The Effects of Topical and Systemic Beta Glucan Administration on Wound Healing Impaired by Corticosteroids
Abstract: Background. Corticosteroid hormones are widely used to treat a variety of diseases. Corticosteriods have been shown to impair wound healing, which has become a serious clinical problem in wound care. The present study was designed to evaluate the efficacy of topical and systemic beta glucan administration on wound healing impaired by corticosteroids. Methods. Wistar albino rats were used for the incision and excision wound models. Percentage of wound contraction, epithelialization period, hydroxyproline level, histopathological examination, and tensile strength were evaluated. Results. Although both systemic and local administration of beta glucan enhanced percentage wound contraction, improved epithelialization time, tensile strength, and elevated hydroxyproline level, systemic administration was found to be more effective. Conclusion. These results indicate that systemic and topical beta glucan improve wound healing that has been impaired by corticosteroids, and that systemic administration is more effective than topical application.
Address correspondence to: Celal Cerci, MD Modernevler 3103 Sokak No. 16 32200 Isparta Turkey Phone: 90 505 2933423 E-mail: celalcerci@yahoo.com
Corticosteroids affect almost every phase of wound healing and delay the appearance of inflammatory cells, fibroblasts, and the deposition of ground substance, collagen, regenerating capillaries, contraction, and epithelial migration.1 Beta glucan, a complex carbohydrate, is found in the cell walls of yeast, fungi, and cereal plants, and is known as a potent macrophage stimulator. Topical and systemic administration of beta glucan enhances wound healing by increasing macrophage infiltration into the wound area, and by stimulating tissue granulation, collagen deposition, re-epithelization, and tensile strength. 2–7 Beta glucan directly affects the chemotactic capacity of circulating neutrophils through a p38 mitogen-activated protein kinase-dependent mechanism and potentiates antimicrobial host defense. 8 Macrophage cells have an important role in wound repair; 9 they are pattern recognition receptors for glucans on mammalian macrophages, 10 and the ligation of glucan by its cognate receptors on macrophages modulates functional activity of the cells. 11 The effect of glucan on wound repair also involves macrophage release of wound growth factors with subsequent modulation of fibroblast activity, which includes collagen biosynthesis. 2–4 Kougias et al12 have reported on the glucan binding sites for normal human dermal fibroblasts. According to the Kougias findings, it can be suggested that glucans can directly modulate the functional activity of human fibroblasts. Glucan also stimulates collagen biosynthesis in cultured normal human dermal fibroblasts by activating the modulation of the reparative process. 13 During wound healing, glucan also stimulates both type I and III collagen production by activating fibroblasts, which increases wound tensile strength. 14,15 This experimental study was designed to evaluate the efficacy of topical and systemic beta glucan administration on wound healing impaired by corticosteroids using both excisional and incisional wound models.
Materials and Methods
Animals. Eighty adult Wistar-albino rats weighing between 200 g–250 g were used. Guidelines for the humane use of laboratory animals were strictly adhered to throughout the study. The animals were acclimatized for 1 week to the laboratory conditions prior to experimental manipulation. They had free access to standard laboratory chow and water ad libitum. The animals (N = 80) were divided into 4 equal groups (n = 20). Subcutaneous 20-mg/kg methylprednisolone acetate was administered at the time of the surgery to all of the animals except those in group 1. This time point was chosen since the inhibitory effect of corticosteroids on wound healing is most pronounced when administration of the hormone begins just prior to the onset of inflammation in the healing process. 