Beyond the Basics: Special Issues in Venous Thromboembolism Prevention
INCIDENCE
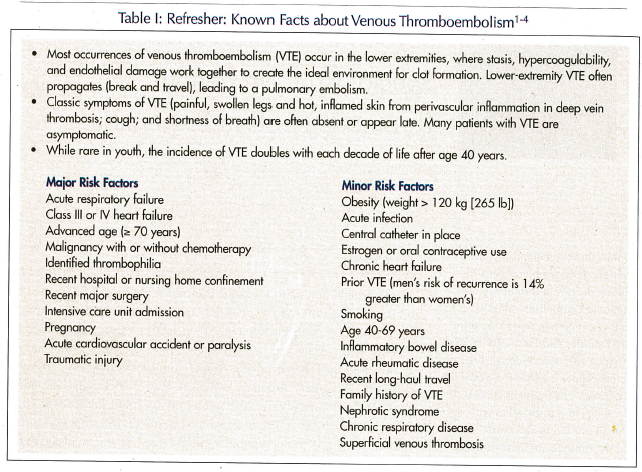
In the general population, venous thromboembolism (VTE) occurs at a rate of one to two events per 1000 annually, with deep vein thrombosis (DVT) accounting for more than half of these. Approximately 75% of these events are first occurrences.1 In the elderly, who are at greater risk, the stakes are high. At one year, the mortality is 21% and 39% for DVT and pulmonary embolism (PE), respectively. The odds ratio for developing VTE in the community is 1, but increases to 10.6 in long-term care (LTC) residents. In the hospital, the rate is 465 times greater than in the general population.2-5 Table I lists some of the well-known facts about DVT. Although most studies have been conducted in general populations, clearly elderly individuals, and especially those who are acutely confined or who have one major risk factor or two minor risk factors, are at increased risk.2
PREVENTION IS POSSIBLE
Several studies have found that up to 75% of medical patients and most surgical patients are at high risk for VTE because they have one or more risk factors (that are cumulative).5-8 Risk of VTE in hospitalized patients varies considerably, depending on the patient’s underlying disease; myocardial infarction, stroke, and malignant disease are linked to the highest risk rates.7 Many LTC residents experience acute or exacerbated illness that leads to an abrupt cessation of mobility, or simply increases VTE risk. Various prophylactic measures are available, including nonpharmacologic steps such as maintaining mobility or promoting early mobility after acute confinement, and using compression stockings, intermittent pneumatic compression devices, or leg elevation. Because they lack bleeding potential, these measures are often primary interventions for residents with high bleeding risks. While the prophylactic measures have been shown to reduce DVT risk in several groups of residents, they are generally less efficacious than anticoagulants for DVT prevention.8
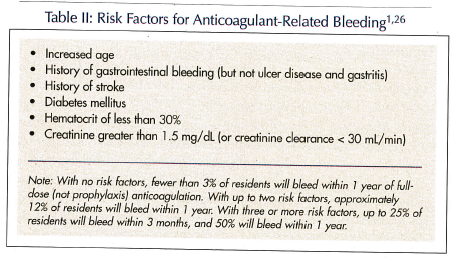
Anticoagulant medication, therefore, may be more effective. In the prevention armamentarium, the Food and Drug Administration has approved heparin, warfarin, the low-molecular-weight heparins (LMWHs; eg, dalteparin, enoxaparin, tinzaparin), and the ultra-low-molecular-weight heparin fondaparinux for VTE prevention, usually at doses lower than those employed for treatment. Although LTC clinicians are familiar with these drugs, they may have concerns about specific drugs or drug classes. Among the concerns are the potential to increase bleeding risk (Table II), food–drug and drug–drug interactions, administration route or time, cost, and treatment duration. Residents and their families may have similar concerns.
Bleeding
Long-term care clinicians may be concerned about possible intracranial hemorrhage or severe hematoma, especially in elderly residents aged 85 or older, and often hesitate to prescribe VTE prophylaxis.9,10 When using warfarin, the international normalized ratio (INR) must be monitored and should remain in a target range of 2.0-3.0. International normalized ratios of 3.5 or greater should be avoided. For heparin, the prothrombin time (PT)/partial thromboplastin time (PTT) must be monitored in lieu of the INR. Except in those residents who have renal failure or weigh less than 45 kg (100 lbs) or more than 104 kg (230 lbs), no monitoring is necessary for the LMWHs.10 The anti-Factor Xa may be used to monitor the LMWHs’ anticoagulant effect for these high-risk residents.
