Managing Urinary Tract Infections: Guide for Nursing Home Practitioners
EPIDEMIOLOGY OF URINARY TRACT INFECTIONS IN THE ELDERLY
Urinary tract infections (UTIs) are the most common bacterial infections encountered in nursing home residents.1 The prevalence of UTIs increases with advancing age in both men and women. With advancing age, the female/male ratio of UTI incidence narrows, approaching 2:1 in older adults. This change is attributed to the increased incidence of UTI among elderly men that accompanies the increased prevalence of bladder outlet obstruction due to prostatic enlargement, as well as to the relative reduction in UTI incidence among elderly women due to decreased sexual activity.2 Recurrent and complicated UTIs are also more common in older adults compared to younger adults. This is attributed to the increased frequency of predisposing anatomic and pathophysiologic factors, such as uterine prolapse, urolithiasis, and genitourinary tract malignancies. Urinary tract infections that complicate the use of urinary catheters are common in the elderly and are associated with increased morbidity.3 Older adults with UTI have more types of urinary tract pathogens compared to younger patients. Escherichia coli (E. coli) is the most frequently isolated urinary pathogen identified in 70% of outpatient elderly females with UTI and in 40% of older patients with urethral catheters.4 Gram-positive bacteria (eg, enterococci, coagulase-negative staphylococci, and group B streptococci) are more frequently isolated in patients with recurrent UTI as a result of frequent use of antibiotics that are inactive against these organisms (eg, quinolones).4
Several factors have been linked to the development of UTI in the elderly. These include increased age, menopause, and instrumentation of the urinary tract. Another risk factor that is often overlooked is dehydration.5 Factors that were found unrelated to the development of UTI include diet and personal hygiene.6,7
As part of the Nursing Home Quality Initiative (NHQI) that became effective January 1, 2004, the percentage of residents with a urinary tract infection over the past 30 days and the percentage of residents who have or had a catheter inserted and left in their bladder over the past 14 days became two of the quality measures publicly released by the Centers for Medicare and Medicaid Services (CMS) on all Medicare- and Medicaid-certified nursing homes on the Nursing Home Compare website.8
ASYMPTOMATIC BACTERIURIA OR UTI
The Association for Professionals in Infection Control and Epidemiology (APIC) defines a positive urine culture as a laboratory confirmation of > 100,000 colony-forming units (CFU)/mL.9 However, a positive urine culture does not indicate whether a nursing home resident has a UTI or asymptomatic bacteriuria (a positive culture without dysuria, urinary frequency, incontinence of recent onset, flank pain, fever, or other signs of infection during the week before a urine sample was obtained).10 Asymptomatic bacteriuria is not a UTI and should not be treated unless accompanied by symptoms that suggest a UTI.7 The prevalence of asymptomatic bacteriuria among residents in long-term care facilities is estimated to be 10-50%.10 Prospective studies have shown that untreated asymptomatic bacteriuria in long-term care residents without indwelling urinary catheters did not result in increased morbidity or mortality.11,12
Bacteriuria is a frequent complication of urinary catheter placement in nursing home residents. Bacteriuria has been detected at a rate of 3-10% per day among patients with urethral catheters. A single in-and-out catheterization may cause bacteriuria in as many as 20% of patients. By about 30 days (the cutoff period between short- and long-term catheterization), most patients have some degree of bacteriuria. Bacteriuria associated with short-term catheterization usually involves a single pathogen, most commonly E. coli. On the other hand, bacteriuria associated with long-term catheterization is often polymicrobial. It is important to note that the presence of bacteriuria does not imply or predict a UTI. Therefore, asymptomatic colonization should not be treated.13
DIAGNOSING UTI IN THE NURSING HOME
Symptomatic UTI can present with one or more of several symptoms such as dysuria, urinary frequency, and incontinence of recent onset, flank pain, or fever. Delirium and functional decline are two other symptoms that may accompany a UTI. It is worth noting that in the absence of fever or sepsis, an uncomplicated UTI is unlikely to cause significant central nervous system dysfunction and delirium.14 This observation, however, does not necessarily apply to nursing home residents with advanced dementia, as delirium and/or functional decline may be the only symptoms of a UTI in this group of patients.
