Using Negative Pressure Wound Therapy Following Surgery for Complex Pilonidal Disease: A Case Series
Pilonidal disease is a common anorectal problem with an incidence of 16 cases per 100,000 people and an incidence of 1.1% in young adult men.1,2 The majority of cases present as acute disease and are adequately managed with incision and drainage (I&D) of abscesses and laying open or excising associated sinus tracts. Infrequently, patients develop complex pilonidal disease, which is characterized by chronic or recurrent abscesses and extensive, branching sinus tracts. This manifestation of the disease demands a more aggressive surgical approach and definitive treatment requires wide excision of all involved tissue. The resulting large wound may be difficult to heal, often necessitating prolonged hospitalization and frequent clinic visits. For patients who are typically young and otherwise healthy, treatment of complex pilonidal disease causes considerable social and economic disability.1  The large wounds created by excising complex pilonidal disease may be managed open with healing by secondary intention or closed with a reconstructive procedure. Open management has the advantage of brief hospitalization but substantial morbidity results from prolonged healing. In a randomized trial, Sondenaa et al3 report 12 weeks to wound closure in the 60 (out of 120 patients) treated using open excision. In a randomized trial involving 96 patients, al-Hassan et al4 report 13 weeks to closure, along with frequent, uncomfortable dressing changes. Closing the wound with a reconstructive flap has been found to reduce healing time but requires longer hospitalization.5-7 Primary dehiscence and infection following closure are also significant causes of morbidity; primary dehiscence occurs in 9% of the cases reported and infection rates range from 3.8% to 13%.5-7 Based on the literature, the multitude of described surgical approaches to complex pilonidal disease suggests their suboptimal results.
The large wounds created by excising complex pilonidal disease may be managed open with healing by secondary intention or closed with a reconstructive procedure. Open management has the advantage of brief hospitalization but substantial morbidity results from prolonged healing. In a randomized trial, Sondenaa et al3 report 12 weeks to wound closure in the 60 (out of 120 patients) treated using open excision. In a randomized trial involving 96 patients, al-Hassan et al4 report 13 weeks to closure, along with frequent, uncomfortable dressing changes. Closing the wound with a reconstructive flap has been found to reduce healing time but requires longer hospitalization.5-7 Primary dehiscence and infection following closure are also significant causes of morbidity; primary dehiscence occurs in 9% of the cases reported and infection rates range from 3.8% to 13%.5-7 Based on the literature, the multitude of described surgical approaches to complex pilonidal disease suggests their suboptimal results.
Favorable outcomes using negative pressure wound therapy (NPWT) following wide excision of complex pilonidal disease recently were noted in three case reports.8-10 Negative pressure wound therapy for large open or nonhealing wounds seems to benefit both open and closed approaches to wound management. It can be performed as an outpatient procedure (unlike extensive reconstructive procedures) and was shown to significantly reduce wound depth in six patients with diabetic foot wounds and 24 patients with chronic nonhealing wounds (P <0.005 and P < 0.001, respectively) compared to moist saline dressing changes.11,12 A case series of five patients who underwent wide excision of their complex pilonidal disease followed by primary NPWT is described to add to existing information about the feasibility and effectiveness of this wound management technology in the treatment of complex pilonidal disease.
Literature Review
Standard surgical approaches to pilonidal disease are well-described and range from simple incision and drainage to wide excision with reconstructive flap closure.13 Allen-Mersh14 reviewed the outcomes of many of these operations, reporting failure rates as high as 43% for laying open the track and 36% for wide excision. The author concludes that no method satisfies all requirements for the ideal treatment – namely, quick healing, no hospital admission, minimal patient inconvenience, and no recurrence. The author concluded that treatment involving open granulation seems limited because it necessitates weeks of regular dressing changes. Alternatives to open granulation have been described. Using gauze dressings, Sondenaa et al3 report a healing time of 12.2 weeks versus 3.2 weeks for primary closure and in the study by al-Hassan et al4 the same comparison yielded results of 13 weeks versus 10.3 days.
