Wound Center Facility Billing: A Retrospective Analysis of Time, Wound Size, and Acuity Scoring for Determining Facility Level
Dr. Fife and Mr. Walker disclose they have financial interest in Intellicure, Inc. and the Intellicure Clinical Documentation & Facility Management Software. This article was developed and submitted for publication with the generous volunteer support of the Association for the Advancement of Wound Care members.
Introduction
Outpatient wound center facility reimbursement for Medicare beneficiaries is defined by the Centers for Medicare and Medicaid Services (CMS) in the Hospital Outpatient Prospective Payment System (HOPPS). (Physician reimbursement by the CMS is determined by the 1995-1997 Medicare guidelines for physician documentation and will not be discussed in this paper.) The HOPPS, published on April 7, 2000 in the Federal Register,1 was intended to revise the outpatient payment system for hospital clinic and emergency departments, as well as for all hospital outpatient departments that did not have an existing billing schedule, such as outpatient cancer centers or pain management clinics. Wound care centers were instructed to use three sets of the five Evaluation and Management (E&M) Codes: new patients – codes 99201 to 99205; consults – codes 99241 to 99245; and established/follow-up – codes 99211to 99215.1 Although the CMS directed facilities to bill using all of these classes of codes, only three payment groups existed. They are known as Ambulatory Patient Classification (APC) Codes 600, 601, and 602; the assigned payments were approximately $44, $52, and $82, respectively (approximate because several other factors impact the actual payment, such as wage index and locality).
In addition, as specified in the 2000 Federal Register,1 each wound facility was expected to “develop a system for mapping the provided services furnished to the different levels of effort represented by the codes.” Provided that the services were medically necessary and properly documented and that the facility was following its own developed system, the CMS would assume the facility was in compliance with reporting requirements. At the same time, the CMS emphasized that the intensity of facility visits and reporting codes should be based on “an internal assessment of the relevant charges for those codes as opposed to failing to distinguish between low- and mid-level visits because the payment is the same.” One of the CMS goals through HOPPS was to study billing information to establish a database for revising weighing factors and other payment adjustments in future years.
“Time” was readily adopted by wound care clinics as a means of assessing the charged level of service for each patient visit. While a time-based analysis is an easy system to develop and subsequent billing codes are easy to calculate, this system rewards inefficiency. Although more complex wound care activities require more time, a system based on a subjective assessment of time spent could result in healthcare workers justifying a billed level of service that is inappropriately high compared to the actual work provided.
Recognizing this problem, the CMS announced its intention to provide specific guidance for determining level of service. In 2004, the American Hospital Association and the American Health Information and Management Association suggested to the CMS that facility level of service be based on wound size.2 The model for this idea was the reimbursement methodology for acute wounds, a familiar concept in emergency departments (EDs). In acute wound repair, a direct relationship between wound size and work exists because these wounds are usually managed by surgical suturing – coding is based on the size of the ultimate repair of the wound and the type of repair (simple, intermediate, and complex) performed.
The wound-size proposal was based on a three-tiered size system in which the wound sizes chosen appear to have been arbitrarily determined by the CMS with possible input from consultants and were as follows: Level 1: <25 cm2; Level 2: 25.1 to 50 cm2; and Level 3: >50 cm2. Because this system had never been applied to chronic wound management, little was known about its effects on outpatient wound centers; critical information such as the average size of various chronic wounds was unknown. Furthermore, it is generally accepted that unlike the situation in acute wound management, there is no demonstrated relationship between chronic wound care level of work and wound size. For example, patients with chronic wounds often are severely debilitated with multiple, complex medical problems and even small wounds can require extensive irrigation, packing, or complex bandaging. An economic study by Pompeo3 (N = 240) utilizing a computerized system of wound tracking, for example, found that patients with the highest level of “wound burden” (defined as the degree to which a wound was related to costs) had significantly higher wound and total stay costs.
In addition, the size-based system did not include depth assessment; small wounds open to tendon or bone and requiring particularly complex interventions cannot be defined using a system based on surface area alone. Moreover, patients with chronic wounds can require extensive education regarding offloading, edema management, diet, or self wound care. For all these reasons, some method of assessing the specific elements of actual work provided needed to be developed in the chronic wound care setting.