1 The beta glucan that was used in this study (Imuneks, MN Pharmaceuticals, Turkey) was 1.3–1.6 beta-D-glucan in microparticulate form, which was prepared from the Saccharomyces cerevisiae yeast. The topical (5%) beta glucan cream was also provided by MN Pharmaceuticals, Turkey. Group 1: Control group; no treatment. Group 2: Corticosteroid only. Group 3: Corticosteroid + topical beta glucan group. A thin layer of beta glucan cream was applied topically twice a day, covering the entire wound area until the sacrification. Group 4: Corticosteroid + systemic beta glucan group: 50 mg/kg/day beta glucan was administered by intragastric gavage once a day starting prior to surgery and continued until the sacrification. The 4 groups were divided into 2 subgroups: excision and incision models. Excisional wound model. All animals in each group were anesthetized by ketamine (1 mL/kg of body weight) before wound creation. A full-thickness excisional wound (2-cm wide and 0.2-cm deep) was created with a surgical blade and was left undressed to the open environment. All animals were housed individually during the study period. Topical and systemic beta glucan therapy was maintained until the wound was completely healed. Wound contraction and wound closure time was monitored. Wound contraction percentage was measured 2 days after wound creation, and every 2 days thereafter until study completion. Wound contraction (%) was determined using the following formula: Wound area was measured at each 2-day interval by tracing the wound margin using transparent paper. The healed area was calculated by subtracting from the original wound area. The number of days required for falling of eschar with no residual raw area was considered the endpoint of epithelialization. The healed tissue specimens from experimental and control group animals were taken using an 8-mm punch and were processed for histological study. Tissue specimens were stained with hematoxylin-eosin, and sections were qualitatively assessed under a light microscope and observed in respect of fibroblast proliferation, collagen formation, angiogenesis, and epithelialization. Hydroxyproline level was measured by the Woessner method from granulation tissue at 540 nm in a spectrophotometer. 16 Incisional wound model. All animals in each group were anesthetized by ketamine (1 mL/kg of body weight) before wound creation. Two long, paravertebral incisions were made through the skin about 1.5 cm from midline on each side of the depilated back. Wounds were closed with 3-0 polypropylene continuous sutures. The sutures were removed on the seventh day. Tensile strength was measured on the 10th post-wounding day using a digital tensiometer.
Statistical Analysis
Results were expressed as mean ± SD and analyzed using the Mann-Whitney U test; P < 0.05 was considered statistically significant.
Results
Corticosteroid administration significantly prolonged the epithelialization period, and decreased tensile strength, hydroxyproline levels, and percentage wound contraction compared to the control group (P < 0.05). Systemic and local administration of beta glucan in the impaired wound model significantly improved the wound healing process in the excision and incision models. Both systemic and local administration of beta glucan significantly enhanced percentage wound contraction on days 2, 10, and 20 (Table 1). 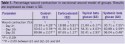 Epithelialization period of control, corticosteroid, topical beta glucan, and systemic beta glucan groups were (in days): 13.4 ± 0.12, 15.18 ± 0.24, 11.92 ± 0.17, and 9.62 ± 0.15, respectively (Figure 1). The differences between the 4 groups were statistically significant (P < 0.05). Tensile strength was measured as: 321.02 g ± 40.12 g (control), 244.03 g ± 48.81 g (corticosteroid), 330.12 g ± 48.3 g (topical beta glucan), and 392.27 g
Epithelialization period of control, corticosteroid, topical beta glucan, and systemic beta glucan groups were (in days): 13.4 ± 0.12, 15.18 ± 0.24, 11.92 ± 0.17, and 9.62 ± 0.15, respectively (Figure 1). The differences between the 4 groups were statistically significant (P < 0.05). Tensile strength was measured as: 321.02 g ± 40.12 g (control), 244.03 g ± 48.81 g (corticosteroid), 330.12 g ± 48.3 g (topical beta glucan), and 392.27 g 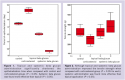 ± 69.89 g (systemic beta glucan [Figure 2]). The difference between the corticosteroid group and beta glucan groups was significant (P < 0.05). The difference between the topical and systemic beta glucan groups was also significant (P < 0.05). In control, corticosteroid, topical beta glucan, and systemic beta glucan groups, hydroxyproline levels were measured as: 0.173 µg/mg ± 0.011 µg/mg, 0.146 µg/mg ± 0.111 µg/mg, 0.186 µg/mg ± 0.129 µg/mg, and 0.304 µg/mg ± 0.177 µg/mg, respectively (Figure 3). Significant differences were detected between the corticosteroid group and beta glucan group. A significant difference was also found between topical and systemic beta glucan groups (P < 0.05).