Primary closure of pilonidal wounds has been shown to decrease healing time compared to open management and although imperfect has been determined to be worth the risk. Most markers of morbidity (primary treatment failure, recurrence, infection) were somewhat greater with primary closure than secondary intention in the studies cited.5-7 However, primary closure of large, complex pilonidal wounds is not a viable option, given a wound dehiscence rate of up to 37%.14
Marsupialization (partial closure) is commonly used for the treatment of simple pilonidal cysts. It reduces the size of the wound by suturing the skin edges toward the base of the wound. This technique has been associated with a decrease in healing time compared to leaving the wound completely open.15,16 While it is the preferred method over standard open management, it still requires multiple dressing changes each day. Furthermore, it has not been used for the treatment of complex pilonidal disease.
Numerous reconstructive procedures to close complex pilonidal wounds have been described.17-23 These procedures not only cover the wound but, in theory, also flatten the natal cleft and reduce hair accumulation, mechanical irritation, and risk of recurrence. Karydakis17,18 pioneered the use of flap procedures for pilonidal disease. He used a subcutaneous advancement flap created by undermining one side of the wound and closing it at the midline. It has been shown to be a successful operation for limited pilonidal disease but is not feasible for complex disease resulting in large wounds, tension-free closure. Numerous, more extensive reconstructive procedures have been described for complex pilonidal disease and are potential options for this difficult problem. Each requires inpatient hospitalization and may be complicated by flap necrosis, wound dehiscence, and infection. For example, V-to-Y advancement flaps have a healing time of 15.3 days but require a mean hospitalization of 7.3 days.20 Alternatively, Z-plasty (a common procedure described elsewhere) is a less extensive procedure but it has been associated with a 20% incidence of tip necrosis and 67% overall patient satisfaction.24,25
For patients who fail repeated interventions, gluteus maximus myocutaneous flap reconstruction has been shown to be effective with acceptable morbidity – ie, no loss of strength or range of motion despite sacrificing the gluteus maximus and no primary wound failures or infections.22,23 However, this procedure is extensive and sacrifices a deep functional muscle.20 The multitude of procedures described to treat complex pilonidal disease suggests the suboptimal results of each method and speaks to the difficulty of managing these complex wounds.
Negative pressure wound therapy for treatment of complex pilonidal disease recently has been reported to have favorable outcomes. Duxbury et al8 first described NPWT in one patient following excision of a chronic pilonidal sinus. The NPWT device was applied for 6 weeks and the wound was completely healed by 8 weeks. McGuinness et al9 report applying the device to one patient for 3 weeks, achieving complete wound healing in 7 weeks. Lynch et al10 used NPWT for primary closure in one of three patients studied (the other two patients’ wounds were closed primarily with split-thickness skin grafts; NPWT subsequently was applied NPWT to the grafts). The device was applied for 4 weeks and complete wound healing was achieved by 8 weeks. Negative pressure exerted on wounds has been reported to increase local blood flow, upregulate cell proliferation, and decrease bacterial counts, facilitating granulation tissue formation.26,27 These benefits of NPWT may be applicable to pilonidal disease.
Methods
Three men and two women with complex pilonidal disease underwent wide excision of all involved tissue and immediate postsurgical application of a portable NPWT device (V.A.C. Freedom®, KCI, San Antonio, Tex). The five patients were selected by the author (surgeon) to undergo this procedure because all of them had extensive, complex, partially open, chronically infected pilonidal sinuses. This procedure has been described previously in the literature with acceptable healing rates and was discussed in detail with the patients before informed consent was obtained. No IRB approval was required.