Two issues commonly raise the specter of potential bleeding: routine cardioprophylaxis with low-dose aspirin (ie, a nonsteroidal anti-inflammatory drug [NSAID]), and the need for invasive surgery or dental care. Concurrent use of warfarin and NSAIDs increases the incidence of gastrointestinal bleeding. Studies have found that the relative risk is 13 times greater when NSAIDs and warfarin are administered concurrently.11-13 Approximately 20% of the adult population has indications for low-dose aspirin prophylaxis,14 and its use is expected to increase. Residents of LTC facilities have high rates of cardiovascular disease, and may use aspirin more frequently than the rest of the population. A recent large study found that low-dose aspirin was implicated in 18% of adverse drug reactions leading to hospitalization; this finding suggests an emerging problem.15 Studies have also found that aspirin at any dose—even the 81-mg dose often employed as prophylaxis, or buffered or enteric-coated formulations—reduces intestinal prostaglandin levels approximately 40% and increases the risk for gastrointestinal bleeding.16,17 Clinicians who chose to employ anticoagulants with low-dose aspirin should acknowledge this increased risk and monitor appropriately.
The American College of Chest Physicians 7th Annual Conference on Antithrombotic and Thrombolytic Therapy Evidence-Based Guidelines continue to recommend discontinuing warfarin at least 4 days before invasive surgery, and using a LMWH or unfractionated heparin to bridge therapy. In the past, sending anticoagulant-treated residents for dental work raised questions, such as “Should the anticoagulant be held?” Currently, the guidelines recommend that warfarin should be continued uninterrupted. Clinicians who are concerned about potential local bleeding can prescribe tranexamic acid or epsilon-aminocaproic acid mouthwash.18
Administration Route or Time
Oral formulations are clearly preferred for most LTC residents, except for those who have had recent upper gastrointestinal surgery, documented absorption problems, dysphagia, or who are too uncooperative to handle capsules or tablets. Oral formulations save nursing time and are less invasive than most other administration routes. Currently, warfarin is the only available oral anticoagulant. Despite widespread know-ledge about its many food and drug interactions, it occupies positions 1 through 5 on the American Society of Consultant Pharmacists (ASCP) list of Top Ten Dangerous Drug Interactions in Long-Term Care.19
Heparin, the LMWHs, and fondaparinux are usually given subcutaneously in the LTC environment. The incidence of adverse skin reactions related to these agents is low, and the reactions are predominantly benign. Urticarial rash, bruising, and discoloration are the most common reactions. In rare instances, necrosis or an anaphylactic-type reaction can occur; these usually resolve when the agents are discontinued, and rechallenge is ill-advised.20 The LMWHs and fondaparinux are available as prefilled syringes with a needle-shielding system, which minimizes the risk of dosing error and needlestick injury.
Often, warfarin is given in the evening, so attending physicians can adjust doses based on laboratory work drawn in the morning. Timing is not a concern with the other agents.
Food–Drug and Drug–Drug Interactions
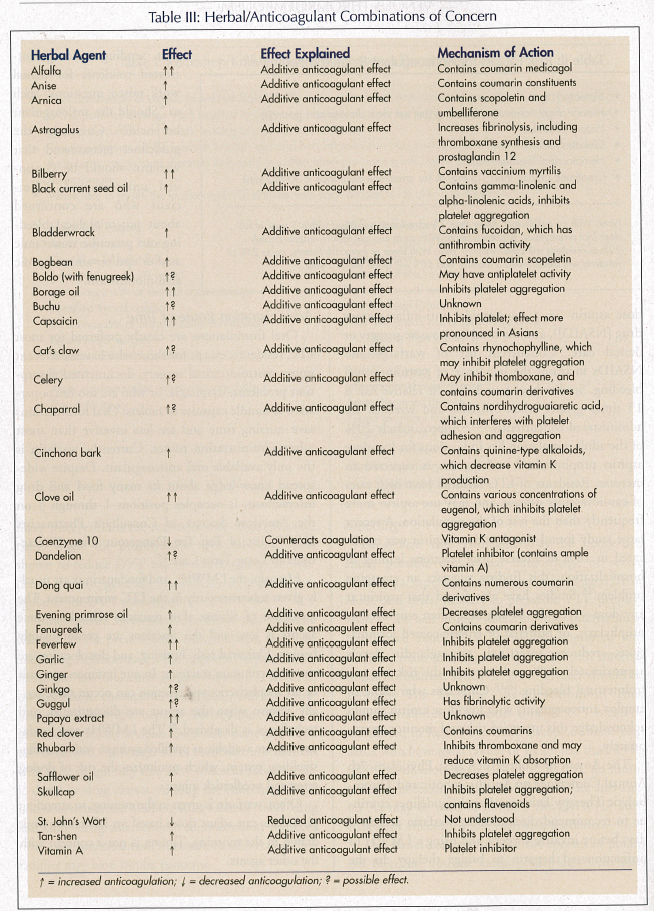
All of the anticoagulants have the potential to interact with numerous herbal/alternative medicaments (Table III). Warfarin’s many additional food and drug interactions increase risk and can disrupt treatment because of its narrow therapeutic window and patients’ variable dose response. This drug’s mechanism of action involves vitamin K–dependent clotting factors, and it interacts with vitamin K–containing foods. Most clinicians are aware that common foods like spinach, seaweed, broccoli, turnip greens, and mango interact with warfarin, and residents must maintain or be maintained on a consistent diet. In the last few years, dietitians have determined that pine nuts, cashews, prunes, liver, kiwi fruit, some cheeses, liquid dietary supplements,21 and smoking (chewing tobacco)22 also have high vitamin K levels, and can cause INR changes.
