Practical Management of Urinary Incontinence in the Long-Term Care Setting
INTRODUCTION
The prevalence of urinary incontinence among nursing home residents ranges between 40-70%.1 Urinary incontinence can be defined in general as an involuntary leakage of urine.2 There are several different types of urinary incontinence including urge, stress, mixed, overflow, and functional incontinence. Urge incontinence is involuntary leakage accompanied or immediately proceeded by urgency,2 and indicates detrusor overactivity. Stress incontinence is involuntary leakage from effort or exertion, or from sneezing or coughing,2 and is usually related to increased urethral mobility, poor intrinsic sphincter function, or weak pelvic floor muscles. Mixed incontinence is the combination of urge and stress incontinence. Overflow incontinence is associated with overdistention of the bladder caused by obstruction (eg, enlarged prostate) or a neurological condition (eg, spinal cord injury). Functional incontinence is leakage in the presence of an intact lower urinary tract system and is due to functional limitations such as decreased mobility, cognitive impairment, or dressing apraxia.
The assessment and management of urinary incontinence in long-term care facilities is an important issue given its high prevalence and its association with morbidity and increased costs. Residents with incontinence may be at risk for falls,3 skin breakdown (eg, perineal dermatitis, skin maceration, skin erosions), and pressure ulcers. However, it should be noted that there is weak correlation between urinary incontinence and pressure ulcer development.4-6 Urinary incontinence is associated with poor self-rated health and decreased quality of life.7,8 The annual cost attributed to urinary incontinence is several thousand dollars per resident with incontinence.9,10
The U.S. Centers for Medicare & Medicaid Services (CMS) released on June 27, 2005, revised interpretative guidance on urinary incontinence to the surveyor community.11 Although the regulation (F-315) did not change, the guidance to federal and state surveyors did change. The regulation still requires that facilities: a) do not insert an indwelling urinary catheter unless the resident’s clinical condition demonstrates that it is necessary; b) provide appropriate treatment and services to prevent urinary tract infections; and c) assist residents to restore as much bladder function as possible. If a facility does not achieve all three criteria it may result in financial penalties ranging from $500-$10,000 per day. Thus, it is imperative that long-term care facilities understand this very important guidance. Although the 50-page document may appear daunting, it suggests that the overall components of effective urinary incontinence management are recognizing and assessing factors affecting urinary function, implementing interventions to address correctable underlying causes in accordance with resident needs and goals, and monitoring residents’ responses to treatment.
The purpose of this article is to highlight some of the key aspects of the revised interpretive guidance and to provide algorithms that can assist facilities in meeting the revised CMS guidance.
RISK FACTORS FOR URINARY INCONTINENCE
Residents of long-term care facilities tend to be a heterogeneous group. They suffer from a variety of conditions including chronic disease, cognitive impairment, and functional limitations. Although the etiology of urinary incontinence in long-term care residents is usually multifactorial, dementia and functional impairments are frequent contributors.4,12 Mobility problems and dependency in transfers are better predictors of continence status than cognition, suggesting that residents with dementia may have the potential to remain continent as long as they are mobile.13,14 Other potentially modifiable factors include poor pelvic floor muscle contraction, constipation, poorly controlled diabetes, delirium, systolic hypertension, parkinsonism, arthritis, back problems, hearing and visual impairment, recurrent urinary tract infections, medications (eg, benzodiazepines, tranquilizers, antidepressants, hypnotics, and diuretics), high caffeine intake, smoking, and obesity.12
INITIAL ASSESSMENT OF LONG-TERM CARE RESIDENTS WITH INCONTINENCE
The CMS guidance requires that an appropriate assessment be conducted and documented. Such a comprehensive urinary incontinence assessment may be best performed using a team approach that includes both nursing staff and physicians. A detailed history should be obtained that includes details of the symptoms and voiding patterns, medications, related comorbidities, and other potentially modifiable risk factors.
Efforts should be made to identify the type of urinary incontinence, which may require completion of a bladder diary by the resident and/or nursing home staff. A bladder diary will help determine the frequency of incontinence episodes, potential precipitating factors, and the resident’s usual voiding pattern. Subsequent bladder diaries can monitor response to treatment.
