Immunization and Screening for Infectious Disease: Health Care Workers in Long-Term Care
INTRODUCTION
Residents of long-term care (LTC) facilities are at increased risk of developing infectious diseases. Health care workers (HCWs) in LTC facilities are both a potential source of infection and at risk for contracting infections from residents of the facility. Employee health is an important component of infectious control in LTC. Medical directors, directors of nursing, and human resources personnel, among others, may be called upon to develop infection control and screening protocols for their staff. There are guidelines that address these issues for HCWs in general.1,2 The needs of HCWs in LTC are not substantially different, but there are several areas that require emphasis.
INFLUENZA
Residents of LTC facilities are at increased risk of being infected with influenza and of suffering serious influenza-related complications. Because employees of LTC facilities live in the community, are likely to be in contact with others who are infected with influenza during a community outbreak, and because they may have close personal contact with residents, they are a mechanism of entry for influenza into a LTC facility and its spread within the facility. Influenza vaccination is effective in preventing HCWs from becoming infected with influenza, and high rates of employee vaccination have been demonstrated to reduce influenza-related mortality in long-term care residents.3
Numerous studies indicate that influenza immunization rates for HCWs are low. Employees may be reluctant to be immunized because of the perceived discomfort associated with the inoculation and/or concerns about adverse effects from the vaccine. Employees should be educated about influenza and the potential risks to themselves and the residents. Employee vaccination rates have increased in facilities that educate staff about influenza and emphasize the safety and health benefits of vaccination for staff and residents of the facility. Health care workers should be informed of the potential impact of the vaccination on their own health, the prevention of influenza in their facility, and the prevention of morbidity and mortality for the residents.4 Influenza vaccination should be offered to all employees free of charge on an annual basis. Long-term care facilities should develop individualized strategies to increase influenza vaccination rates among their employees. Facilities should monitor immunization rates for their employees on an annual basis. Egg allergy is a contraindication to influenza vaccination.
There is at least a theoretical concern about using the live, attenuated, cold-adapted, trivalent influenza nasal vaccine for HCWs in LTC facilities. This is a live attenuated vaccine, and there is a concern that the virus, if transmitted to an immunocompromised patient, could cause influenza. Until further data are available on its safety, the nasal influenza vaccine should not be given to HCWs working in LTC facilities.
HEPATITIS B
Health care workers are at risk of contracting the hepatitis B virus (HBV). The risk for acquiring HBV infection from occupational exposures is dependent on the frequency of percutaneous and permucosal exposures to blood or body fluids containing blood. Depending on the tasks he or she performs, any health care worker may be at high risk for HBV exposure. Health care workers who have a reasonable expectation of being exposed to blood on the job should be offered hepatitis B vaccine.2 The Occupational Safety and Health Administration (OSHA) Federal Standard requires employers to offer hepatitis B vaccine free of charge to employees who are occupationally exposed to blood or other potentially infectious materials.
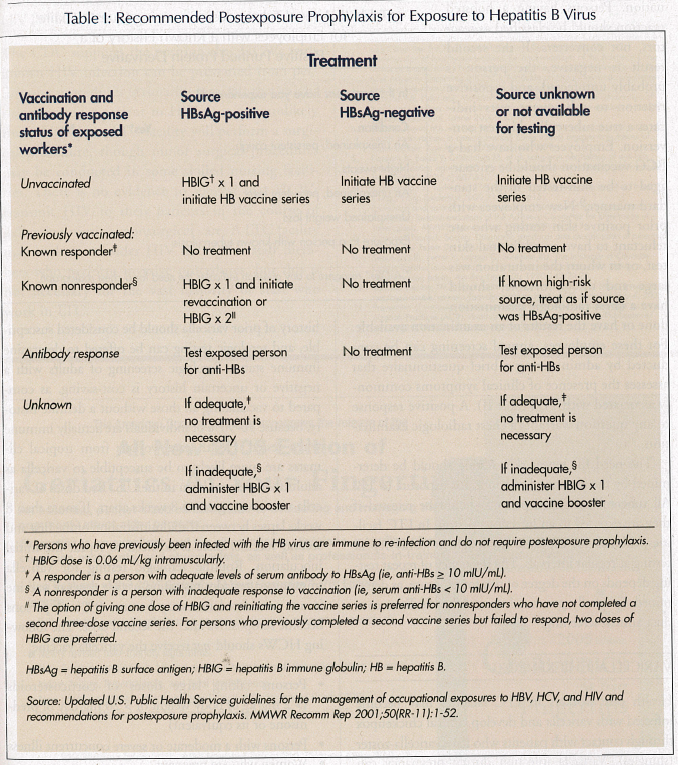
Prevaccination serologic screening for previous infection is not indicated for persons being vaccinated because of occupational risk. Post-vaccination testing for antibody to hepatitis B surface antigens (anti-HBs) response is indicated for HCWs who have blood or resident contact and are at ongoing risk for injuries with sharp instruments or needlesticks. Knowledge of antibody response aids in determining appropriate postexposure prophylaxis. Postvaccination anti-HBs immunology 1-2 months after completion of vaccination is recommended. Longitudinal immunity testing and the administration of booster doses are not considered necessary. Vaccine-induced antibodies to HBV decline gradually over time.5 However, studies among adults have demonstrated that, despite declining serum levels of antibody, vaccine-induced immunity continues to prevent clinical disease or detectable viremic HBV infection. For this reason, routine periodic serologic testing—at least in areas with low level of endemic hepatitis B—is not recommended after an initial test to evaluate the immunologic response to vaccination. If an employee has experienced a potential exposure to HBV, the approach described in Table I is recommended.
