A Prospective Evaluation of a Pressure Ulcer Prevention and Management E-Learning Program for Adults with Spinal Cord Injury
Abstract
Pressure ulcers are a common complication of spinal cord injury (SCI). Pressure ulcer education programs for spinal cord injured individuals have been found to have a positive effect on care protocol adherence. A prospective study was conducted among hospitalized spinal cord-injured men and women to determine if viewing the Pressure Ulcer Prevention and Management Education for Adults with Spinal Cord Injury: E-Learning Program affects their knowledge scores. A 20-question multiple-choice pre-/post learning test was developed and validated by 12 rehabilitation nurses.
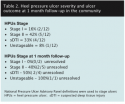
Twenty (20) patients (13 men, seven women; mean age 49 years, [SD: 18.26] with injuries to the cervical [seven], thoracic [six], and lumbar [six] regions) volunteered. Most (42%) had completed high school and time since SCI ranged from 2 weeks to 27 years. Eighteen (18) participants completed both the pre- and post test. Of those, 16 showed improvement in pressure ulcer knowledge scores. The median scores improved from 65 (range 25 to 100) pre-program to 92.5 (range 75 to 100) post-program. Descriptive statistics, Student’s t-test, and analysis of variance (ANOVA) were used to analyze the data. The results suggest that a single viewing of this e-learning program could improve pressure ulcer knowledge of hospitalized adults with SCI. Research to ascertain the effects of this and other educational programs on pressure ulcer rates is needed.
Potential Conflicts of Interest: The authors provided no relevant disclosures. The development of the web-based program was supported by Grant #528 (PI: Jane Schubart) from the Paralyzed Veterans Association Education and Training Foundation and developed at the University of Virginia School of Medicine, 2004–2006.
Pressure ulcer development continues to be a common complication, second only to respiratory illness, among spinal cord-injured persons.1,2 Approximately 85% of spinal cord-injured persons will develop a pressure ulcer during their lifetime despite available evidence-based prevention programs.3,4 To be effective, an education program must be individualized for spinal cord-injured persons2,5-7 (most are designed for inpatients in rehabilitation facilities, not for patients in acute care) and should include an assessment of the person’s learning abilities and a test of the knowledge and skills retained.6,8 Yet methods to satisfactorily appraise the information retained by the spinal cord-injured person are rare.5
A prospective study was conducted to determine if viewing the Pressure Ulcer Prevention and Management Education for Adults with Spinal Cord Injury: E-Learning Program affected spinal cord-injured patient knowledge about the identification, prevention, and early detection of pressure ulcers.

Identical tests were administered before and after viewing the program and results assessed. This is the first study of the E-Learning Program.


 Spinal Cord-Injured Population
Spinal Cord-Injured Population
A recent report by the Christopher and Dana Reeve Foundation9 shows that approximately 0.4% of the US population (~1,275,000 people) report being paralyzed due to a SCI, which is five times more people living with SCI than previously estimated. This study9 was led by the University of New Mexico’s Center for Development and Disability (CDD) from 2006 to 2008 and included experts from the US Centers for Disease Control and Prevention (CDC) and 13 universities and medical centers. The main causes of SCI were found to be work-related accidents (28%), vehicle accidents (24%), and sporting/recreational accidents (17%). The average length of time since the SCI occurred among participants was 14 years (SD: 12 years). Of persons who reported being paralyzed due to a SCI, 61% were men (39% women) — men were nearly twice as likely as women to incur a SCI; approximately 75% were Caucasian, 15.6% were Black/African American, 7.3% were Native American/Alaskan, and 13% were Hispanic. Fifty percent (50%) of admissions to hospitals specializing in the spinal cord-injured population are related to pressure ulcers.10 The primary causes of death in spinal cord-injured persons are pneumonia, pulmonary embolism, and septicemia. Considerably higher mortality rates are reported in the first year after injury as compared to subsequent years after injury.11
Pressure Ulcer Prevalence and Incidence
Pressure ulcer rates are highest among the elderly and spinal cord-injured patients10; the latter have a life-long risk for developing a pressure ulcer.12-14 Approximately 95% of all pressure ulcers reported in the US are located below the waist15,16; approximately 65% of these pressure ulcers occur on the ischial tuberosities, sacrum, coccyx, and trochanters and are attributed to wheelchair use among spinal cord-injured persons.17
Among spinal cord-injured persons, reported annual pressure ulcer prevalence rates range from 10.2% to 30%2 and annual incidence rates range from 20% to 31%.2 A review of the literature by the National Pressure Ulcer Advisory Panel18 (NPUAP) reported that 31% of pressure ulcers were associated with the spinal cord-injured population. Of the 31% reported pressure ulcers among spinal cord-injured persons, 15.2% to 31% were determined to be Stage I to Stage IV, and of these 7.4% were identified as Stage II to Stage IV.18
Pressure Ulcer Costs and Complications
Regan et al2 estimated the annual cost of treating pressure ulcers among the spinal cord-injured population to be $1.2 billion to $1.3 billion. Pressure ulcers increase the length of hospital stays and, in spinal cord-injured persons, they are one of the foremost reasons for rehospitalization.19,20 These expenditures for pressure ulcer treatment are more costly than the treatment of all other health conditions.19
Data regarding pressure ulcer complications, as well as prevalence and incidence rates, may be underestimated for numerous reasons, including; 1) hospitals, long-term care facilities, and home care may not report pressure ulcers or may report a lesser stage of the pressure ulcer to avoid monetary penalties; 2) in some facilities, spinal cord-injured persons with pressure ulcers may not be reported separately from all other persons with pressure ulcers; 3) individuals who are not experts may not designate the correct pressure ulcer stage; 4) not all persons with pressure ulcers are in a healthcare setting or followed by a home care agency, and 5) national databases are not always equipped to track pressure ulcers over a period of time — the literature indicates that prevalence and incidence data collected in some studies differ from national database data.18
Pressure ulcers cause detrimental physical and emotional alterations that affect body image, self-esteem,21-23 social relations, and loss of income and support systems.2,21 These are considered “hidden” costs for healthcare but may drastically impact outcomes for patients.