All procedures were performed under general anesthesia on an outpatient basis by one surgeon. Patients were placed in a prone jack-knife position and all involved tissue was excised using electrocautery. After ensuring hemostasis, an NPWT device was applied using an intermittent mode and 125 mm Hg negative pressure (standard settings at the author’s institution) to minimize variation in the treatment regimen in this small series. All patients were discharged on the day of the operation and the device dressings were changed every 48 hours at home by family members. The patients were re-evaluated in the clinic at 2- to 3-week intervals. Negative pressure wound therapy was continued until granulation tissue approached the level of the skin; NPWT generally is discontinued when the foam dressing can no longer fit within the wound because the wound is too shallow. Moist saline dressing changes then were initiated and continued until complete wound healing occurred. Follow-up was conducted both in the clinic and by telephone.
Individual Case Results (see Table 1)
Case 1. Ms. L, an otherwise healthy 21-year-old woman with symptomatic pilonidal disease of 2 years’ duration who had undergone two prior marsupialization procedures, presented with a fluctuant abscess and branching sinus tracts measuring 10 cm x 4 cm x 3 cm. Following excision, her wound defect measured 13 cm x 5 cm x 7 cm. She required 9 weeks of NPWT and a total of 11 weeks for complete epithelialization. The wound was healed at 14-month follow-up.
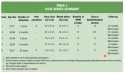 Case 2. Mr. M, an otherwise healthy 16-year-old, presented to the emergency department with bloody drainage from his perianal area. He had experienced intermittent drainage for up to 6 months. A branching pilonidal sinus tract containing a large amount of hair extended 12 cm x 3 cm x 3 cm. Following excision, the wound defect measured 12 cm x 3 cm x 3 cm. Mr. M received NPWT for 4 weeks; subsequent moist saline dressing changes failed to epithelialize the wound. After 8 weeks, Mr. M was returned to the operating room for debridement to remove hypertrophic granulation tissue that had formed at the wound edge. An NPWT device was reapplied and continued for 2 weeks in the same manner as before. At follow-up 12 weeks later, the wound had completely epithelialized. Mr. M later experienced a superficial wound separation, which healed with dry dressing applications. At his 11-month follow-up visit, the wound remained healed.
Case 2. Mr. M, an otherwise healthy 16-year-old, presented to the emergency department with bloody drainage from his perianal area. He had experienced intermittent drainage for up to 6 months. A branching pilonidal sinus tract containing a large amount of hair extended 12 cm x 3 cm x 3 cm. Following excision, the wound defect measured 12 cm x 3 cm x 3 cm. Mr. M received NPWT for 4 weeks; subsequent moist saline dressing changes failed to epithelialize the wound. After 8 weeks, Mr. M was returned to the operating room for debridement to remove hypertrophic granulation tissue that had formed at the wound edge. An NPWT device was reapplied and continued for 2 weeks in the same manner as before. At follow-up 12 weeks later, the wound had completely epithelialized. Mr. M later experienced a superficial wound separation, which healed with dry dressing applications. At his 11-month follow-up visit, the wound remained healed.
Case 3. Otherwise healthy 21-one-year-old Mr. N presented with a large, hair-filled abscess. He reported having recurrent purulent drainage from the natal cleft for 6 years – a problem that had never been treated surgically. On physical examination, the abscess measured 9 cm x 4 cm x 3 cm; following excision, the wound defect measured 9 cm x 4 cm x 4 cm. Mr. N required 6 weeks of NPWT and an additional 3 weeks of moist saline dressing changes for complete epithelialization. The wound remained well healed for 10 months but then separated to a depth of 1.5 cm. This separation was managed conservatively and healed with dry gauze dressings within 2 weeks.
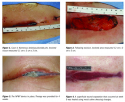
Case 4. Otherwise healthy 16-year-old Mr. O presented with numerous draining pilonidal pits that were noticed at a high school physical examination. The pits could be probed, revealing a branching network of sinus tracts. The involved tissue measured 11 cm x 3 cm x 3 cm (see Figure 1). Following excision, the wound defect was 12 cm x 3 cm x 5 cm (see Figure 2). Mr. O required 4 weeks of NPWT (see Figure 3); at 9 weeks, the wound was completely epithelialized. At 12 weeks, Mr. O experienced a superficial wound separation (see Figure 4) that healed with moist saline dressing changes. At Mr. O’s 9-month follow-up, the wound remained healed.
