Utilization of Bovine Acellular Dermal Matrix for Abdominal Wall Reconstruction: A Retrospective Case Series
Abstract:
Abdominal wall reconstruction using nonabsorbable synthetic material can be challenging due to the risk for bacterial colonization and subsequent complications. Bioprosthetic materials are a safe alternative that can facilitate soft tissue reconstruction, including abdominal wall repair.
To assess the short-term outcomes of using a bovine acellular dermal matrix in contaminated postsurgical wounds, charts of all patients who were managed using the bovine acellular dermal matrix between November 2006 and July 2007 were reviewed. Six related procedures were performed in five patients: two men and three women, median age 61 years (range 50 to 66 years), median body mass index 35 kg/m2 (range 28 to 51kg/m2). Patients underwent parastomal hernia repair and anterior abdominal wall reconstruction (one patient), reinforcement of colostomy site (one patient), and repair of large anterior abdominal wall defects following bowel resection (three patients). Clinical follow-up was complete on all patients until December 2008. Three of the five patients did not develop any wound-related complications during a median follow-up of 10 months (range 9 to 17 months). The two patients who developed complications (2 months and 10 days postoperatively, respectively) had a body mass index of 42 and 51, respectively, and multiple comorbidities. The authors’ initial experience with bovine acellular dermal matrix for various soft tissue reconstruction suggests the product is safe when used in uninfected wounds. Further experience is required to determine the effectiveness, complication profile, and feasibility of using this bioprosthesis in clinical practice and to evaluate its use in infected wounds.
Please address correspondence to: Imran Hassan, MD, Department of Surgery, SIU School of Medicine, 701 North Rutledge, PO Box 19638, Springfield, IL 62794; email: ihassan@siumed.edu.
Abdominal wall reconstruction in a contaminated or infected field1 continues to pose a significant challenge to surgeons (see Table 1). The use of nonabsorbable synthetic material is usually contraindicated in these situations due to the risk for bacterial colonization and subsequent complications including infection, skin erosion, seroma formation, bowel obstruction, and fistula formation.2 With recent advances in tissue engineering and biologic materials, a number of bioprostheses have become available for soft tissue reconstruction, including the repair of complex abdominal wall defects in the presence of contamination or infection.2-5 Bioprosthetics appear to be an excellent alternative in these circumstances because of their ability to become vascularized, remodeled into autologous tissue, and resist infection.
 The majority of the literature (case series)2,5-9 regarding bioprosthetic materials pertains to the use of human acellular dermal matrix (H-ADM, Alloderm [Lifecell, Branchburg, NJ]); reports suggest it is safe and effective. Recently, a new bioprosthetic material, SurgiMend (TEI Biosciences, Boston, MA), a bovine acellular dermal matrix, was approved by the US Food and Drug Administration (FDA) for various indications including soft tissue reconstruction. The acellular dermal matrix is manufactured from fetal bovine tissue. It is processed to remove both the epidermis and cellular components while maintaining an intact basement membrane complex and collagen bundles.
The majority of the literature (case series)2,5-9 regarding bioprosthetic materials pertains to the use of human acellular dermal matrix (H-ADM, Alloderm [Lifecell, Branchburg, NJ]); reports suggest it is safe and effective. Recently, a new bioprosthetic material, SurgiMend (TEI Biosciences, Boston, MA), a bovine acellular dermal matrix, was approved by the US Food and Drug Administration (FDA) for various indications including soft tissue reconstruction. The acellular dermal matrix is manufactured from fetal bovine tissue. It is processed to remove both the epidermis and cellular components while maintaining an intact basement membrane complex and collagen bundles.
The purpose of this retrospective case series is to describe the authors’ experience with the product when used for various indications in contaminated fields. 
Patients and Methods
A chart review of hospital records during hospitalization and physician notes from subsequent clinic visits was performed to obtain data variables including patient demographics, operative procedures, and postoperative outcomes on all patients undergoing wound repair that involved the bovine acellular dermal matrix. Between November 2006 and July 2007, the bovine acellular dermal matrix was used for six procedures in five patients. Clinical follow-up was complete on all patients through December 2008.
Institutional Review Board (IRB) approval was waived because this was a retrospective case series.