High rates of medical complications and mortality have been reported with spinal cord-injured patients with pressure ulcers.3,21 Even though this population is living longer due to medical advancements, death occurs at ages younger than the general population.24 Cardenas et al19 conducted a cross-sectional analysis of data (n = 8,668 persons with SCI) and Chen et al24 performed a multicenter cohort study design (n = 3,361 spinal cord-injured persons) — both studies found the risk of developing a pressure ulcer increases as the spinal cord-injured patient ages. Complications such as anemia, osteomyelitis, and sepsis from a pressure ulcer can be life-threatening; in addition, patients with injuries of the cervical spine (ie, the neck and upper back region from C1 to C8) tend to have respiratory complications and patients with injuries of the thoracic and sacral spine (ie, middle to lower back region from T1 to S5) are more likely to have pressure ulcer complications.19
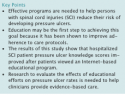
The Role of Educational Programs
Educational programs providing instruction on the risk, prevention, and early detection of pressure ulcers are important for the overall well being of spinal cord-injured persons. The patients must know what to do to reduce the risk of occurrence and be able to recognize and manage a pressure ulcer when one occurs. Adherence to the pressure ulcer prevention program is vital. According to the Spinal Cord Medicine’s Guidelines,5,25,26 spinal cord-injured persons who participate in rehabilitation and an educational program have greater protocol adherence than those who do not participate. Increased adherence with prevention programs has been associated with educational strategies that include detailed knowledge and practice techniques.27 However, few studies have been designed to test knowledge retention and occurrence/reoccurrence rates after initial pressure ulcer prevention education.2,6,7
According to the literature,6,7 pressure ulcer education is typically offered during the hospital and rehabilitation period when the newly injured person is adjusting to many life changes and may not be receptive to education about pressure ulcers. Additional factors that may influence the effectiveness of education include cognitive impairments, psychological distress, unwillingness to accept and learn about the disability, lack of available programs, and timing of delivery that may be too soon after injury.5,6
Hospital and rehabilitation length of stay have decreased over the years, further limiting opportunities for effective education.5 According to the National Spinal Cord Injury Statistical Center11 (NSCISC) database, the average length of inpatient rehabilitation stays of patients with SCI in 1974 was approximately 127.3 days. Over the next 20 years, NSCISC recorded a steady decline; by 1994, the length of inpatient rehabilitation stay was, on average, 54.6 days.28 The NSCISC data collected from 2005 to 2008 showed that the average length of stay in acute care and rehabilitation facilities decreased to 12 days and 37 days, respectively.
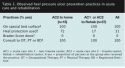
Although evidence-based guidelines for preventing pressure ulcers have been developed, a mail survey study by Krause and Broderick29 of 826 spinal cord-injured persons who were at least 5 years since injury showed that current prevention programs for this population have had limited success in reducing pressure ulcer occurrence and reoccurrence and that the risk of recurrent pressure ulcer development is related to overall activities such as healthy behavior, not just to health maintenance activities such as weight shifts and skin checks. Garber et al6 conducted a randomized, controlled study of 41 patients — 39 were spinal cord-injured and two had multiple sclerosis. The treatment group (n = 20) received four 1-hour educational sessions on the prevention and management of pressure ulcers and the control group received standard education, which was not specified. The Pressure Ulcer Knowledge Test, which was developed by Garber et al, administered after instruction, showed a significant difference (P <0.03) between the study and control groups in knowledge gained. A 2-year follow up showed that the two groups retained the knowledge; however, the treatment group scored higher than the control group on the Pressure Ulcer Knowledge Test (73.86% versus 64.00%).