While many healthcare systems in the US have instituted or adopted Electronic Patient Records (EPRs),4-5 Computerized Physician Order Entry (CPOE),6-7 and Clinical Data Support Systems (CDSS),8-9 the level of detail and relevance of these systems to wound care centers are often unsatisfactory. Business corporations have developed systems, commonly known as Activity-Based Cost Accounting (ABC Accounting),10 that more accurately measure unit costs associated with procedures and products and these techniques have been adapted in the wound care arena.11 However, in the situation under consideration, simple ABC Accounting is not sufficiently robust to describe the broad range of activities involved in outpatient wound care. A more extensive system that is not based on time or wound size is needed.
In response to the unique demands of wound care documentation, two of the authors have spent more than 10 years developing a group of software programs to handle physician, facility, front office, and managerial documentation requirements. Their corporation (Intellicure, The Woodlands, Tex) now licenses its software for use by hospital-based wound centers. These programs, collectively known as the Intellicure Clinical Documentation & Facility Management Software (ICDFMS), are used not only to manage clinic operations, but also to document all aspects of patient medical data in the form of electronic medical records (EMRs), recording each patient visit in sufficient detail to enable tracking of wound parameters. Using the Structured Query Language (SQL)-associated database with the ICDFMS, the authors conducted a retrospective study to: 1) determine the average sizes and types of the wounds associated with a population of 500 patients who visited an outpatient wound center, 2) compare a time-based to a wound size-based or acuity score-based system, and 3) validate an acuity scoring system for those procedures and products not covered by specific American Medical Association (AMA) Current Procedural Terminology (CPT) codes under HOPPS.
Methods
Software description. The ICDFMS consists of the Intellicure Clinical Documentation software (formerly known as WoundTrak™), HyperTrak™, Inventory Trak™, Front Desk Manager™, and the Intellicure™ Management Database.
The Evaluation and Management (E&M) scoring sheet is intended for use at every patient encounter and comprises 10 major components:
1. Method of arrival
2. Additional resource utilization
3. Patient assessment (history, general physical exam, and risk determination)
4. Patient process (coordination of care, level of processing and education)
5. Problem-focused activities (areas of wound, ulcers, and burns; edema/lymphedema; and ostomy/continence)
6. Focused assessments and interventions
7. General procedures
8. Point-of-care testing
9. Departure instructions
10. Departure disposition.
For each patient visit, the level of service as billed by “time” and documented wound size is collected using the Intellicure Clinical Documentation™ and Front Desk Manager™ software. Time does not differentiate between any type of activity. For example, a person could spend 10 minutes performing a complex debridement or 10 minutes moving a patient from point A to point B.
Data collection for the study. The dataset comprised patients seen between April 2003 and November 2004 at a busy wound center operated by Tomball Regional Hospital, Bryan, Tex, which had used Intellicure software since the center’s inception.
To prevent any confounding due to additional billed services for the time-based billing analysis and to exclude all encounters in which the wound was not measured for the wound-size analysis, the patient visit database was reduced from approximately 12,000 to 5,098 patient visits and included only those visits in which the wound was measured and no separately billable procedures were performed. The study dataset comprised the following variables for each patient encounter:
• Patient ID to facilitate data verification, if needed
• Acuity scores (see next subsection)
• Associated wound sum area (sum of the surface areas of all wound problems documented in a single encounter – the formula proposed by the CMS)
• Time-based level of service (five levels) used for billing.
Development of the Acuity Scoring System. Intellicure began developing an acuity scoring system in response to the 2000 HOPPS publication. The acuity scoring system incorporates elements of a sophisticated ABC methodology for the E&M codes previously described and additional medical information needed for procedure-based billing and inventory control of medical supplies, as well as patient medical history and demographics. Acuity scoring also has been investigated as a billing methodology in trauma patients12 but results of studies evaluating this approach as a measure of work in outpatient wound centers have not been published. While the acuity system continued in development, the clinic continued to bill using a time-based system.
