A One-Page Nursing Home to Emergency Room Transfer Form: What a Difference It Can Make During an Emergency!
BACKGROUND
As stated in our previous article on nursing home (NH) transfer, published in the May 2005 issue, a major complaint of NHs involves transfer of NH residents to and from the emergency room (ER),1 especially when it happens after hours when administrative staff are no longer in the facility. At the same time, the ER staff can encounter great difficulty in determining the exact reason why the NH resident was sent to the ER. Often, little is known concerning the medical problems that necessitate the transfer.2 Nursing home residents have complex needs due to their numerous comorbidities and psychosocial needs. Therefore, effective communication between NHs and the ER is essential.
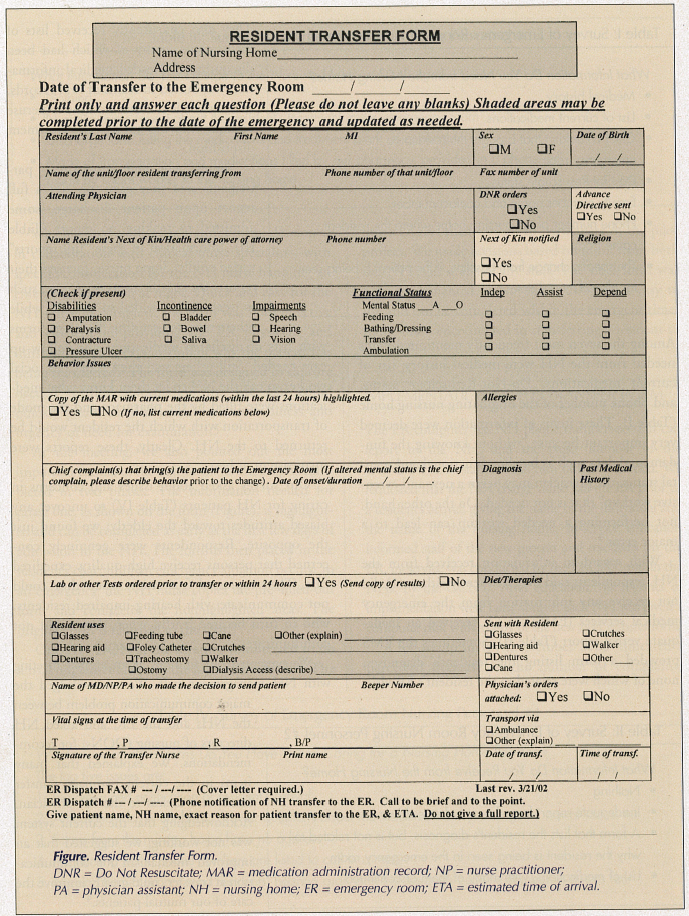
In the University of Texas Medical Branch hospital ER, the geriatric clinical nurse specialist and the emergency room clinical nurse specialist collaborated to develop a one-page “Resident Transfer Form” (Figure). The form, which the NH nurse can fill out quickly during an emergency, provides ER staff with a clear description of the situation. This form has been in use for four years, and is monitored monthly for compliance. Emergency room staff are pleased with the form, and it has reportedly reduced the number of problems related to NH transfer.
DEVELOPMENT OF THE TRANSFER FORM
To understand the problem, we formed a collaborative project between the geriatric clinical nurse specialist (GCNS)/nursing home liaison (NHL) and the ER clinical nurse specialist (ERCNS). We surveyed approximately 120 ER nursing personnel who worked 12-hour shifts using an open-forum discussion. To include as many nurses as possible, we held four meetings with both day and night shifts, each approximately one week apart. We asked the following questions:
• What information do you need from the nursing home?
• What information do you receive from the nursing home?
• What information do you provide to the nursing home at discharge?