The E-Learning Program
A Pressure Ulcer Prevention and Management Education for Adults with Spinal Cord Injury: E-Learning Program (E-Learning Program) was developed by Jane Schubart, PhD, and Michelle Hilgart, MEd, at the University of Virginia (Pressure Ulcer Prevention E-Learning Program: (University of Virginia Patent Foundation, Copyright Registration No. TXu1-570-776, J. Schubart and M. Hilgart).7 Development of the E-Learning Program was funded by a grant from the Paralyzed Veterans of America Education Foundation.
The content is organized into three sections, Learning, Living, and Looking. The Learning section covers pressure ulcer basics, pressure ulcer risk factors, equipment and environment, healthy skin strategies, and focus on caregivers. The Living section is an interactive case (“Martha’s story”) designed to reinforce the material. The Looking section contains a glossary of common terms and images related to the prevention and treatment of pressure ulcers. The E-Learning Program is highly interactive (self testing, risk assessment, and glossary) and includes audio narration of the text. Because the program was designed so the user could stop and start at the same point at a future time, it may be completed in one or multiple sessions, either in a linear fashion or by maneuvering throughout to view or review topics of interest.
Positive attributes of the E-Learning program are its ease of use and the narration that guides users throughout the program. Audio instructions/questions, as well videos and images, are provided for those whose reading skills may be limited. Another positive quality is that the E-Learning program is comprehensive and includes various aspects of prevention and early detection of pressure ulcers. The E-Learning program includes standard content and is intended to reduce the amount of time a skilled nurse educator needs to be available to provide instruction and answer questions. The developers can easily update content as pressure ulcer prevention and treatment guidelines change.
On the negative side, spinal cord-injured persons without access to the Internet, persons with a lack of computer experience, and persons with cervical injuries would not be able to use the E-Learning Program without assistance.
This is the first study to test the program with hospitalized SCI patients for knowledge regarding pressure ulcers. The program can be used wherever there is Internet access. (For access to the program, please contact the corresponding author.)
1. King RB, Porter SL, Vertiz KB. Preventive skin care beliefs of people with spinal cord injury. Rehabil Nurs. 2008;33(4):154–162.
2. Regan MA, Teasell R, Wolfe DL, Keast D, Mortenson WB, Aubut JL. A systematic review of therapeutic interventions for pressure ulcers after spinal cord injury. Arch Phys Med Rehabil. 2009;90:213–231.
3. Rathore FA, Waheed A. Pressure ulcers in spinal cord injury: an unusual site and etiology. Am J Phys Med Rehabil. 2009;88(3):1–4.
4. Vohra R, McCollum C. Fortnightly review: pressure sores. Br Med J. 1994;309(6958):853–857.
5. Consortium for Spinal Cord Medicine. Pressure Ulcer Prevention and Treatment Following Spinal Cord Injury: A Clinical Practice Guideline for Health-Care Professionals. Washington, DC: Paralyzed Veterans of America;2000.
6. Garber SL, Rintala DH, Holmes SA, Rodriguez GP, Friedman J. A structured educational model to improve pressure ulcer prevention knowledge in veterans with spinal cord dysfunction. J Rehabil Res Develop. 2002;39(5):575–588.
7. Schubart JR, Hilgart M, Lyder C. Pressure ulcer prevention and management in spinal cord injured adults: analysis of educational needs. Adv Skin Wound Care. 2008;21(7):322–328.
8. Maklebust J, Magnan MA. Approaches to patient and family education
9. Christopher and Dana Reeve Foundation 2010. One Degree of Separation: Paralysis and Spinal Cord Injury in the United States. Available at: www.christopherreeve.org/site/c.mtKZKgMWKwG/b.5184255/k.6D74/Prevalence_of_Paralysis.htm. Accessed March 15, 2010.
10. Thomas DR. Prevention and treatment of pressure ulcers: What works? What doesn't? Cleve Clin J Med. 2001;68(8):704–707.
11. Spinal Cord Injury Information Network. Spinal Cord Injury Facts and Figures at a Glance 2009. Birmingham, AL: National Spinal Cord Injury Statistical Center; 2009. Available at: www.nscisc.uab.edu/public_content/ facts_figures_2009.aspx. Accessed March 21, 2010.
12. Langemo D, Brown G. Skin fails too: acute, chronic, and end-stage skin failure. Adv Skin Wound Care. 2006;19(4):206–212.
13. Phillips L. Pressure ulcers – prevention and treatment guidelines. Nurs Stand. 1999;14(12):56–62.
14. Witkowski J, Parish L. The decubitus ulcer: skin failure and destructive behavior. Int J Dermatol. 2000;39(12):894–895.
15. Baldwin KM. Damage control: preventing and treating pressure ulcers. Nursing Made Incredibly Easy! 2006;4(1):12–27.