± 69.89 g (systemic beta glucan [Figure 2]). The difference between the corticosteroid group and beta glucan groups was significant (P < 0.05). The difference between the topical and systemic beta glucan groups was also significant (P < 0.05). In control, corticosteroid, topical beta glucan, and systemic beta glucan groups, hydroxyproline levels were measured as: 0.173 µg/mg ± 0.011 µg/mg, 0.146 µg/mg ± 0.111 µg/mg, 0.186 µg/mg ± 0.129 µg/mg, and 0.304 µg/mg ± 0.177 µg/mg, respectively (Figure 3). Significant differences were detected between the corticosteroid group and beta glucan group. A significant difference was also found between topical and systemic beta glucan groups (P < 0.05).  Histopathological examination revealed a significant increase in collagen deposition, fibroblasts, and macrophages in beta glucan-treated groups. Collagen deposition was especially significant in the systemic beta glucan group (Figures 4–6).
Histopathological examination revealed a significant increase in collagen deposition, fibroblasts, and macrophages in beta glucan-treated groups. Collagen deposition was especially significant in the systemic beta glucan group (Figures 4–6). 
Discussion
Among factors thought to impair wound healing, corticosteroids are commonly investigated, and their harmful effects to various tissues have been reported. 17–21 Corticosteroids are widely used in the treatment of various diseases for their anti-inflammatory and immunosuppressive functions. In addition to therapeutic function, their adverse effects became evident and impaired wound healing during glucocorticoid therapy had become a serious clinical problem. 1,17–20 Corticosteroids are known to cause a significant decrease in collagen fibers, thickening of the skin, and inhibition of fibroblast growth and granuloma formation in scar tissue in animal models. 21 Fibroblasts, one of the most important cellular components of connective tissue, are the target cells for corticosteroids in wound healing processes. 21 Corticosteroid treatment also causes a decrease in leukocyte infiltration and decreased macrophage formation. Wound healing can be significantly retarded during corticosteroid treatment because both macrophages and leukocytes participate in the destruction and phagocytosis of injured tissue, debris, and fibrin. 22–25 Wound healing consists of phases such as granulation, collagenation, collagen maturation, and scar maturation that are concurrent, but independent. It is well known that topical and systemic beta glucan administration enhances the wound-healing process in different pathways. The results of the present study showed that both topical and systemic beta glucan administration significantly improved wound-healing activity; systemic administration was more effective than topical application. Dinc et al26 also demonstrated that oral administration of beta glucan significantly improved the healing of an anastomotic wound that had been impaired by long-term corticosteroid administration. Mechanisms by which glucan enhances wound repair have been reported. 10–12 There are pattern recognition receptors for glucans on mammalian macrophages. 10 Ligation of glucan by its cognate receptors on macrophages modulates functional activity of the cell. 11 It is highly conceivable that the effect of glucan on wound repair involves macrophage release of wound growth factors with subsequent modulation of fibroblast activity, including collagen biosynthesis. 2–4 Kougias et al12 reported the presence of glucan binding sites on dermal fibroblasts that can be the evidence of modulation of the functional activity of human fibroblasts by glucan. During wound healing, fibroblasts produce and deposit large quantities of matrix protein, predominantly type I and III collagen, which increase the tensile strength of the wound; 14,15 glucan stimulates both type I and III collagen genes. 13 In the wound model impaired by corticosteroid, it was observed that systemic administration and local application of beta glucan significantly increased tensile strength, but that systemic administration was more effective. Leibovich et al25 demonstrated that topical application of glucan to experimental wounds in mice resulted in mobilization and activation of macrophages to the wound area, which in turn enhanced proliferation of fibroblasts and capillaries, which ultimately accelerated wound repair. 25 Our histopathological findings were similar to Leibovich’s in both topical and systemic groups, but the effects of systemic administration of beta glucan seemed more powerful than topical application on fibroblast proliferation. Hydroxyproline, a collagen composed of amino acids, is the major component of extracellular tissue that provides both strength and support. Measurement of the hydroxyproline could be accepted as an index for collagen turnover. In the present study, corticosteroid administration decreased hydroxyproline content of the wound significantly when compared to the control group and topical and systemic beta glucan treatment was increased hydroxyproline levels.
Conclusion
Systemic and topical administration of beta glucan significantly stimulated wound contraction, increased incision tensile strength, improved epithelialization, and elevated hydroxyproline levels in rats that had received corticosteroid treatment. Further clinical studies are needed, but it may be suggested that beta glucan be applied, both locally and systemically, to patients receiving steroid therapy in order to improve wound healing. From the Suleyman Demirel University, Isparta, Turkey
