The diagnosis of symptomatic UTI can be challenging in older adults. Symptoms such as dysuria, urinary frequency, and incontinence of recent onset, flank pain, and fever may not be present or may be overlooked. The diagnosis of UTI requires consideration not only of clinical symptoms, but also of comorbidities. For example, confusion and delirium may indicate a severe UTI, as might a change in appetite, agitation, or functional decline. Similarly, an elderly resident with urinary incontinence and a UTI may experience an increase in the number of episodes of incontinence. Some practitioners use the McGeer et al and MeSH definitions for long-term care nosocomial infections to diagnose symptomatic UTI.15 In order to meet the criteria for a suspected UTI without an indwelling catheter, 3 of the following must be met:
• Fever (> 38°C) or chills
• New or increased burning pain on urination
• New flank or suprapubic pain or tenderness
• Changes in character of urine
• Worsening mental function
On the other hand, in order to meet the criteria for a suspected UTI with an indwelling catheter, 2 of the following must be met:
• Fever (> 38°C) or chills
• New flank or suprapubic pain or tenderness
• Changes in character of urine
• Worsening mental function
Nursing home practitioners need to be reminded at this stage that federal guidelines define a UTI as “colonization (growth of bacteria) of the urinary tract with signs or symptoms of UTI.”16 Many long-term care federal and state surveyors interpret this regulation as that bacteriuria with any symptom is considered a UTI. Consequently, the McGeer et al and MeSH definition of a UTI in long-term care settings that was developed in Canada might not necessarily be applicable in U.S. nursing homes.
The diversity of potential pathogens makes it necessary to obtain urine cultures in elderly nursing home residents with suspected UTI. When or if to send a urine culture is another controversial issue. In general, cultures should not be sent in the absence of symptoms, or if a decision is made not to treat. Randomly screening urine from patients with indwelling catheters is not indicated in the absence of symptoms. The cost of culture and sensitivity testing of the urine is more than $100, and this should be taken into account when ordering urine culture and sensitivity tests.
Frail, elderly nursing home residents are often unable to provide midstream voided urine specimens for diagnostic testing. For men, it is frequently necessary to apply a clean condom external collection device to obtain the urine specimen,17 while in women it may be necessary to use in-and-out catheterization.10
Bacteriologic diagnosis of UTI is often based on the concept of clinically significant bacteriuria, which is usually defined as > 105 CFU/mL in a clean catch after more than 4 hours of bladder incubation. The urine must be refrigerated if culture and incubation are delayed. Storage of the urine specimen for more than 4 hours should be avoided as substantial bacterial replication still occurs, even at cold temperatures.
Dipstick (rapid) tests can help identify bacteriuria and can be performed in the facility. Studies, however, have shown that dipstick analysis is not sensitive enough to diagnose UTI in high-risk patients in whom a missed diagnosis would have a serious consequence.18 In addition, dipstick tests do not detect gram-positive organisms such as Enterococcus. The most widely used dipstick test is the nitrite test, in which the conversion of nitrate to nitrite by bacteria in the urine is demonstrated by color change on a dipstick. The test has a high degree of sensitivity and specificity but does not demonstrate bacteriuria caused by Pseudomonas sp., staphylococci, or enterococci, which are incapable of reducing nitrate to nitrite.
UTI COMPLICATING URINARY CATHETER PLACEMENT
It is estimated that 5-15% of long-term care residents have chronic urinary catheters in place.19,20 Urinary catheters are most frequently used in residents with urinary retention, urinary incontinence, and in those with sacral or perineal wounds. Transurethral urinary catheters are the most frequently used compared to suprapubic or condom-type catheters. No method, however, has proven superior for use in skilled nursing facilities. Saint and collegues21 surveyed 104 elderly male patients with either an indwelling or a condom catheterization and 99 nursing staff members in a Veterans Administration Hospital, and reported increased patient satisfaction with condom catheters compared to indwelling catheters, as they were perceived to be less painful and less restrictive. Nursing staff respondents, on the other hand, believed that condom catheters fell off, leaked more often, and required more nursing time. Use of condom catchers may be associated with a lower risk of UTI than transurethral catheters.22,23
About 21% of residents catheterized for more than 30 days (chronically catheterized residents) develop symptomatic urinary tract infections.24 Suprapubic urinary catheters are associated with lower risk of bacteriuria and increased patient satisfaction compared to transurethral catheters. This method, however, is associated with a higher degree of mechanical failure.22
Intermittent catheterization (in-and-out) may be applicable in a select group of patients. This technique is frequently utilized in patients with spinal cord injury who are capable of performing self-catheterization. Most residents in the nursing home, however, are unable to perform self-catheterization on their own and would require nursing staff assistance in order to perform this task. The burden on nursing staff time is likely to be prohibitive to the widespread utilization of this technique in many skilled nursing facilities. The high cost of disposable catheters is another compounding factor.25 Data from the literature indicate that bacteriuria is a universal finding in patients who have intermittent catheterization regularly. The majority of these patients, however, remain asymptomatic.26,27