Each E&M procedure listed under the 10 major components was assigned a score (0 to 200 points) based on the authors’ experience. The higher the score, the more work was required to effect the activity or procedure. Not all procedures performed at the clinic were categorized this way because some can be directly billed using the AMA CPT codes listed under HOPPS (eg, Apligraf® [Organogenesis, Inc, Canton, Mass] is charged under a product code and the technical portion of the procedure; wound debridements also have specific billing codes). Only those elements of facility work that were not billable under a specific procedure code were included in the acuity scoring system.
To illustrate the development of the acuity scoring process, the example of dressing changes will be highlighted. Initially, dressing changes were categorized as simple, moderate, and complex and each product was assigned a score from 1 to 10. Thus, gauze – a commonly used product used almost exclusively in drainage control – was given 0 points, while the application of an Unna’s boot compression bandage was assigned 10 points. The application of the compression bandage is covered under CPT code 29580 (Unna’s boot); thus, to avoid duplication and an overestimation of work, 20 points were subtracted from the overall acuity score, reflecting the fact that the application of the bandage is billed with its own CPT code that incorporates an assessment of work for that procedure.
Acuity scores for patient encounters then were refined over several months, periodically plotting the data and searching for the best distribution of points over the activities identified. Table 1 shows the assigned scores for all individual activities grouped under the 10 major E&M categories. 
Acuity score analysis. Statistical analysis was accomplished using back-end SQL data tables under the software company’s Management Database using SPSS© software (Chicago, Ill). The acuity scores were analyzed to determine the mean and standard deviation (SD) and the normality of the distribution evaluated by the Kolmogorov-Smirnov procedure.
Acuity scores were allocated to the five levels of service in two ways. The first was equal membership in each level (membership used to define allocation to specific categories or elements of a mathematical function), which does not depend on the normal distribution property of the acuity scores; thus, it can be described as a non-parametric method. This was defined by rank-ordering the acuity scores and then dividing them into five equal membership groups. Because the acuity scores were designed to measure services provided on an equal value basis, distinguishing first visit encounters from follow-up encounters was not necessary. The second method was based on normal distribution percentiles in which the lowest membership was given to levels 1 and 5, highest membership to level 3, and intermediate membership to levels 2 and 4. This was accomplished by setting the cut-off points at -2, -1, +1, and +2 SD intervals.
The billing rate per point was calculated by dividing the billing rate by the average acuity points for each of the five levels for both approaches. To obtain the uniform billing rate, the mean billing value per point was multiplied by the average acuity point for each level. Finally, the uniform billing rate was multiplied by the number of patients in each level and these figures summed to obtain the total billing based on both approaches.
Analysis by time and correlation with acuity score. Initial and follow-up visit data were analyzed separately by determining the frequency for which various levels of service were billed categorized by the CPT codes 9924x, where x corresponds to 1 to 5 and 99241 would be service Level 1, a “minimal” visit. The relationship between the time level of service and acuity score was analyzed using the Pearson correlation coefficient, which can be employed in this situation.13
Wound diagnosis, size measurement, and correlation with acuity score. A critical problem of billing by wound size is that no universally accepted, reproducible method of wound measurement is available.14 Figure 1 shows the dilemma posed by a typical wound in which the wound surface area, calculated by the longest x widest method, yields 4.50 cm2, while the head-to-toe x perpendicular axis method yields 3.27 cm2, a 38% difference based on the lower figure. Without a standardized, easily implemented measurement method, a reimbursement system based on size would have the probability of encouraging “overestimation” of wound surface area. In this study, all wounds were measured using the longest x widest method of calculation, a rectangular equivalent area.
 The distribution of wound areas was analyzed empirically to determine the best mathematical representation. The correlation between wound area and acuity score was determined using the Pearson correlation coefficient because both variables were normally distributed and calculated for both mathematically transformed and untransformed data.
The distribution of wound areas was analyzed empirically to determine the best mathematical representation. The correlation between wound area and acuity score was determined using the Pearson correlation coefficient because both variables were normally distributed and calculated for both mathematically transformed and untransformed data.