Results
The five patients in whom the bovine acellular dermal matrix was utilized included two men and three women, median age 61 years (range 50 to 66 years), median body mass index (BMI) of 35 kg/m2 (range 28 kg/m2 to 51 kg/m2). Surgical procedures included parastomal hernia repair and anterior abdominal wall reconstruction (one patient), reinforcement of colostomy site (one patient), and repair of large anterior abdominal wall defects following bowel resection (three patients). The median operative time was 503 minutes (range 190 to 689 minutes); median surface area of mesh used was 820 cm2 (range 100 cm2 to 1,500 cm2). After a median follow-up of 10 months (range 9 to 17 months), three wound-related complications were seen in two patients, both morbidly obese women with BMIs of 42 kg/m2 and 51 kg/m2, respectively. As of final follow up in December 2008, the remaining three patients (two men, one woman) with BMIs of 35, 30, 28 respectively, have not had any wound-related complications.
Case Reports
Case 1. Fifty-four year old Mr. Q had a history of Crohn’s disease and an enterocutaneous fistula for which he underwent repair and a complete proctectomy (removal of the rectum). Following the fistula repair with small bowel resection and primary anastomsosis, a 10 cm x 15 cm fascial defect remained in the anterior abdominal wall that could not be closed primarily. This defect was repaired using a 10 cm x 15 cm piece of the acellular bovine dermal matrix circumferentially sewn to the fascial edges using interrupted No. 1 polypropylene sutures.
In order to gain adequate overlap of mesh and fascia, the skin and subcutaneous tissue were separated from the underlying fascia and closed over drains. The drains were removed when the output was less than 20 cc per 24 hours. No complications developed and Mr. Q was discharged on postoperative day 10.
Case 2. Mr. R, 56 years old, with locally advanced colon cancer that was adherent to the anterior abdominal wall, underwent an en bloc resection of the colonic primary and the anterior abdominal wall that resulted in a 5 cm x 10 cm anterior abdominal wall defect that could not be primarily closed without tension. The defect was repaired by sewing a 5 cm x 10 cm piece of bovine acellular dermal matrix circumferentially to the fascial edges using No. 1 polypropylene sutures. The patient was discharged from the hospital after an unremarkable hospital course on postoperative day 8.
 Case 3. Ms. S was a 64-year-old morbidly obese woman (BMI 46 kg/m2) with a history of diabetes mellitus, coronary heart disease, and hypertension. She underwent a radical cystecotomy (removal of the urinary bladder) with ileal conduit reconstruction for a transitional cell bladder carcinoma. Two months postoperatively, she developed a parastomal hernia that continued to increase in size over the subsequent 18 months. She was unable to maintain an appliance and became homebound. The 5-cm parastomal hernia was closed primarily through a midline incision and reinforced with a 10 cm x 20 cm sheet of bovine acellular dermal matrix in an on-lay fashion. The midline incision
Case 3. Ms. S was a 64-year-old morbidly obese woman (BMI 46 kg/m2) with a history of diabetes mellitus, coronary heart disease, and hypertension. She underwent a radical cystecotomy (removal of the urinary bladder) with ileal conduit reconstruction for a transitional cell bladder carcinoma. Two months postoperatively, she developed a parastomal hernia that continued to increase in size over the subsequent 18 months. She was unable to maintain an appliance and became homebound. The 5-cm parastomal hernia was closed primarily through a midline incision and reinforced with a 10 cm x 20 cm sheet of bovine acellular dermal matrix in an on-lay fashion. The midline incision  was primarily closed and reinforced using a 10 cm x 10 cm sheet of bovine acellular dermal matrix in the same manner. Approximately 2 months after surgery, Ms. S developed subcutaneous fluid collection, requiring opening of the lower part of her midline wound. She underwent wound debridement and negative pressure dressing placement (V.A.C. Therapy®, KCI®, San Antonio, TX) at 125 mm Hg continuous negative pressure for 3 weeks. This was associated with a chronic midline wound that eventually healed by secondary intention. She also developed a recurrence of her parastomal hernia 12 months postoperatively.
was primarily closed and reinforced using a 10 cm x 10 cm sheet of bovine acellular dermal matrix in the same manner. Approximately 2 months after surgery, Ms. S developed subcutaneous fluid collection, requiring opening of the lower part of her midline wound. She underwent wound debridement and negative pressure dressing placement (V.A.C. Therapy®, KCI®, San Antonio, TX) at 125 mm Hg continuous negative pressure for 3 weeks. This was associated with a chronic midline wound that eventually healed by secondary intention. She also developed a recurrence of her parastomal hernia 12 months postoperatively.