 Case 5. Ms. P was an otherwise healthy 63-year-old woman with chronic, recurring pilonidal disease for 30 years. She had undergone five prior operations, most recently wide excision with Z-plasty. She presented with an 8 cm x 4 cm x 5 cm area of branching sinus tracts. Following excision, her wound defect measured 11 cm x 4 cm x 7 cm. She tolerated 5 weeks of NPWT but had significant skin irritation from the adherent dressing. When she was re-evaluated in the clinic, areas of skin adjacent to the wound had broken down. She chose to discontinue NPWT before achieving optimal granulation and moist saline dressing changes were initiated. She achieved complete epithelialization at 9 weeks. At her 6-month follow-up clinic visit, the wound remained well healed.
Case 5. Ms. P was an otherwise healthy 63-year-old woman with chronic, recurring pilonidal disease for 30 years. She had undergone five prior operations, most recently wide excision with Z-plasty. She presented with an 8 cm x 4 cm x 5 cm area of branching sinus tracts. Following excision, her wound defect measured 11 cm x 4 cm x 7 cm. She tolerated 5 weeks of NPWT but had significant skin irritation from the adherent dressing. When she was re-evaluated in the clinic, areas of skin adjacent to the wound had broken down. She chose to discontinue NPWT before achieving optimal granulation and moist saline dressing changes were initiated. She achieved complete epithelialization at 9 weeks. At her 6-month follow-up clinic visit, the wound remained well healed.
Summary of Results
The median age of the five patients was 21 years (range 16 to 63 years). Duration of symptoms before current treatment ranged from 6 months to 30 years; two patients had undergone prior operations (I&D and Z-plasty), of whom one had five prior operations over 30 years and no period of complete healing. The mean area of involved tissue on physical examination was 10 cm x 3 cm x 4 cm or 124 cm3 (range 90 cm3 to 140 cm3). Mean wound defect after excision was 11 cm x 4 cm x 5 cm, or 205 cm3 (range 90 cm3 to 410 cm3). Mean duration of NPWT was 6 weeks (range 4 to 9 weeks). Mean time to complete epithelialization was 12 weeks (range 9 to 22 weeks). Three patients experienced a superficial wound separation following epithelialization. Each was managed conservatively with moist saline or dry dressing changes. One patient’s wound failed to epithelialize and required operative debridement and reapplication of the NPWT device; the wound eventually healed. One patient did not tolerate NPWT due to significant skin irritation from the NPWT dressing material; measures taken to protect the skin failed and NPWT was discontinued after 5 weeks, at which point she was managed with moist saline dressing changes twice a day. The wound healed after 9 weeks.
Discussion
Pilonidal disease is a common anorectal problem that infrequently manifests as chronic or recurrent abscesses with extensive, branching sinus tracts. Complex pilonidal disease may stem from prolonged neglect of symptoms but also occurs despite appropriate treatment of the acute problem. Wide excision of all involved tissue is necessary for definitive treatment but the resulting large wounds may be difficult to heal and often are debilitating for patients. The optimal approach to healing these wounds would be a simple procedure with few complications requiring brief hospitalization and short healing time; current approaches fail to meet these criteria. Open management and healing by secondary intention may involve brief hospitalization but require prolonged healing with frequent dressing changes. Closing the wounds with various reconstructive procedures reduces healing time but requires longer hospitalization and risks flap necrosis, wound dehiscence, and infection.5-7
Negative pressure wound therapy recently has been used to manage complex pilonidal wounds; it appears to optimize open and closed approaches.8-10 The five patients reported in this case series had large wound defects averaging 205 cm3. Allowing large wounds to heal by secondary intention would require weeks if not months of frequent dressing changes, resulting in considerable social and economic disability for patients. In the cases presented, it appears that primary NPWT for complex pilonidal disease is feasible as an outpatient procedure. It is effective in terms of low morbidity and is generally well tolerated by the patients. An intermittent therapy mode of 125 mm Hg was used as the standard setting in order to minimize variation in the treatment regimen in this small series. Negative pressure wound therapy helped facilitate granulation of healthy tissue and avoided the accumulation of any slough (none was noted before treatment). One patient did not tolerate the NPWT dressing (exhibited skin sensitivity to the adherent dressing) which resulted in premature discontinuation of the therapy. However, when NPWT was discontinued, the patient’s wound was clean, smaller than the initial wound, and by 9 weeks closed with moist saline dressing changes. One patient needed re-operation and re-initiation of NPWT after it had been discontinued due to poor healing after starting moist saline dressing. Three of the five patients experienced minor skin separation that healed within a few weeks with standard dry dressing changes.