Results
Acuity score analysis. The acuity scores for all 5,098 encounters ranged from 26 to 184 and constituted a near-normal distribution, with a mean of 95.6 (SD 30.0) (see Figure 2). The distribution failed the Kolmogorov-Smirnov test for normality because the lower tail is a little too short and a bulge occurs around 60. However, the difference from normal is relatively small as is noted by the normal curve superimposed on the histogram.
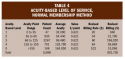
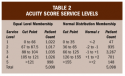 The results of the two ways of defining levels of service showed that the counts are not perfectly balanced because many acuity points have the same value (see Table 2). All identical values were placed into a single level and not split to enforce an even count. A total billing of $302,290 was calculated, which is a 13.2% reduction from $348,326 (time-based method) in billing (see Table 3). In contrast, using the normal distribution percentiles method results in the most revenues coming from Level 3. Nevertheless, the reduction in billing amount, relative to the time-based method, is similar (13.1%) (see Table 4).
The results of the two ways of defining levels of service showed that the counts are not perfectly balanced because many acuity points have the same value (see Table 2). All identical values were placed into a single level and not split to enforce an even count. A total billing of $302,290 was calculated, which is a 13.2% reduction from $348,326 (time-based method) in billing (see Table 3). In contrast, using the normal distribution percentiles method results in the most revenues coming from Level 3. Nevertheless, the reduction in billing amount, relative to the time-based method, is similar (13.1%) (see Table 4).

 Analysis by time and correlation with acuity score. The frequency with which various levels of service were billed for each initial encounter categorized by CPT codes showed that the billed level of service increased exponentially – the majority of initial consultations were billed at the highest facility level of service (see Figure 3).When follow-up visits were similarly analyzed, the most frequently billed level of service was Level 3 (CPT code 99213), with progressively fewer follow-ups billed at Levels 4 and 5 (see Figure 4). Although the Pearson correlation coefficient was 0.442 and the correlation was statistically significant (P <0.01), the results were highly inconsistent (see Figure 5). Acuity scores of 80 were billed in all five time levels of service; whereas, acuity scores 100 or higher were billed in all of the top four levels. The CMS-approved time-level billing for the 5,098 patient encounters was $348,326 (see Table 5).
Analysis by time and correlation with acuity score. The frequency with which various levels of service were billed for each initial encounter categorized by CPT codes showed that the billed level of service increased exponentially – the majority of initial consultations were billed at the highest facility level of service (see Figure 3).When follow-up visits were similarly analyzed, the most frequently billed level of service was Level 3 (CPT code 99213), with progressively fewer follow-ups billed at Levels 4 and 5 (see Figure 4). Although the Pearson correlation coefficient was 0.442 and the correlation was statistically significant (P <0.01), the results were highly inconsistent (see Figure 5). Acuity scores of 80 were billed in all five time levels of service; whereas, acuity scores 100 or higher were billed in all of the top four levels. The CMS-approved time-level billing for the 5,098 patient encounters was $348,326 (see Table 5).

 Wound diagnosis, size, and correlation with acuity score. The 5,098 patient encounters in the database contained 510 initial visits and 4,588 follow-up visits and the majority of encounters were patients with venous ulcers and traumatic wounds (see Table 6).
Wound diagnosis, size, and correlation with acuity score. The 5,098 patient encounters in the database contained 510 initial visits and 4,588 follow-up visits and the majority of encounters were patients with venous ulcers and traumatic wounds (see Table 6).
Wound areas ranged from 0 to 605 cm2, with a median value of 2.3 cm2 and a mean of 13.1 cm2. The distribution of wound areas <100 cm2 (97% of the wound areas) is shown in Figure 6. If the full range of values is plotted, the histogram collapses to a single cell on the left with a trail of insignificant columns to the right.  Statistical analysis determined that wound areas were log-normal in distribution (see Figure 7). Figure 8 shows the plot of logarithm of wound area versus acuity score (Pearson correlation coefficient of 0.055). Direct correlation of the untransformed wound area data with the acuity score yielded a correlation coefficient of 0.017.
