Pain Management in a Long-Term Care Setting: An Interdisciplinary Approach
INTRODUCTION
Nearly 1.5 million people live in the nation’s 16,000 nursing care facilities.1 More than 50% of those residents have three or more chronic conditions and require seven to eight prescribed medications.2-4 With an increasing number of chronic conditions, there is an associated limitation in activity level and a higher incidence of associated pain. Common conditions that are associated with pain in nursing facility residents include arthritis, depression, dementia, anxiety, and cancer.5 Chronic 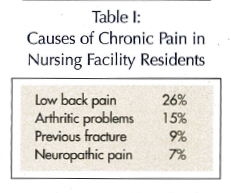 pain is defined as any pain that persists for greater than one month beyond the healing of an inciting injury, pain that is associated with a lesion or disorder that is not expected to heal, or pain from any cause that recurs frequently over a period of months.6,7 Therefore, chronic pain does not have to be constant; rather it can occur as intermittent flare-ups that produce disturbing pain. Chronic pain occurs in 25-50% of community-dwelling elderly and in 45-80% of nursing facility residents (Table I). It is estimated that less than 50% of nursing facility residents who suffer from chronic pain are adequately assessed and treated.4 Minimum Data Set (MDS) data from 11 states with a total of 120,000 patient records reviewed demonstrated that 15% of residents were experiencing persistent pain. Of these residents, 25% were new admissions to the nursing facility. Of all the residents assessed, over 40% were still in pain at 60- and 180-day reviews.8 Adequate assessment and treatment of chronic pain in nursing facility residents has been associated with improvement in activities of daily living and function.9 The inherent difficulties of pain assessment and management due to cognitive impairment, and resident and staff attitudinal barriers have been previously described.10,11
pain is defined as any pain that persists for greater than one month beyond the healing of an inciting injury, pain that is associated with a lesion or disorder that is not expected to heal, or pain from any cause that recurs frequently over a period of months.6,7 Therefore, chronic pain does not have to be constant; rather it can occur as intermittent flare-ups that produce disturbing pain. Chronic pain occurs in 25-50% of community-dwelling elderly and in 45-80% of nursing facility residents (Table I). It is estimated that less than 50% of nursing facility residents who suffer from chronic pain are adequately assessed and treated.4 Minimum Data Set (MDS) data from 11 states with a total of 120,000 patient records reviewed demonstrated that 15% of residents were experiencing persistent pain. Of these residents, 25% were new admissions to the nursing facility. Of all the residents assessed, over 40% were still in pain at 60- and 180-day reviews.8 Adequate assessment and treatment of chronic pain in nursing facility residents has been associated with improvement in activities of daily living and function.9 The inherent difficulties of pain assessment and management due to cognitive impairment, and resident and staff attitudinal barriers have been previously described.10,11
AN INTERDISCIPLINARY APPROACH TO CHRONIC PAIN MANAGEMENT
Hearthstone Nursing Facility of Northern Nevada is a 125-bed facility that has an active skilled/subacute care unit and long-term custodial residents. In the autumn of 2000, the management of Hearthstone decided to initiate an interdisciplinary and coordinated approach to patient care.12 This effort involved medical providers, pharmacists, nursing staff, physical/occupational therapists, speech pathologists, social workers, dietitians, certified nursing assistants, and administrators agreeing to work together toward a common goal: the residents’ well-being.
Through a coordinated drug review process, the use of analgesic medications for the control of breakthrough pain was identified as an area in need of further quality improvement. The care team identified that many residents were being admitted from the acute care setting with pain-related diagnoses (eg, cancer, fractures), with no mention of pain assessment or management. In addition, there were established residents within the facility that had associated behavioral symptoms and declines in physical capabilities over time due to painful conditions. A decision was made to develop and implement a comprehensive assessment and treatment program to address both acute and chronic painful conditions.
In the spring of 2001, the assessment and treatment of painful conditions became a component of the facility-wide quality improvement program. The clinical practice guideline developed by the American Medical Directors Association (AMDA) and recommendations from the American Geriatrics Society (AGS) Consensus Panel on the management of chronic pain in older persons 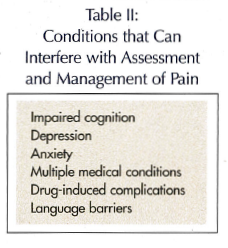 were incorporated into this facility-wide program.13,14 We selected the quality measures gathered through the resident assessment, as reported in the MDS, at specific intervals during their stay as a means of monitoring the effectiveness of the program. The quality measures included the percentage of residents who have moderate-to-severe pain or excruciating pain at any frequency on the target assessment (chronic pain measure), and the percentage of short-stay residents at 14-day assessment with daily moderate pain or excruciating pain at any frequency (acute pain measure).15
were incorporated into this facility-wide program.13,14 We selected the quality measures gathered through the resident assessment, as reported in the MDS, at specific intervals during their stay as a means of monitoring the effectiveness of the program. The quality measures included the percentage of residents who have moderate-to-severe pain or excruciating pain at any frequency on the target assessment (chronic pain measure), and the percentage of short-stay residents at 14-day assessment with daily moderate pain or excruciating pain at any frequency (acute pain measure).15
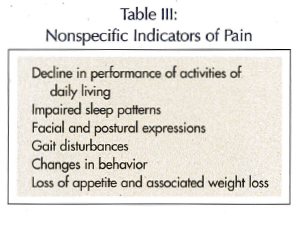
Clinical conditions that can interfere with the assessment and management of pain include impaired cognition, depression, anxiety, multiple medical conditions, multiple medications, drug-induced complications, and language barriers (Table II). In the long-term care setting the clinicians must often be on the lookout for nonspecific indicators of pain. Examples include changes in activities of daily living, impaired sleep patterns, facial and postural expressions, gait disturbances, and changes in behavior (Table III).