Modifiable risk factors should be identified. Although there is insufficient evidence from controlled trials that treating factors associated with urinary incontinence results in improvement, it is generally agreed that risk factor identification and modification is appropriate.15-17 Compliance with the new CMS guidance requires that correctable underlying causes of incontinence are identified and interventions to address them are implemented.
Physical examination should include blood pressure measurement, body mass index determination, and neurological, mental status, abdominal, and mobility examinations to evaluate for potentially modifiable risk factors. A rectal examination should be performed to evaluate rectal tone, assess for fecal impaction, and, in men, to evaluate prostate size. It is appropriate to perform a pelvic examination in women, which focuses on assessment of pelvic floor muscle strength and identification of masses and symptomatic pelvic organ prolapse. Direct observation of urine loss can be performed using a cough stress test. Instantaneous urine leakage upon coughing is consistent with stress incontinence.
The postvoid residual urine volume should be determined using in-and-out bladder catheterization or a portable ultrasound bladder scanner.18 For mild to moderate elevations (100cc -200cc), repeat postvoid urine volume measurements may be indicated. Postvoid residual volumes of 200cc or more should prompt consideration of further evaluation by a urologist or urogynecologist.1,16 Other reasons to consider referral for further evaluation include diagnostic uncertainty, recurrent urinary tract infections, hematuria without infection, symptomatic pelvic organ prolapse, obstructive urinary symptoms, or failed conservative treatment in patients who may benefit from surgical treatment.
A functional assessment with development of an associated management plan by an occupational therapist and/or physical therapist may be beneficial. There is evidence that combining continence care with functionally oriented exercise improves continence and other functional outcomes among long-term care residents.19,20
It is appropriate to perform a urinalysis. A urinalysis will help to identify sterile hematuria and symptomatic urinary tract infections. However, eradicating asymptomatic bacteriuria appears to have no effect on chronic urinary incontinence among nursing home residents.21 The CMS guidance defines symptomatic urinary tract infections, in noncatheterized residents, as a positive urine culture in the presence of at least three of the following: 1) fever; 2) new or increased burning on urination, frequency, or urgency; 3) new flank or suprapubic pain or tenderness; 4) change in character of urine; 5) worsening of mental or functional status.
Other laboratory tests can be conducted if indicated based on the history and physical examination. Specialized tests, such as urodynamics and cystoscopy, are not intended to be part of the initial evaluation.16
MANAGEMENT OPTIONS AND ALGORITHMS
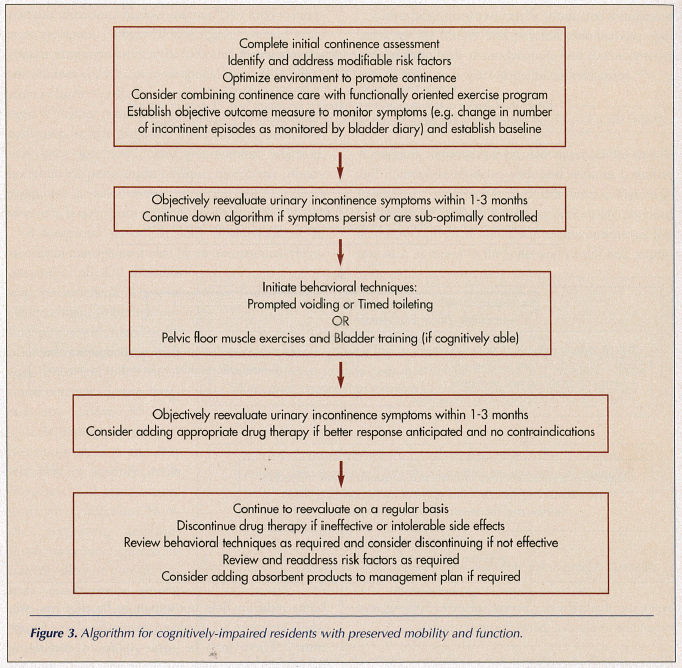
A practical, stepwise management approach for mobile and nonmobile residents with and without cognitive impairment is outlined in algorithm form in Figures 1-3. Details of different treatment options are provided below. All care plans should address environmental factors such as access to the toilet and/or call bell, appropriate use of assistive devices and adaptive clothing, and avoidance of physical barriers and restraints.