At the present time, the consensus is lacking on when a transurethral urinary catheter should be changed. It is common practice in many skilled nursing facilities to change an indwelling catheter monthly. Priefer and collegues28 studied the relationship between the duration to changing transurethral urinary catheters and the incidence of symptomatic UTI, and reported no reduction in the incidence of symptomatic UTI with monthly versus as-needed catheter changes. On the other hand, catheter change at the onset of UTI is recommended, as it has been linked to faster clinical improvement, fewer febrile days, and a lower rate of infection relapse.29
Catheter-associated UTIs are common and carry increased risks of complications and morbidity. Federal regulations mandate that certain criteria be met in order to justify the use of an indwelling catheter in a skilled nursing facility. As noted in Intent: 483.25(d)(1) of OBRA ’87: “An indwelling catheter should only be used when there is valid medical justification. The resident should be assessed for and provided the care and treatment needed to reach his or her highest level of continence possible. The facility is expected to show evidence of any medical factors which caused the intervention.”16 Many residents are transferred to the nursing home from acute care hospitals with indwelling catheters. Unlike long-term care settings, acute care hospitals do not have to adhere to stringent criteria to justify use of a catheter. The result is that many nursing home residents who are admitted to an acute care hospital return to the nursing home with a urinary catheter, although they did not leave the nursing home with a catheter. In many cases, the catheter is inappropriately left in place, increasing the resident’s risk of developing a UTI. The Centers for Disease Control and Prevention (CDC) have published guidelines for prevention of catheter-associated urinary tract infections (Table I).30

Culturing urine samples obtained from the lumen of urinary catheters often grows more species than are actually present in the bladder. It is often recommended that a urinary catheter be removed and replaced with a new catheter before obtaining urine cultures.31,32 Studies of silver- and antibiotic-coated catheters in relation to the development of UTI have reported mixed results. In addition, none of these studies included nursing home residents or chronic catheter users.33 At the present time, there are not enough data to justify recommending the utilization of coated catheters for UTI prevention.
TREATMENT OF UTI IN THE NURSING HOME
Asymptomatic bacteriuria should not be treated. The organisms (frequently E. coli) often lose their virulence and become susceptible to the bactericidal effect of normal human plasma.9 Treatment of symptomatic UTI should not be delayed while waiting for culture and sensitivity results. It may be helpful to start empiric treatment, taking into account previous urine culture and sensitivity results and the antibiotic sensitivity pattern in the facility. There is no consensus on the duration of antibiotic course needed to treat a urinary tract infection in nursing home residents. Generally speaking, elderly women with uncomplicated UTI may be treated with a 10-day course of antibiotic therapy while elderly men may need to receive a 14-day course of antibiotic therapy. Abbreviated courses of antibiotic therapy (< 7 days) to treat a UTI in elderly nursing home residents are generally not recommended because of relatively high rates of treatment failure and infection relapse. Patients with pyelonephritis or urosepsis are generally treated for a minimum of 14 days. Parenterally administered antibiotics (intravenous or intramuscular) may need to be prescribed if the resident is not able to take antibiotics orally (eg, because of vomiting).34
Takahashi and colleagues35 studied 196 elderly women (22% were nursing home residents and 78% were community-dwelling elderly) in Olmsted County, Minnesota, and reported that nursing home residents with a UTI were often treated for longer duration than their community-dwelling counterparts. Ninety-eight percent of nursing home subjects received antibiotic courses for 7 days or longer compared to 77% of community-dwelling subjects. Nursing home subjects were also 5.1 times more likely than community-dwelling subjects to be treated for 10 days or longer. The study also showed that the frequency of infection relapses and adverse events as a result of the antibiotic therapy were greater in nursing home subjects compared to community-dwelling subjects.
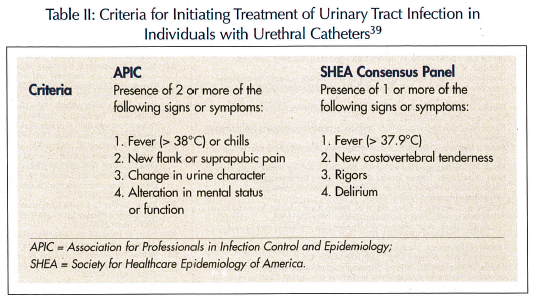
Although the use of antibiotic prophylaxis has been reported to decrease the incidence of UTI in younger women,36 this practice was not studied in nursing home residents, and there is a concern that such practice may lead to the development of resistant pathogens. The use of prophylactic antibiotics to prevent urinary tract infection in nursing home residents with indwelling urinary catheters should also be avoided, as it has not been shown to prevent bacteriuria or infection and may lead to the emergence of antibiotic-resistant pathogens.37,38 Table II lists recommendations from the APIC and the Society for Healthcare Epidemiology of America (SHEA) regarding initiating treatment for UTI in patients with urinary catheters.39 Urologic consultation should be sought when obstructive uropathy, calculi, abscesses, or genitourinary tract anatomic abnormalities are suspected. After treating a UTI, it is not recommended to order urine culture to document clearing of the infection in the absence of symptoms.
See Internet Journal of Geriatrics and Gerontology published by Internet Scientific Publications at ispub.com for more information on urinary tract infections (Volume 1, Number 4, 2004).