Case 4. Mr. T was a 56-year-old paraplegic who underwent a cystectomy (removal of urinary bladder) with an ileal conduit for a neurogenic bladder and an end colostomy for fecal incontinence. His colostomy site was reinforced with a 5 cm x 10 cm piece of bovine acellular dermal matrix secured to the undersurface of the anterior abdominal wall after cutting an aperture in the middle in order for the bowel to pass through. His postoperative period was unremarkable and he was discharged on postoperative day 8.
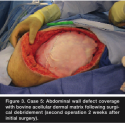 Case 5. Sixty-five-year-old Ms. E was morbidly obese with locally advanced low rectal cancer. She had previously undergone a ventral hernia repair with synthetic mesh that had recurred. She underwent an abdominoperineal resection (removal of the rectum and anus) following preoperative chemoradiotherapy. Intra-operatively, the fascial edges could not be approximated and the abdominal wall was reconstructed using a 50 cm x 60 cm piece of bovine acellular dermal matrix sewn to the fascial edges with a running No. 2 polypropylene stitch (see Figure 1), over which the subcutaneous tissue was closed. On postoperative day 10, Ms. E developed serous drainage from the wound, requiring the wound to be opened and serially debrided in the operating room over the course of a couple of weeks (see Figure 2). The resultant abdominal wall defect then was covered with another piece of bovine acellular dermal matrix (see Figure 3) and negative pressure wound therapy at 125 mm Hg, continuous negative pressure, was applied. When the negative pressure dressing was removed 48 hours later, the mesh appeared degraded and desiccated (see Figure 4). The wound was subsequently managed with wet-to-dry dressing and closed secondarily over drains.
Case 5. Sixty-five-year-old Ms. E was morbidly obese with locally advanced low rectal cancer. She had previously undergone a ventral hernia repair with synthetic mesh that had recurred. She underwent an abdominoperineal resection (removal of the rectum and anus) following preoperative chemoradiotherapy. Intra-operatively, the fascial edges could not be approximated and the abdominal wall was reconstructed using a 50 cm x 60 cm piece of bovine acellular dermal matrix sewn to the fascial edges with a running No. 2 polypropylene stitch (see Figure 1), over which the subcutaneous tissue was closed. On postoperative day 10, Ms. E developed serous drainage from the wound, requiring the wound to be opened and serially debrided in the operating room over the course of a couple of weeks (see Figure 2). The resultant abdominal wall defect then was covered with another piece of bovine acellular dermal matrix (see Figure 3) and negative pressure wound therapy at 125 mm Hg, continuous negative pressure, was applied. When the negative pressure dressing was removed 48 hours later, the mesh appeared degraded and desiccated (see Figure 4). The wound was subsequently managed with wet-to-dry dressing and closed secondarily over drains.
Discussion
Prosthetic materials often are used to reconstruct or reinforce the anterior abdominal wall in contaminated fields. Nonabsorbable synthetic materials such as polypropylene mesh may  be contraindicated in these settings due to the risk of infection. Biologic materials such as acellular dermal matrixes are alternatives in these situations because of their ability to become vascularized, remodeled into autologous tissue, and resist infection. The authors’ initial experience suggests that using a bovine acellular dermal matrix for abdominal wall reconstruction for various indications during colorectal surgery is safe and feasible in the setting of contaminated fields. However, wound-related complications can occur in high-risk patients and infections can compromise its efficacy.
be contraindicated in these settings due to the risk of infection. Biologic materials such as acellular dermal matrixes are alternatives in these situations because of their ability to become vascularized, remodeled into autologous tissue, and resist infection. The authors’ initial experience suggests that using a bovine acellular dermal matrix for abdominal wall reconstruction for various indications during colorectal surgery is safe and feasible in the setting of contaminated fields. However, wound-related complications can occur in high-risk patients and infections can compromise its efficacy.
The incidence of complications after abdominal wall reconstruction using bioprosthetics including human acellular dermal matrix (H-ADM) has been reported to be 20% to 60% in several retrospective studies.2,4,5 Among these, minor wound complications can be managed conservatively; major complications require surgical debridement or removal of the mesh and may involve hernia recurrence. The case series presented describes three wound-related complications in two of five patients, both of whom were morbidly obese women with multiple comorbidities including diabetes and malignancy.