Out-of-range INRs occur frequently during warfarin therapy. Concomitant drugs, changes in medical condition, alcohol use, and activity level may alter INRs. One study of 1020 patients with a mean age of 60.2 years found that the most frequent cause of insufficient anticoagulation (29.7%) was “indeterminate.”23 Other causes included a response to previous dosage change (16.4%), noncompliance or dosing errors (16.3%), and recent therapy initiation (15.6%). When INRs exceeded 4.0, indeterminate findings accounted for 43% of cases. Thus, excessive and insufficient anticoagulation with warfarin is often unexplained.23
Often, acetaminophen is prescribed because warfarin interacts with most NSAIDs. One significant study, however, examined unexplained elevated INRs, and found that the odds of having an INR greater than 6.0 were tenfold higher in adults taking acetaminophen 9100 mg or more weekly.24 The ASCP indicates that short-term use of acetaminophen (less than 2 g/day) does not appear to affect the INR,25 but this study suggests acetaminophen as an underrecognized cause of excessive anticoagulation.24
Heparin interacts with cephalosporins, penicillins, nitroglycerin, digoxin, tetracyclines, nicotine, and some antihistamines. The LMWHs have few interactions, but their concurrent use with NSAIDs increases the risk of gastrointestinal bleeding. Residents taking both should be monitored closely. Obesity or very low body weight, renal failure, and abnormal clotting factors are not strict contraindications to LMWHs but are serious concerns. Monitoring of anti-Xa levels can guide LMWH dosing.10 Peak anti-Xa levels are monitored 4 hours after subcutaneous administration, and dosing should be adjusted to maintain a target peak anti-Xa level of 0.2-0.6 IU/mL.26
Cost
The cost of anticoagulant therapy varies significantly depending on the drug employed and the facility. Facilities that understand that failure to prevent one DVT or PE leads to costs of $17,000 or more will be able to put prophylaxis costs in perspective.25 Each agent’s cost is a composite of drug cost, administration cost, monitoring cost, and the cost of managing any consequent adverse events. Warfarin’s low purchase price, for example, is a poor indication of total cost because frequent monitoring is necessary. If point-of-care INR testing (now technologically advanced and reliable) is unavailable, laboratory costs can increase the total cost significantly. Phlebotomy can also be difficult or inconvenient, especially in cognitively impaired residents.27-29
Most pharmacoeconomic analyses have been conducted in hospitals on patients having orthopedic surgery or experiencing serious exacerbations of medical problems. They confirm that prophylaxis with any anticoagulant is more cost-effective than no prophylaxis, and LMWHs or fondaparinux are superior to unfractionated heparin or warfarin, and are cost-effective. LMWHs are now the standard of care in these settings. After major orthopedic surgery, a LMWH or fondaparinux further reduces the likelihood of VTE complications.30-32 The mandate for LTC clinicians is twofold: to be certain that VTE prophylaxis continues appropriately when residents return from or are admitted after total hip or total knee replacement, and to initiate prophylaxis when ambulatory residents become acutely bedridden.
Treatment Duration
Later, the mandate is to ensure that prophylaxis is not continued unnecessarily. Treatment duration is perhaps the most difficult issue of all, and few studies have looked at the effectiveness of using mechanical prophylaxis alone. The best evidence for drug prophylaxis duration is available, again, from surgical candidates. An optimal prophylaxis duration has not yet been established. Many of these patients develop VTE up to 6 weeks after surgery. Prolonged prophylaxis of 3-4 weeks duration after surgery may benefit high-risk patients. In elective hip replacement, four studies of prolonged prophylaxis with a LMWH for 3-4 weeks after hospital discharge demonstrated a significant reduction in the incidence of venography-confirmed DVT.32-35
The evidence is weaker for patients with acute medical illnesses, but most studies have used a duration of 7-14 days after acute immobilization.35 Here, prescribers must assess each candidate’s risk factors before making a decision about whether or how long to employ prophylaxis.
CONCLUSION
Prescribing and administering VTE prophylaxis remains an area lacking precise guidelines, especially when the candidate is a LTC resident. Heightening awareness and taking appropriate precautions based on each resident’s unique characteristics can prevent VTE-induced morbidity and mortality. Long-term care facilities should consider designating VTE prevention as a performance improvement initiative, and should implement screening or assessment tools specific to the elderly that identify residents at high risk.
The views expressed herein are those of the author and not necessarily those of any government agency.
The author reports no relevant financial relationships.