Although no assertion that NPWT accelerated healing in these five patients can be made without a control group, other studies present evidence that NPWT speeds healing over saline gauze dressings in other types of wounds.11,12 One study28 specifically addresses the safety of NPWT. Several studies3,4 comparing healing by granulation with saline gauze and primary closure following excision of a pilonidal cyst indicate that primary closure is preferable. However, in large wounds, as described in this series, the failure rate of primary closure is high (37%); therefore, these wounds need to be closed with reconstructive flaps, which have drawbacks (extensive procedures requiring hospitalization and carrying risk of wound dehiscence and infection) or must be left open to granulate. Negative pressure wound therapy is a new potential treatment modality; its use is reported in three separate case reports. In this case series, four out of the five wounds reported healed safely. One patient experienced skin irritation that resulted in discontinuing NPWT.
A possible disadvantage of NPWT is cost, although in studies involving other types of chronic wounds its cost-effectiveness has been demonstrated.29 Furthermore, many otherwise healthy younger patients often do not qualify for wound care at home because they are not home bound. The newer NPWT devices allow the patient to be more mobile – one of the patients in this series continued attending high school while undergoing NPWT. Long-term follow-up is needed in these five patients to assess the risk of recurrent pilonidal disease or wound breakdown following excision and primary NPWT. Future studies should evaluate optimal NPWT parameters, costs, quality of life, and patient satisfaction with this new treatment option for complex pilonidal disease.
Conclusion
Primary NPWT following wide excision of complex pilonidal disease is feasible and effective with short-term subsequent follow-up. Initial NPWT can be provided as an outpatient procedure and, in this case series, few complications occurred. Long-term follow-up is required to assess the risk of recurrent pilonidal disease or wound failure following NPWT.
1. Dwight RW, Maloy JK. Pilonidal sinus: experience with 449 cases. N Engl J Med. 1953;249(23):926-930.
2. Sondenaa K, Anderson E, Nesvik I, Soreide JA. Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis. 1995;10:39-42.
3. Sondenaa K, Nesvik I, Anderson E, Soreide JA. Recurrent pilonidal sinus after excision with closed or open treatment: final result of a randomized trial. Eur J Surg. 1996;162(3):237-240.
4. al-Hassan HK, Francis IM, Neglen P. Primary closure or secondary granulation after excision of pilonidal sinus? Acta Chir Scand. 1990;156(10):695-699.
5. Füzün M, Bakir H, Soylu M, Tansug T, Kaymak E, Harmancioglu O. Which technique for treatment of pilonidal sinus – open or closed? Dis Colon Rectum. 1994;37(11):1148-1150.
6. Sondenaa K, Anderson E, Soreide JA. Morbidity and short-term results in a randomized controlled trial of open compared to closed treatment of chronic pilonidal sinus. Eur J Surg. 1992;158(6-7):351-355.
7. Perruchoud C, Vuilleumier H, Givel JC. Pilonidal sinus: how to choose between excision and open granulation versus excision and primary closure. Swiss Surg. 2002;8(6):255-258.