Complications and/or hernias following repair of complex abdominal wall defects with bioprosthetics can be attributed to factors related to the patient, the surgical technique, and/or the product used. Patient factors reported to increase the risk of complications include medical comorbidities, obesity, and wound status. In a retrospective case study of abdominal wall defects managed with H-ADM, Bellows et al2 reported 15 perioperative complications (six graft dehiscences, one evisceration, two postoperative intra-abdominal bleeds, five bacterial graft infections, and one death) in 11 of 20 patients who underwent repair. In their review, patients with the American Society of Anesthesiologists (ASA) Class 4 (patient with severe systemic disease that is a constant threat to life), heart disease, and/or Class 4 wounds were more likely to have peri-operative complications. In a median follow-up period of 9.4 months (range 2 to 16 months), six hernia recurrences were reported. Although bioprosthesis can be used in the presence of gross contamination or infection, the mesh is at risk of being degraded by proteolytic enzymes associated with infections, decreasing its tensile strength2 and subsequently increasing the risk of hernia recurrence and other complications. Based on their experience with H-ADM, Schuster et al5 suggested that having an open wound with exposed H-ADM in the postoperative period following repair of contaminated fascial defects was associated with a high probability of hernia recurrence. The authors of the current study believe this may have been the reason why the bovine acellular dermal matrix became degraded and desiccated within 48 hours of placement in an infected field in Ms. S (case 3).
From a technical standpoint, the bioprosthesis can be positioned either above the fascia as an overlay, beneath the fascia as an underlay, or sutured directly to the fascial edges to act as a bridge. Espinosa-de-los-Monteros et al8 performed a retrospective analysis of 39 patients in which H-ADM was used as an adjunct to abdominal wall reconstruction. They reported H-ADM improved results by achieving tension-free repair. Jin et al3 also demonstrated that the technique employed when using H-ADM for abdominal wall reconstruction had a notable impact on hernia recurrence rates. They suggested that H-ADM should be used only as reinforcement after primary fascial re-approximation due to the significantly higher hernia recurrence rate when used as a fascial bridge.3 Unfortunately, this is not always technically feasible, particularly when soft tissue loss or loss of abdominal domain occurs and the bioprosthetic has to be used to bridge the defect between the fascial edges instead of reinforcing a primary closure.
Conclusion
Results of a five-patient case series in which bovine acellular dermal matrix was used suggest it is a feasible option for abdominal wall reconstruction in clean contaminated fields. However, the ability to maintain its integrity in an infected field is not known and warrants additional study. Further experience is required to determine its efficacy, complication profile, and feasibility in clinical practice. Due to the complex nature of indications and heterogeneous patient characteristics in which these bioprostheses are used, a comparative analysis between different materials to determine the superiority of one over the other is unlikely. Therefore, determining whether the product is an acceptable alternative to currently available bioprosthetics is likely to be based on reported experiences and complication rates as well as its availability and cost.
Drs. Wietfeldt, Hassan, and Rakinic are resident, Assistant Professor, and Associate Professor, respectively, Section of Colon and Rectal Surgery, Department of Surgery, Southern Illinois University, Springfield, IL.
1. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250–278; quiz 279–280.
2. Bellows CF, Albo D, Berger DH, Awad SS. Abdominal wall repair using human acellular dermis. Am J Surg. 2007;194:192–198.
3. Jin J, Rosen MJ, Blatnik J, et al. Use of acellular dermal matrix for complicated ventral hernia repair: does technique affect outcomes? J Am Coll Surg. 2007;205:654–660.
4. Patton JH Jr, Berry S, Kralovich KA. Use of human acellular dermal matrix in complex and contaminated abdominal wall reconstructions. Am J Surg. 2007;193:360–363; discussion 363.
5. Schuster R, Singh J, Safadi BY, Wren SM. The use of acellular dermal matrix for contaminated abdominal wall defects: wound status predicts success. Am J Surg. 2006;192:594–597.
6. Buinewicz B, Rosen B. Acellular cadaveric dermis (AlloDerm): a new alternative for abdominal hernia repair. Ann Plast Surg. 2004;52:188–194.
7. Diaz JJ Jr, Guy J, Berkes MB, Guillamondegui O, Miller RS. Acellular dermal allograft for ventral hernia repair in the compromised surgical field. Am Surg. 2006;72:1181–1187; discussion, 1187–1188.
8. Espinosa-de-los-Monteros A, de la Torre JI, Marrero I, Andrades P, Davis MR, Vasconez LO. Utilization of human cadaveric acellular dermis for abdominal hernia reconstruction. Ann Plast Surg. 2007;58:264–267.
9. Maurice SM, Skeete DA. Use of human acellular dermal matrix for abdominal wall reconstructions. Am J Surg. 2009;197(1):35–42.













