrinsic risk factors is useful in preventing falls in this population.2
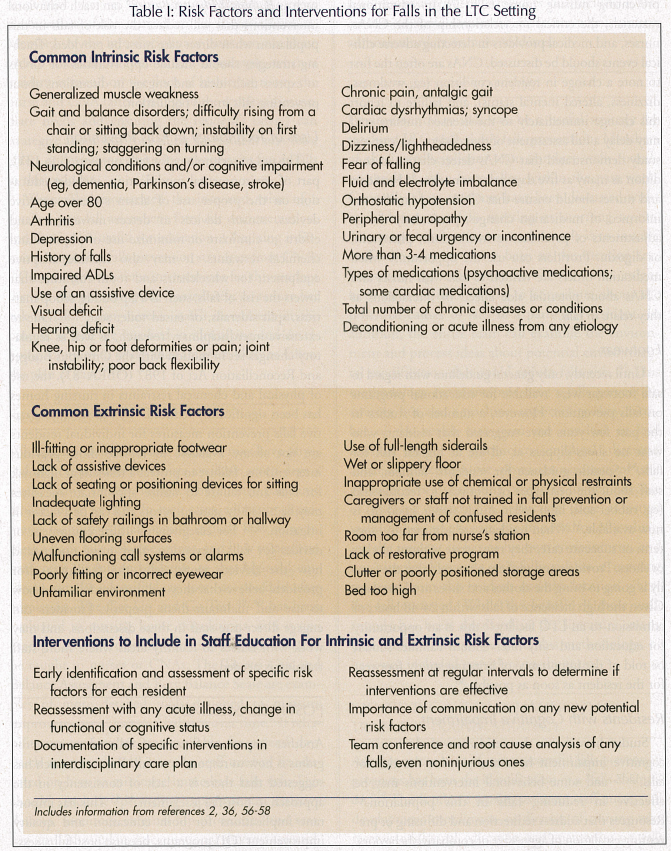
An important component of risk factor education is emphasizing the multifactorial nature of falls prevention, and the importance of identifying each risk factor so that potentially modifiable ones can be addressed. In LTC, many more risk factors may be nonmodifiable (eg, late-stage Parkinson’s disease, age over 80, prior stroke with dense hemiparesis) compared to potentially modifiable factors in community-dwelling patients (eg, reduced environmental clutter, education about potentially dangerous activities or weather conditions). Nurses and certified nursing assistants (CNAs) may not be aware that one single fall is the best predictor of future falls.19 By increasing awareness of this, LTC residents who have fallen once, even prior to admission to the nursing home, can be targeted for comprehensive care plans and individualized interventions. A complete review of risk factors and increased awareness of the importance of individual risk factor identification and modification for falls will lead to more consistent and timely interventions by staff, behaviors that are critical to reducing injurious falls.
INTERVENTIONS
Exercise Programs
Gait and balance disturbances and generalized weakness have been determined to be major falls risk factors in recent reviews and meta-analyses.2,8,20 While individualized physical therapy is often part of falls prevention, nurses and CNAs also play an important role in providing exercise and restorative care to residents. To date, research on exercise programs in this setting has had limited ability to demonstrate effectiveness of these programs alone.12,21 Some researchers posit that this is due to the multifactorial nature of falls in frail, institutionalized adults, and the inability to conduct randomized, controlled trials that are adequately powered to detect an intervention’s effect.22
Earlier studies demonstrated that strength training increased muscle mass in 90-year-old nursing home residents; yet a relationship between increased muscle mass and reduced falls was not established.23 Nevertheless, many experts agree that specific education for CNAs who are assisting with activities of daily living (ADLs), restorative care, and exercise is essential.24,25 Video instruction for CNAs on how to provide restorative care and exercise to prevent falls is available for purchase from the University of Maryland (www.videopress.org) and other organizations.
Sensory Impairment
The importance of visual assessment and correction for falls prevention has been addressed in several studies.26-30 It is not easy to ensure that a resident has adequate eyewear accessible. Temporary staff can be unaware that a resident requires corrective lenses to see properly and ambulate safely. Challenges also need to be addressed for residents who cannot leave the nursing home for an ophthalmologic examination, or cannot cooperate due to dementia or other cognitive issues. Similar issues exist with regard to hearing aid use. Failure to correct hearing loss is a known risk factor for falls.2
Medication Review
Several evidence-based articles have documented the importance of medication review and adjustment in preventing nursing home falls.17,31 In educational materials, the critical interrelationship of the CNAs, nurses, and medical providers in detecting adverse clinical events should be discussed. CNAs are often the first to note a change in resident condition (eg, weakness, dizziness, altered mental status), and failure to report this change immediately to the licensed nursing staff may delay a full assessment of the resident. At least one study demonstrated that CNAs detect change in condition as many as five days prior to nurses.32 Providers and nurses should ensure that CNAs and families are informed of medication changes, particularly dosage adjustments of psychoactive medications, phenytoin, or digoxin. Providers can use the opportunity when medication orders are written to talk with nurses and CNAs about potential side effects or interactions as they relate to falls.