Statistical analysis determined that wound areas were log-normal in distribution (see Figure 7). Figure 8 shows the plot of logarithm of wound area versus acuity score (Pearson correlation coefficient of 0.055). Direct correlation of the untransformed wound area data with the acuity score yielded a correlation coefficient of 0.017. 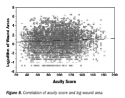
Discussion
Not surprisingly, initial consultations were viewed as the most time-consuming and billing by time tends to overestimate the billed level of service for follow-up visits. If time were a good measure of the work required for each level of service (excluding directly reimbursable procedures and products), a correlation would be expected with an acuity-based system; this was not the case. The correlation coefficient between billed level of service by time and estimated level of service by acuity was 0.442, confirming that time is not a surrogate for actual work. In an ideal system, a more normal distribution of visits would be expected, with the number of follow-up visits billed at less than Level 3 approximately equal to the number of follow-up visits billed as greater than Level 3. Time-based level of service was found to be a more reliable determinant than wound area but is still too arbitrary to constitute a consistent cost-related basis for billing.
For wound care clinics, a wound size-based system is not a viable basis for billing, regardless of how the levels of service are defined. In many cases, the final follow-up visit would have a wound area of zero (completely healed), making it unclear how these encounters would be billed in this system.
Based on the CMS proposal, this retrospective study showed that 89.4% of patient encounters would be billed at the lowest APC Code, which is tantamount to being reimbursed with a “one size fits all” billing system. If the time-based and wound-size-based analyses are compared on a financial basis, the CMS wound size-based proposal would result in a substantial decrease in billed revenue, provided the average value per point of $0.621 is maintained. Thus, while the time-based system might be fair in the acute care setting, these findings suggest that it does not translate to the chronic wound care setting.
Part of the problem is the broad range of wound areas – ie, nearly five orders of magnitude. Wound size data approximate a normal distribution once they have been transformed into a log scale. By implication, any linear scale employed to categorize wounds by area will fail in terms of fairly distributing the data for billing purposes. This is in addition to the other problems of measuring wound size and the differing amounts of work required to deal with different types of wounds. The other part of the problem is that wound area does not correlate with work performed, a fatal error for billing purposes.
How can the actual cost of providing patients with wound care services for items that are not directly reimbursable be determined? A system that measures the actual work performed, utilizing a tool such as the E&M scoring sheet, would seem both fair and straightforward to implement. The idea behind this system is to allocate the amount of work and product cost to each item that might be utilized in a patient encounter. As the point system was reviewed and refined, a normal distribution curve emerged that is more consistent with the actual value added during a patient encounter. In fact, in a recent Hospital Outpatient Regulation memorandum, the CMS reiterated statements made in its November 1, 2002 OPPS Final Rule: “… the distribution of codes should result in a normal curve.”15
All that would be needed to implement such a system is an accepted list of all the non-directly reimbursable procedures/products and an acuity score for each item. Although Table 1 provides such a schema, this system can be further improved.
The primary disadvantages of such a system are that it 1) requires detailed chart documentation and 2) is time-consuming to calculate by hand. Any items “checked” on the scoring sheet as having been carried out must correlate with specific documentation in the patient record. Obviously, in this scenario, clinics utilizing a wound care-specific EMR, which incorporates the scoring sheet into the documentation package and calculates the level of service automatically, have an operational advantage. An additional advantage of such an EMR is that it is data-based, which allows for further refinement based on logical analysis rather than arbitrary assignment of values. The E&M scoring sheet can be easily modified to delete procedures a clinic never uses or add others not currently listed, giving flexibility to the scoring system. Thus, the authors intend this tool as a starting point for the development of a comprehensive system that can undergo further validation using patient data.
In the system evaluated, the ranges of acuity scores for the five levels of service were determined based on each level being assigned 20% (on average) of patient encounters. This is for demonstration purposes; other schemes utilizing the normal curve can be developed. One such scheme was presented in Table 4. Also, although there are five levels of service, they track to only three payment amounts according to rules determined by the CMS. For this reason, the “normal membership” method of acuity scoring might be superior. The result is that scores ranging from 0 to 65 (levels 1 and 2) will track to the lowest payment schedule, scores ranging from 66 to 125 (level 3) to the second payment schedule, and scores from 126 and above (levels 4 and 5) to the highest payment schedule. The authors followed Medicare’s instructions that the ideal billing system would result in a “normal distribution” of clinic charges over a large dataset. Therefore, it was necessary not only to define an acceptable tool to measure acuity, but also to define the appropriate “break points” to relate acuity score to level of service. Regardless of whether “equal membership” or “normal distribution” breakpoints were utilized, the breakpoints are integral to the scoring system to ensure fairness in billing.