Behavioral Techniques
Prompted voiding requires caregivers to ask dependent residents on a regular basis whether they need toileting assistance. The resident is assisted to the toilet only if he/she requests it and receives positive feedback if he/she voids successfully when prompted. Prompted voiding has been found to increase self-initiated voiding and decrease incontinent episodes.22 Prompted voiding is successful for persons with dementia, as long as they can recognize their own name and/or identify objects. Nighttime prompted voiding among nursing home residents does not appear to be effective, even when attempts are made to minimize sleep disruption.23 There may be some value to combining prompted voiding with anticholinergic medication for the treatment of urge incontinence, especially in residents who do not respond adequately to prompted voiding alone.24
Timed voiding is passive assisted toileting initiated by a caregiver at fixed 2-3- hour time intervals. It is appropriate for residents who cannot independently toilet themselves. Although there is limited data from randomized controlled trials, timed voiding in combination with other interventions may be more effective than usual incontinence care.25

Habit retraining involves identification of a person’s toileting pattern and development of an individualized toileting routine that aims to keep the voiding interval as long as possible without incontinence. Habit retraining may reduce skin rash but is labor-intensive. A Cochrane review found no significant difference in the incidence and in the volume of incontinence, however there were nonsignificant improvements of these measures.26
Pelvic floor muscle exercises, or Kegel exercises, involve repeated voluntary pelvic floor muscle contraction. In order to strengthen the pelvic floor muscles the resident first needs to be able isolate and contract them. Each contraction needs to be held for several seconds, several contractions should be performed within each session, and several sessions are to be performed each day. This treatment modality requires that the resident be able to learn and perform the exercises consistently. Pelvic floor muscle training appears to be effective in individuals with stress, urge, and mixed incontinence, and there does not appear to be any advantage to adding biofeedback techniques to these exercises.27 Combining pelvic floor muscle training with bladder training is more effective than either therapy alone.
Bladder training aims to increase the time interval between voids using progressive voiding schedules, distraction techniques, and pelvic floor contractions. This therapy requires residents to be able to toilet independently and to monitor and comply with voiding schedules. Clinical trials appear to favor bladder training, though greater effectiveness is achieved when used in combination with pelvic floor muscle training.28
Medications
Anticholinergic medications, such as oxybutynin and tolterodine, significantly improve symptoms associated with overactive bladder syndrome (urgency with frequency and/or urge incontinence).29 However, studies have also reported significantly more dry mouth and higher residual urine volumes with these medications.30 There are other potential adverse effects (eg, tachycardia, confusion, dizziness, abnormal vision, dry eyes, urinary retention, headache, nausea, constipation), and these medications are contraindicated in patients with narrow-angle glaucoma, urinary retention, and gastric retention. They also have to be used with caution in persons with dementia given the increased risk of confusion. There is evidence to suggest that extended-release formulations may cause fewer side effects, specifically less dry mouth.31 Lower doses may also be as effective and have less risk of dry mouth. An oxybutynin transdermal patch can be used for residents who have difficulty swallowing, but cutaneous side effects are frequent. The newer antimuscarinic agents, such as trospium chloride, solifenacin and darifenacin, may also be an option. They appear to be effective in the treatment of urge incontinence but also have anticholinergic side effects, and their advantage over oxybutynin and tolterodine has not yet been established.31-34
Doxepin, a tricyclic antidepressant, has recently been studied in women with detrusor instability or urinary incontinence and has been found to subjectively improve symptoms.35 Tricyclic antidepressants can have anticholinergic side effects and have also been associated with hypotension.
Adrenergic drugs have been evaluated for the treatment of stress incontinence, and the limited evidence demonstrates improvement compared to placebo.36 However, these drugs can cause serious side effects and are not recommended for frail and/or older persons with dementia. Duloxetine, a new selective serotonin-noradrenalin reuptake inhibitor (SNRI), has been found to improve quality of life and reduce incontinence episode frequency in individuals with stress incontinence.37 Although subjective cure favors duloxetine over placebo, there was no difference in objective cure. The most common reported side effect was nausea;38 however further long-term follow-up is required to rule out serious side effects.
Estrogens, both oral and topical formulations, have been used in the management of urinary incontinence. Estrogens were hypothesized to improve urinary incontinence by improving vaginal atrophy. However, the Women’s Health Initiative hormone replacement therapy trial found that both estrogen replacement therapy and hormone replacement therapy were actually associated with increased incidence of all types of urinary incontinence and also worsened existing urinary incontinence.39 Therefore, estrogens no longer appear to be a treatment option for urinary incontinence.