Footwear
Until recently, only general guidelines with regard to safe footwear were available for educational programs on falls prevention. However, a number of studies in the past few years have suggested that residents who wear no shoes/slippers at all are at highest risk for falls.33 Specific guidance for residents, families, and staff about the best types of footwear to recommend (eg, rubber sole, high collar, sturdy upper, good fit) is now available.34 When residents are admitted to long-term or subacute care, they may arrive without clothes or shoes. Providers and staff are often told that the family is going to bring the clothes and shoes at a later date. Given the high incidence of falls within 24-48 hours of admission to an LTC facility,35 this is an opportunity for education and early intervention. Families should be told of the importance of bringing sturdy footwear for the resident as soon as possible.36
Residents with Cognitive Impairment
Studies have shown that residents with dementia or cognitive impairment have nearly twice the risk for falls,13,37, and some behavioral interventions may be effective in reducing falls in this population.13 Resources that address redirection and diffusing or preventing escalation of aggressive or combative behaviors, such as Bathing Without a Battle,38 can teach behavioral interventions that will reduce the risk of falls in this population when direct care must be provided. Teaching strategies should include opportunities for CNAs to express their ideas and engage in discussions about preventing falls in this population.
Uses of Technology in Falls Prevention
The use of technology for falls prevention in LTC, part of environmental modification, includes education on the proper use of alarm systems, assistive devices, sensor devices to detect movement, and efforts to eliminate or minimize use of physical and chemical restraints. It may also include adaptive equipment for wheelchairs and room furniture that lowers the risk of falls, such as a lap buddy, scoop mattress, split siderails, or raised toilet seat.17,35 Due to extensive interdisciplinary research, as well as regulatory changes set in motion with the Omnibus Budget and Reconciliation Act of 1987 (OBRA ‘87), the use of physical and chemical restraints in nursing homes has been significantly reduced.39,40 However, alternative falls prevention measures for individual residents are not always available to replace those previous interventions. Failure to protect a resident at high risk for falls and failure to utilize appropriate measures may be noted by state surveyors and can be a factor in litigation.41,42 For caregivers to utilize equipment or devices for falls prevention, they must understand how the devices work, why the facility and/or providers believe that they will prevent falls, and how to use and maintain them properly. Providers can engage direct care staff in these discussions, and may work with nurses to identify areas where more staff training is needed.
POST-FALL ASSESSMENT
Another important feature of falls education programs is how to respond to a fall. Recent research has suggested that there is a lack of consistency in the approach to post-fall assessment.43-45 This has important implications for both education and quality improvement (QI) programs, because post-fall assessment may offer an opportunity to detect the most likely causes of the immediate fall in an individual. Members of the interdisciplinary team can use these events as teachable moments. For example, when a resident is found on the floor of his or her room, the nurse and CNA (after tending to the resident’s immediate needs and ensuring the resident’s safety) can strategize about why they think the resident may have fallen, and what interventions may prevent future falls in this resident.
Wagner43 demonstrated the increased value of a detailed post-fall assessment form for documentation, and this is also useful for education. Obtaining information regarding falls prevention strategies from CNAs (“Can you give me three interventions for this resident that we can put into place immediately, to reduce her risk of falls?”) can increase staff’s investment in the process. If staff are involved in identifying and developing solutions to issues, they are more likely to follow the plan of care.46,47
NEW ADMISSIONS
While some skilled nursing facilities may have physical or occupational therapists available seven days a week, many smaller facilities have only part-time rehabilitative services. In such cases, educational programs for nursing staff should include how to complete a basic falls risk assessment, and how to perform basic tests for gait and balance, so that high-risk residents can be identified as soon as possible after admission. The Get Up and Go Test48,49 has been evaluated in nursing home populations, and is one example of a short, standardized assessment that can be taught to nurses or CNAs. The Tinetti Gait and Balance Assessment and Berg Balance Scale are examples of more detailed tools designed to measure improvements in gait and balance over time.6 If rehabilitative services are not available for several days (such as on weekends), nursing staff need to be educated on how to minimize immediate falls risk. This should include providing appropriate assistive devices, monitors, external hip protectors, and seating until physical and occupational therapy can evaluate the new resident. Providers can include a discussion of these important measures when writing admission orders on new residents.
ENVIRONMENTAL ROUNDS
Environmental rounds can be a useful strategy for teaching LTC staff about falls prevention. Members of the interdisciplinary team conduct walk rounds on residents who have fallen within the past week. Generally, these residents have been discussed within 24 hours at a falls meeting or morning report. The purpose of environmental rounds is to involve staff who may not have been at the meeting (eg, housekeeping, maintenance, CNAs) who might have valuable information to contribute about the potential causes of falls in a particular resident. In addition, the entire team can examine the environment and process ideas about potential environmental modification that could reduce falls risk.35 This methodology represents not only a falls prevention strategy but also a teaching opportunity. Any member of the health care team can conduct or lead rounds; often, a physician, medical director, advanced practice nurse, physician assistant, or unit manager acts as attending physician for the purpose of teaching rounds.50 Conducting these as actual walk rounds emphasizes the importance of evaluating the resident in her or his own environment, and not simply discussing the falls risk at a meeting removed from the resident and the location where the fall occurred. While the benefit of these walk rounds has been discussed in the literature, many facilities have not yet adopted this methodology, or have not included providers on the team.