Conclusion
Results of this study suggest that time-based billing methods will likely overestimate the work involved in outpatient wound care; whereas, size-based methods will likely underestimate the actual work involved. Wound area has been shown to be unrelated to the value-added activities and should not be pursued further. Acuity-based systems seem to offer the most realistic assessment of work actually performed in association with wound management. Moreover, acuity-based systems can be adjusted in a variety of ways to provide suitable levels of service for billing purposes.
Acknowledgments
The authors thank Tomball Regional Hospital for its support in the development and testing of acuity scoring in their wound centers, as well as their support of this project. The authors are also grateful to Dr. Marissa Carter, Strategic Solutions, Inc., Little Rock, Ark, for input in the preparation of this manuscript.
1. Medicare: Hospital Outpatient Services; Prospective Payment System. Health Care Financing Administration Rules. Federal Register. 2000;65:18450-18451.
2. Goldberg M. Alliance of Wound Care Stakeholders meets with CMS. WOCN Soc News. 2005;1:1.
3. Pompeo MQ. The role of “wound burden” in determining the costs associated with wound care. Ostomy Wound Manage. 2001;47(3):65-71.
4. Garrido T, Jamieson L, Zhou Y, et al. Effect of electronic health records in ambulatory care: retrospective, serial, cross sectional study. Br Med J. 2005;330:581-584.
5. Stausberg J, Koch D, Ingenerf J, Betzler M. Comparing paper-based with electronic patient records: lessons learned during a study on diagnosis and procedure codes. J Am Med Inform Assoc. 2003;10(5):470-477.
6. Ash JS, Stavri PZ, Kuperman GJ. A consensus statement on considerations for a successful CPOE implementation. J Am Med Inform Assoc. 2003;10(3):229-234.
7. Payne TH, Hoey PJ, Nichol P, Lovis C. Preparation and use of preconstructed orders, order sets, and order menus in a computerized provider order entry system. J Am Med Inform Assoc. 2003;10(4):322-329.
8. Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. Br Med J. 2005;330(3):765-768.
9. Sim I, Gorman P, Greenes RA, et al. Clinical decision support systems for the practice of evidence-based medicine. J Am Med Inform Assoc. 2001;8(6):527-534.
10. Kennedy T, Affleck-Graves J. The impact of activity-based costing on firm performance. J Manage Account Res. 2001;13:19-45.
11. Ohura T, Sanada H, Mino Y. Clinical study using activity-based costing to assess cost-effectiveness of a wound management system utilizing modern dressings in comparison with traditional wound care. Nippon Ronen Igakkai Zasshi. 2004;41(1):82-91.
12. Bond AE, Thomas FO, Menlove RL, et al. Scoring acuity hours and costs of nursing for trauma care. Am J Crit Care. 1993;2(6):436-443.
13. Sheskin DJ. Handbook of Parametric and Nonparametric Statistical Procedures, 2nd ed. New York, NY: Chapman & Hall/CRC;2000:871.
14. Fette AM. A clinimetric analysis of wound measurement tools. Worldwide Wounds web site. Available at: http://www.worldwidewounds.com/2006/january/Fette/Clinimetric-Analysis-Wound-Measurement-Tools.html. Accessed March 14, 2006.
15. Medicare Program: Proposed Changes to the Hospital Outpatient PPS (OPPS) and CY 2007 Rates; Proposed CY 2007 Update to the ASC Covered Procedures List; and Proposed Changes to the ASC Payment System and CY 2008 Payment Rates. http://www.cms.hhs.gov/HospitalOutpatientPPS/Downloads/CMS1506P.pdf. Accessed September 4, 2006.