There are pharmacological management options for the management of obstructive symptoms and overflow incontinence associated with benign prostatic hyperplasia that will not be addressed in this review.
Urinary Catheters
Catheter types include external catheters (eg, condom catheters), indwelling catheters, or intermittent catheterization. External catheterization in male nursing home residents has been found to increase the risk of symptomatic urinary tract infections.40 The role of intermittent catheterization among nursing home residents has not been well studied. Indwelling catheters are often overused and have been associated with bacteriuria, symptomatic urinary tract infection, and increased risk of death.41-47 There is insufficient evidence to draw conclusions about what type of catheter to use in the long-term management of neurogenic bladder.48 The CMS guidance requires that there be medical justification for the initiation and continued use of indwelling catheters. These indications include urinary retention that cannot be managed medically or surgically, stage III or IV pressure ulcers where urine has impeded healing despite appropriate personal care, and terminal illness or severe impairment where positioning changes are uncomfortable or painful.
Pessaries and Absorbent Products
Pelvic organ prolapse can contribute to urinary incontinence in women. Although there is a dearth of evidence,49 pessaries can be used in the management of pelvic organ prolapse. They are inserted into the vagina and need to be removed at regular intervals in order to inspect the vaginal mucosa for erosions.
The CMS guidance requires that absorbent products not be used as the primary approach to continence management until other approaches have been considered. Incontinence garments include disposable and reusable bodyworns (eg, diapers, pad and pant combinations) and disposable and reusable underpads (ie, bedpans). Disposable products contain a fluff pulp core with or without superabsorbent material. Disposable products may be better than nondisposable products at decreasing skin problems, and superabsorbent products may perform better than products containing only fluff pulp; however, data is limited, and new products are continually arising on the market.50
TARGETING MANAGEMENT PLANS TO THE INDIVIDUAL RESIDENT
Functional status, cognitive abilities, comorbidities, and preferences should be considered when developing a continence management plan for each long-term care resident. The resident or his/her legal representative should be involved in the design of an appropriate care plan. The CMS guidance allows long-term care facilities to develop standard treatment protocols or care plans that can then be appropriately adapted to the individual. These care plans need to include an initial comprehensive assessment, measurable objective outcomes, time frames to assess whether the objective outcomes have been met, and the ability to modify the care plan if required. An appropriate outcome measure would be a decrease in the number of incontinent episodes, ideally determined objectively through the use of bladder diaries.
SYSTEM AND PERSONNEL BARRIERS TO MANAGING URINARY INCONTINENCE
Although the efficacy of interventions to improve continence management in nursing home residents is well documented, implementing and sustaining these interventions in “real-life” presents unique challenges and opportunities. Staffing issues, negative beliefs and perceptions about urinary incontinence, and the incremental costs associated with implementing labor-intensive interventions for frail nursing home residents are among the potential barriers to optimal implementation of management programs.19,51,52
The success of any intervention to improve continence care for nursing home residents will need to address the individual, group, organizational, and environmental level factors that set sustainable care. These will vary for every institution. At the very least, educational programs for the personnel that focus on knowledge, attitudes, and skill development will be required. Educative strategies that are interactive and participatory are usually preferred, and these will need to take into account different literacy levels among the participants. Audio-visual educational materials and resources may be more effective than distributing written tools or algorithms. Designating a continence specialist in each institution may be one way of ensuring that continence programs are maintained even in the face of high staff turnover. Methods of ensuring system accountability for following the CMS guidance will also need to be established. These might include weekly or monthly statistics of continence/incontinence rates and average number of absorbent products needed per resident per week or month.
CONCLUSIONS
Urinary incontinence is a prevalent condition among nursing home residents that is associated with morbidity and increased costs. The new CMS guidance requires that long-term care facilities establish protocols to evaluate and appropriately manage urinary incontinence. There are several behavioral strategies that can be effectively implemented within long-term care facilities, and many of these strategies can be used successfully for residents with impaired mobility and dementia. It is evident that CMS has raised the bar on the expectations for the effective assessment and management of urinary incontinence in long-term care. However, these algorithms may be an effective method for meeting the new guidance.
The authors report no relevant financial relationships.