8. Duxbury MS, Finlay IG, Butcher M, Lambert AW. Use of a vacuum-assisted closure device in pilonidal disease. J Wound Care. 2003;12(4):355.
9. McGuinness JG, Winter DC, O’Connell PR. Vacuum-assisted closure of a complex pilonidal sinus. Dis Colon Rectum. 2003;46(2):274-276.
10. Lynch JB, Laing AJ, Regan PJ. Vacuum-assisted closure therapy: a new treatment option for recurrent pilonidal sinus disease. Report of three cases. Dis Colon Rectum. 2004;47(6):929-932.
11. Eginton MT, Brown KR, Seabrook GR, Towne JB, Cambria RA. A prospective randomized evaluation of negative pressure wound dressing for diabetic foot wounds. Ann Vasc Surg. 2003;17(6):645-649.
12. Joseph E, Hamori CA, Bergman S, et al. A prospective randomized trial of vacuum-assisted closure versus standard therapy of chronic nonhealing wounds. WOUNDS. 2000;12(3):60-67.
13. Nivatvongs S. Common anorectal problems. In: Kelly KA, Sarr MG, Hinder RA, eds. Mayo Clinic Gastrointestinal Surgery. Philadelphia, Pa: Saunders;2004:589-626.
14. Allen-Mersh TG. Pilonidal sinus: finding the right track for treatment. Br J Surg. 1990;77(2):123-132.
15. Solla JA, Rothenberger DA. Chronic pilonidal disease. An assessment of 150 cases. Dis Colon Rectum. 1990;33(9):758-761.
16. Spivak H, Brooks VL, Nussbaum M, Friedman I. Treatment of chronic pilonidal disease. Dis Colon Rectum. 1996;39(10):1136-1139.
17. Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. 1992;62(5):385-389.
18. Kitchen PR. Pilonidal sinus: experience with the Karydakis flap. Br J Surg. 1996;83(10):1452-1455.
19. Mansoory A, Dickson D. Z-plasty for treatment of disease of the pilonidal sinus. Surg Gynecol Obstet. 1982;155(3):409-411
. 20. Schoeller T, Wechselberger G, Otto A, Papp C. Definite surgical treatment of complicated recurrent pilonidal disease with a modified fasciocutaneous V-Y advancement flap. Surgery. 1997;121(3):258-263.
21. Mentes BB, Leventoglu S, Cihan A, Tatlicioglu E, Akin M, Oguz M. Modified Limberg transposition flap for sacrococcygeal pilonidal sinus. Surg Today. 2004;34(5):419-423.
22. Perez-Gurri JA, Temple WJ, Ketcham AS. Gluteus maximus myocutaneous flap for the treatment of recalcitrant pilonidal disease. Dis Colon Rectum. 1984;27(4):262-264.
23. Rosen W, Davidson JS. Gluteus maximus musculocutaneous flap for the treatment of recalcitrant pilonidal disease. Ann Plast Surg. 1996;37(3):293-297.
24. Bose B, Candy J. Radical cure of pilonidal sinus by Z-plasty. Am J Surg. 1970;120(6):783-786.
25. Tschudi J, Ris HB. Morbidity of Z-plasty in the treatment of pilonidal sinus. Chirurg. 1988;59(7):486-490.
26. Saxena V, Hwang CW, Huang S, et al. Vacuum-assisted closure: microdeformation of wounds and cell proliferation. Plast Reconst Surg. 2004;114(5):1086-1096.
27. Morykwas MJ, Argenta LC, Shelton-Brown EI, McGwirt W. Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. 1997;38(6):553-562.
28. Pham CT, Middleton PF, Maddern GJ. The safety and efficacy of topical negative pressure in non-healing wounds: a systematic review. J Wound Care. 2006;15(6):240-250.
29. Philbeck TE Jr, Whittington KL, Millsap MH, et al. The clinical and cost effectiveness of externally applied negative wound therapy in the treatment of home healthcare Medicare patients. OstomyWound Manage. 1999;45(11):41-50.