TUBERCULOSIS
Long-term care residents are at increased risk of developing Mycobacterium tuberculosis (TB). Outbreaks of TB have been reported in skilled nursing facilities.6 Long-term care employees are a potential reservoir of TB and are at risk for contracting TB following close contact with infected residents. The Centers for Disease Control and Prevention (CDC) considers residents and employees of long-term care residential facilities to be among those at high risk of developing clinical TB.7,8 Foreign-born persons are also included in the high-risk categorization. In some parts of the United States, many direct-care providers in LTC facilities were born in countries with endemic TB. Tuberculosis screening helps detect employees who may have clinical or latent tuberculosis, and also allows the facility to identify employees who may have been exposed to TB if a clinical case is subsequently identified in the facility.
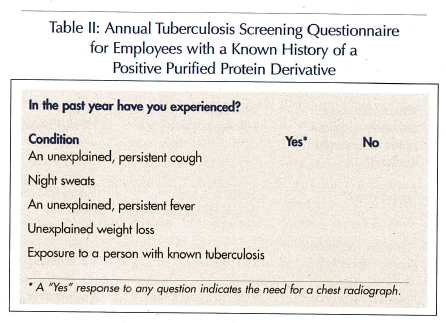
Tuberculin skin testing is the standard method for identifying persons infected with TB. The Mantoux test (ie, the intracutaneous administration of 5 units of purified protein derivative [PPD] tuberculin [TU]) best detects infection. An induration of > 10 mm is classified as positive in all employees of nursing homes and other LTC facilities for the elderly.7,8 In areas with high rates of tuberculosis infection, LTC facilities should consider using a two-step skin test at the time of initial employment. When tuberculin skin testing of adults is repeated periodically, as in employee health or institutional screening programs, an initial two-step approach can reduce the likelihood that a boosted reaction will be misinterpreted as a recent infection. If the first tuberculin test result is negative, a second 5-TU test should be administered 1-3 weeks later. A positive second result probably indicates boosting from a past infection or prior Bacillus Calmette Guérin (BCG) vaccination. Persons having a boosted reaction should be classified as reactors, not converters. If the second result is negative, the person is probably uninfected, and a positive reaction to subsequent tests indicates a true tuberculin skin test conversion. Employees who have had a BCG vaccination should be encouraged to be skin-tested in the standard manner.9 New employees with prior positive skin testing who are reluctant to have an additional skin test, or in whom the induration was large and uncomfortable, should have a chest radiologic examination done or have the results of an examination available. For these employees, annual screening can be conducted by administering a brief questionnaire that assesses the presence of clinical symptoms commonly associated with TB (Table II). A positive response to any question warrants a chest radiologic examination.
The need for repeat skin testing should be determined by the likelihood of continued exposure to TB. All tuberculin-negative persons should be retested if they are exposed to an infectious person. In LTC facilities, the risk for exposure is enough to justify repeat testing at regular intervals. The frequency of repeat testing depends on the degree of risk for exposure, as determined by locally generated data. Most facilities conduct annual screening.
VARICELLA (CHICKENPOX)
Health care workers in LTC facilities may become infected with varicella and develop clinical chickenpox through contact with patients who have varicella-zoster (shingles). Varicella infection during pregnancy can result in fetal abnormalities. Data available to date indicate that in the health care setting, a positive history of disease is a reliable predictor of positive immune status.10,11 Among tested health care workers, more than 97-99% of those with a positive history had antibodies when tested. Employees who do not have a convincing history of prior varicella should be considered susceptible, and serologic testing can be offered to determine immune status. Serologic screening of adults with a negative or uncertain history is cost-saving, as compared to vaccinating all those without a definite history, because 70-90% of individuals are actually immune when tested. Health care workers from tropical climates are more likely to be susceptible to varicella as adults than persons born in the U.S. Two doses of varicella vaccine are given 4-8 weeks apart. If more than 8 weeks lapses between the administration of the first and second vaccine, there is no need to repeat the initial inoculation. Routine serologic testing for varicella immunity after administration of two doses of vaccine is not considered necessary because 99% of persons become seropositive after the second dose. The following HCWs should not receive the varicella vaccine:
• Persons taking large doses of corticosteroids (> 2 mg/kg of body weight or > 20 mg/day of prednisone or its equivalent)
• Persons with a moderate or severe concurrent illness
• Women who are pregnant
• Persons who have received blood products (such as whole blood or immune globulin) during the previous 5 months
• Persons with a family history of congenital hereditary immunodeficiency in first-degree relatives, unless they are known to be immunocompetent.
HIV INFECTION
The CDC supports the position that HCWs with known HIV infection can be prevented from performing procedures (primarily surgical) that might risk exposing a patient to HIV. It is very unlikely that a HCW in a LTC facility will perform a surgical procedure, though minor surgical procedures may be conducted in some skilled nursing facilities. There is no evidence to suggest that HCWs transmit HIV to their patients in the course of delivering routine, nonsurgical care. A LTC facility may wish to consider HIV testing for staff members who perform invasive procedures, but this is not necessary for the vast majority of staff who work in LTC.