 An educational program was developed and incorporated into the ongoing staff development program at Hearthstone. The focus of the program is that the day-to-day frontline caregivers—the certified nursing assistants, licensed nursing staff, and therapists—are truly the eyes and ears of a successful program. The program included the various causes of painful conditions, how to assess and monitor the treatment of pain, and an attempt to dispel some of the myths about pain and aging (Table IV).
An educational program was developed and incorporated into the ongoing staff development program at Hearthstone. The focus of the program is that the day-to-day frontline caregivers—the certified nursing assistants, licensed nursing staff, and therapists—are truly the eyes and ears of a successful program. The program included the various causes of painful conditions, how to assess and monitor the treatment of pain, and an attempt to dispel some of the myths about pain and aging (Table IV).
As Hearthstone staff began to learn more about the various causes of painful conditions and possible treatment 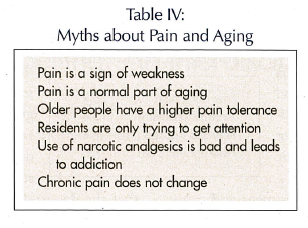 options, they saw the opportunity to make a profound change in the residents’ quality of life. This collaborative approach to patient care has resulted in a comprehensive pain management program. Team members now seek out information about the assessment and treatment of pain for individual residents. Weekly standards-of-care meetings are held with the interdisciplinary team. The team reviews each resident’s plan of care, shares and addresses patient care needs, communicates process barriers, and creates improvement strategies. Observations of each resident’s response to treatment are shared with the other team members.
options, they saw the opportunity to make a profound change in the residents’ quality of life. This collaborative approach to patient care has resulted in a comprehensive pain management program. Team members now seek out information about the assessment and treatment of pain for individual residents. Weekly standards-of-care meetings are held with the interdisciplinary team. The team reviews each resident’s plan of care, shares and addresses patient care needs, communicates process barriers, and creates improvement strategies. Observations of each resident’s response to treatment are shared with the other team members.
OUTCOMES
At a statewide and national reporting level, Hearthstone has demonstrated ongoing success in the areas of pain 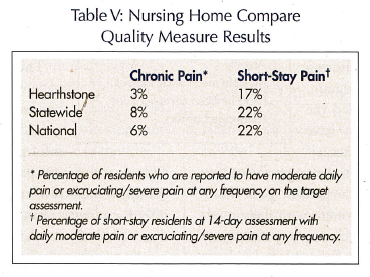 assessment and management, as reflected in the Nursing Home Compare quality measure results (Table V). Prior to initiation of the facility-wide quality improvement program, Hearthstone scores were consistently in the 7% and 20% range for chronic and short-stay pain categories, respectively. Hearthstone has recently been recognized by HealthInsight, the State Quality Improvement Organization for Nevada and Utah, for its innovative approach to pain management for the period of January 2003 through July 2004.
assessment and management, as reflected in the Nursing Home Compare quality measure results (Table V). Prior to initiation of the facility-wide quality improvement program, Hearthstone scores were consistently in the 7% and 20% range for chronic and short-stay pain categories, respectively. Hearthstone has recently been recognized by HealthInsight, the State Quality Improvement Organization for Nevada and Utah, for its innovative approach to pain management for the period of January 2003 through July 2004.
SUMMARY
The development of an interdisciplinary approach to the assessment and management of both acute and chronic pain has resulted in a favorable quality measurement within our nursing facility. The residents, staff, and family members have become part of this program and share in the results. The use of frontline staff in the ongoing assessment of pain, evaluation of response to treatment, and reporting within an interdisciplinary model has improved facility-wide communication and patient care. We have identified aspects of patient care that can be affected both positively and negatively through the implementation of this program. The assessment and adequate treatment of pain has the potential of reducing falls, fractures, behavioral symptoms including depression, and the eventual decline in activities of daily living. At the same time, the aggressive treatment of pain could potentially worsen cognitive impairment, incontinence, fecal impaction, and pressure sores. These areas require ongoing monitoring and the continuing education of residents, staff, family members, and surveyors. The use of Nursing Home Compare quality measures for moderate-to-severe pain has provided an opportunity for the staff of Hearthstone to be acknowledged for their efforts in improving the recognition and management of residents with painful conditions. This has been a stimulus to incorporate additional quality measurement data into our ongoing quality improvement activities.