• What issues and concerns do you have when caring for a nursing home resident? (Tables I-IV)
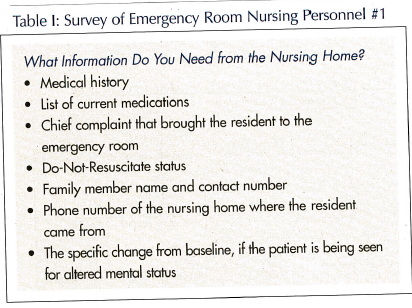 Among the seven most frequently mentioned items needed from the NH were medical history, list of current medications, Do-Not-Resuscitate status, and phone number of the originating nursing home (Table I). These items of information were deemed very important because “without knowing the fundamental data such as baseline functional and mental status, the physician may begin a new and extensive workup” that is not needed. On the other hand, not performing a needed workup can lead to a major error.3
Among the seven most frequently mentioned items needed from the NH were medical history, list of current medications, Do-Not-Resuscitate status, and phone number of the originating nursing home (Table I). These items of information were deemed very important because “without knowing the fundamental data such as baseline functional and mental status, the physician may begin a new and extensive workup” that is not needed. On the other hand, not performing a needed workup can lead to a major error.3
With regard to information received from the NH, respondents said they frequently either: (1) did not receive any information from the emergency medical services (EMS); or (2) received an inadequate verbal report (Table II). Sometimes the EMS provided a form listing the resident’s diagnoses, none of which were related to the resident’s ER visit. They also consistently received lists of medications, many of which had been discontinued. Needed medical information was buried in reams of NH records, which the ER staff has no time to peruse without delaying appropriate treatment disposition.
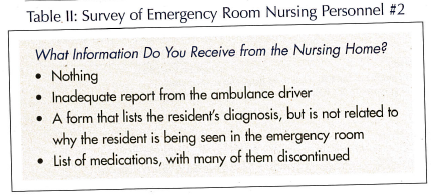
Interestingly, while most survey participants said they gave the NH a full report upon patient discharge, some admitted to making no report (Table III). Information in these “full reports” varied wildly. Some nurses focused their reports on specific aspects of care, such as treatment provided in the ER, while others reported sending discharge forms with lists of discharge medications and follow-up care needed. Still others said they asked the social worker to call the NH to let them know what medications were filled by the pharmacy and the mode of transportation with which the resident would be returned to the NH. Clearly, these reports were inconsistent at best.
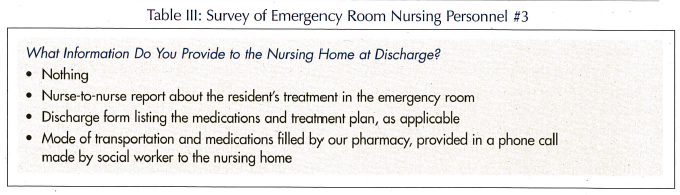
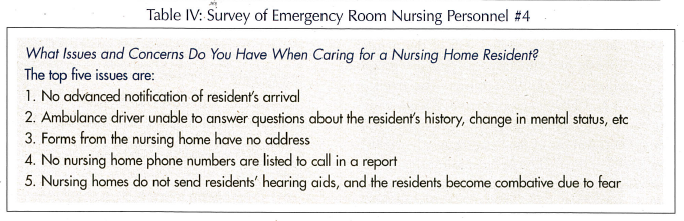
Our survey asked about issues and concerns in caring for NH patients (Table IV) to uncover any biased attitudes toward the elderly; we found just the opposite. Respondents were genuinely concerned that persons receive high-quality, expedited care. They expressed frustration when they could not communicate with hearing-impaired residents, who in turn became fearful when they could not communicate.
We presented our findings at an annual meeting with NH management staff. We acknowledged the major communication problem between the NHs and the ER, and asked NH directors of nursing (DONs) for recommendations. We explained that many items in the current two-page transfer form were useless to the ER physician. Acknowledging that the current system was not working, we suggested that an improved mechanism for communication at transfer could greatly improve the care of our mutual patients.4
We presented a one-page transfer form, developed in collaboration with clinical nurse specialists, with specific consideration for the NH nurse handling an emergency situation at night. Quick and easy for the NH nurse to complete, the form was both effective and efficient in providing the ER physician and nurse with a clear explanation of why the patient was being transferred.5 The form was designed to capture needed medical information the ER staff could quickly glean, such as severity of acute illness and urgency of need for examination.6
At the meeting, we also pointed out the most important feature of the new form: its one page is completed in two phases. The information needed for phase one, as shown on the form (Figure), is highlighted and can be completed as early as the first few days of admission to the NH. The form is then placed in the resident’s chart until an emergency situation occurs. In an emergency, the NH nurse copies the pre–filled-out form and completes the nonhighlighted areas. The original form is returned to the chart.