IDENTIFYING A “FALLS CHAMPION” FOR A TRAIN-THE-TRAINER STRATEGY
Another component of some successful falls prevention programs has been the identification of a “falls champion.”18 This is often a nursing assistant, staff nurse, staff development coordinator, or director of nursing who receives additional education and mentoring on falls prevention strategies and leadership skills. This person may be charged with training new staff, overseeing documentation and communication, and continuing to raise awareness about the importance of preventing falls. These key individuals require additional training and support for sustainability of a falls education program.
Typically, the facility identifies an individual who is motivated, has leadership qualities, and is willing to take on this new role. Providers can work with the falls champion by acknowledging the individual’s new role as a resource and advocate for falls safety. When a fall occurs in the facility, the provider can discuss the specifics of that fall with the designated falls champion, who would then be responsible for disseminating any new information to other staff members. Comprehensive programs reviewed by national experts are available, some of which include materials for training a falls champion (Table II).

FROM MULTIDISCIPLINARY TO INTERDISCIPLINARY EDUCATION
While some articles in the literature discuss falls prevention programs as interdisciplinary,51 in many real-life practice situations these programs are actually only multidisciplinary. Clinical practice guidelines may be geared primarily to medical providers, rather than nursing and facility staff. (A notable exception is the American Medical Directors Association [AMDA] Clinical Practice Guideline on Falls and Fall Risk36). Policies and procedures are infrequently reviewed by primary care providers other than by medical directors. Educational programs are geared to either nurses or physicians, and infrequently to nursing assistants. A true appreciation for the interdependence of all LTC team members is needed, with particular attention to teaching communication on resident change in condition, as well as information sharing between disciplines.52 Educational programs should include all facility staff, not just nursing and rehabilitation.
Part of a complete education program is ensuring that there are no assumptions about who is responsible for each aspect of falls prevention—everyone should know who is accountable for each component of the facility’s program. While these are often considered aspects of program and policy implementation, they should be included in educational programs as well. Many programs considered to be educational do not include information on leadership and accountability, even though these can be important influences on resident outcomes such as falls and restraint use.53
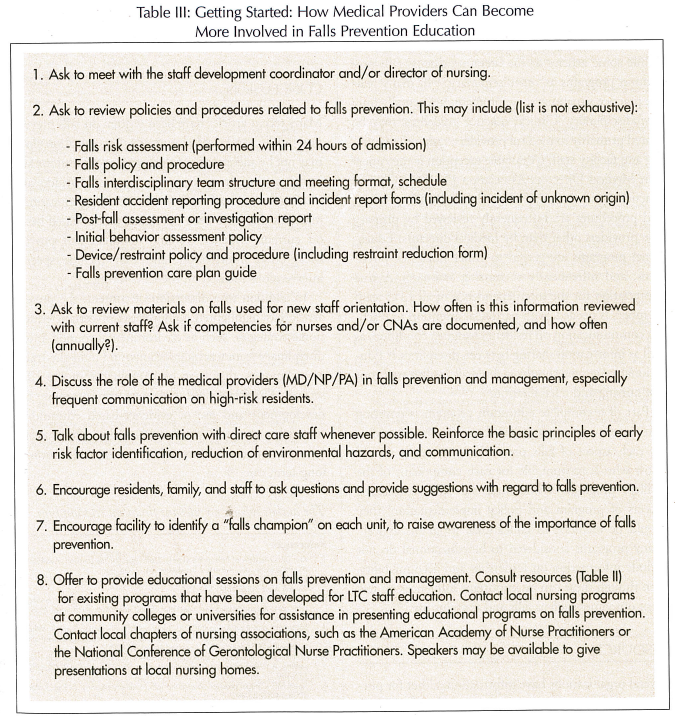
RESOURCES
Several organizations have information, either for purchase or available at no cost, on their websites. Table II includes a selected list of organizations with LTC falls prevention information and resources. Books on falls in older persons by Tideiksaar,54 Lord,55 and others present background material and templates for the development of educational programs and nursing care plans specific to LTC.56-58 Primary care providers and medical directors should become familiar with each facility’s education program, and provide resources and updates as new information becomes available (Table III).
CONCLUSION
Many recent articles have been written on falls prevention in LTC, and research suggests that education alone may not be adequate for reducing rates of injurious falls in this setting. In order to be effective, providers and nursing home staff must have access to educational materials that have been developed and updated based on current evidence. Online resources can provide background information, and may include specific interventions focused on the LTC setting. In addition to a discussion of content, the present article has highlighted components of certain educational strategies, such as environmental rounds, interdisciplinary team teaching sessions, and train-the-trainer techniques, that have been evaluated in the LTC setting. Physicians and providers can promote the development and use of evidence-based educational materials and teaching strategies, and can be a strong voice for interdisciplinary falls prevention education in long-term care.
The author reports no relevant financial relationships.