One NH DON at the meeting volunteered to do a trial implementation of the form in her facility. The other DONs then wanted to participate in the pilot project. We made revisions based on input from both the NH staff and the ER staff. The final form was fully implemented in November 2001. It is easy to use and can be completed within the emergent timeframe often encountered in transferring a resident to the ER.7
IMPLEMENTATION OF THE TRANSFER FORM
The ER computer has NH phone numbers so staff can report to the NH, and the pager number of the GCNS/NHL so staff can call him or her as needed. We requested that the NH charge nurse call the ER prior to a resident’s arrival, giving the name of the individual and the name of the nursing home. In-service education informed staff of the new process and resources (in the ER, in-service was conducted by the ERCNS, and in the NHs, by the GCNS). After education, the logistics of implementation were fairly simple: each NH was given a computer disk with a copy of the new NH transfer form.
A follow-up survey in October 2002 indicated a perceived decrease in the number of complaints from the ER nursing staff about NH documentation. When asked if they were satisfied with the new form, most staff answered “yes” and also stated that they were receiving the current medication records. The one-page form expedites gathering all needed information and saves ER staff from time-consuming checking of documentation. With ER phone numbers in the form, the NH nurse can easily call ER staff when a resident is on the way to the ER. This facilitates exchange of information if the ER staff member receiving the call needs to ask questions about the patient. Although the survey reported that, in most cases, the exact reason for the ER visit remained either missing or unclear, ER physicians reported informally that the NH transfer form was very helpful when it actually arrived with the resident.
We also found that, initially, the new NH transfer form was not used consistently, so we developed a tracking mechanism. A dispatch log was created wherein the ER dispatchers recorded the name of the resident, the name of the NH residence, and whether the form was used. After one month, the ERCNS and GCNS reviewed the results. If the form was not used by a specific NH or was not completed, the GCNS contacted the NH DON so he or she could follow up with the staff. The DONs were very receptive, intervened immediately, and compliance at the NH improved. After implementing these changes, use of the NH form increased from 30% to 70%. Today, use is at 90%.
BARRIERS TO IMPLEMENTATION OF THE TRANSFER FORM
The high NH nursing staff turnover rate requires periodic in-servicing to remind staff of the transfer form. However, one unresolved barrier continues to be a problem: NH DON turnover. The frequent change of NH DONs means the GCNS must continue soliciting support from new DONs for the program. Decreased use of the form frequently signals a new DON at the facility. At one facility, the nursing staff liked using the form, but the new director’s resistance resulted in communication setbacks.
FUTURE PLANS
We monitor compliance monthly with use of the NH transfer form, periodically providing in-service education for NH staff on the importance of the form and how to use it. Our current challenge is to establish a process that is not dependent upon NH DONs. Two nursing homes that send all their residents to our ER present little problem, but the four nursing homes that send their residents to another ER and maintain company-specific transfer forms continue to have some compliance problems. In our latest intervention, we changed the form title from “NH Transfer Form” to “Resident Transfer Form,” for ready identification by NH nurses.
A one-page NH-to-ER transfer form—clearly identifiable and supported by administrative buy-in and periodic training—shaves essential minutes from evaluation time when a NH resident arrives in the ER. After four years, our system is still being improved, but it serves as a reminder that individuals in special circumstances, such as residents of long-term care facilities, can benefit from coordinated, sustained attempts to address care issues, and that these attempts need not be complicated or expensive. Together, NHs and ERs can make incremental improvements that add up to greater benefits.
The research reported in this article was supported by the Department of Health and Human Services (DHHS), National Institutes of Health, National Institute on Aging grant PG0-AG17231, and DHHS, Agency for Healthcare Research and Quality grant R24-HS11618.










