A Prospective, Descriptive Study of Characteristics Associated with Skin Failure in Critically Ill Adults
Abstract
Critically ill patients with multi-organ failure are especially susceptible to problems with skin integrity, including skin failure. An 18-month, prospective, descriptive study was conducted to identify and describe characteristics of intensive care unit (ICU) patients with skin failure and examine the relationships among patient demographics, nutritional status, laboratory parameters, the presence of other organ system failures, and use of mechanical assistive devices, support surfaces, and vasopressive and sedative medications. A total of 29 patients with acute skin failure were identified. All (100%) patients with skin failure were diagnosed with failure of at least one other organ system. Ninety percent (90%) had failure of more than one organ system other than skin, and 90% had an albumin level <3.5 mg/dL. In addition, generalized edema, ventilator use, age >50 years, weight > 150 lb, creatinine >1.5 mg/dL, mean arterial pressure <70 mm Hg, and/or the use of sedatives and/or analgesic medications were observed in >75% of patients with skin failure. Significant positive correlations were seen between several pairs of variables, including sepsis and renal failure, and the concurrent use of several types of vasopressive agents. This is the first known study of its type and results confirm that nonskin organ system failure and skin failure can be expected to be observed at the same time. Research to ascertain whether skin failure occurs at the same time, precedes, or follows the development of nonskin organ system failure is needed, as are studies to understand the relationship among the various risk factors in order to optimize preventive care.
Potential Conflicts of Interest: none disclosed
Introduction
Regardless of the quality of care received, critically ill patients are at high risk for impaired skin integrity. Pressure ulcer (PU) incidence, one type of skin integrity problem, occurs in 13% to 42% of intensive care patients despite advances in support surface technology and knowledge about PU prevention strategies.1 Possibly, intrinsic factors are associated with critically ill patients that negate clinician efforts to prevent the development of skin problems.
The skin and underlying structures are dependent on other organs and body systems to supply nutrition and oxygen, as well as to remove toxins. Critically ill patients with multi-organ failure are especially susceptible to problems with skin integrity, including skin failure. These patients frequently have alterations in tissue perfusion and, because of their failed organs, are unable to maintain homeostasis. This may lead to the death of the skin and underlying structures.
The purpose of this prospective, descriptive study was to identify and describe the characteristics of intensive care unit (ICU) patients with skin failure and examine the relationships among patient demographics, nutritional status, laboratory parameters, the presence of other organ system failures, and use of mechanical assistive devices, support surfaces, and vasopressive and sedative medications. 
Literature Review
Organ failure in patients admitted to the ICU. Admission to an ICU poses significant risks for the patient. These risks come not only from the disease or trauma that necessitate ICU admission, but also from characteristics of the patients and the treatments designed to help them. Patient risk factors of which most nurses are well aware include age, the presence of comorbidities, and a history of trauma or surgery. Treatment factors include nutritional management, effectiveness of infection control measures, and management of tissue perfusion. Each type of risk factor may carry substantial implications for the development of complications and organ system failure. Skin, the largest organ in the body, is not immune to these risks; it, too, can develop complications, become dysfunctional, and ultimately fail.
The increasing use of technology in providing life support to critically ill patients has contributed to prolonged survival in this patient population. Thus, it is not uncommon for patients to die from conditions unrelated to their initial injury or condition.2 Multi-organ failure was first described in 1973 by Tilney3 as the postoperative failure of uninvolved organs after significant blood loss and shock. Over the years, this syndrome has been referred to as multi-system organ failure, multiple organ failure, and most recently multi-organ dysfunction syndrome (MODS).4 MODS is defined as “the presence of altered organ function in an acutely ill patient such that homeostasis cannot be maintained without an intervention.”5
In contrast to organ failure due to other causes, failure of organs in MODS often is not due to direct insult to the failing organ; there is a period of time, ranging from days to weeks, from the initiating event to failure of the distant organ. The sequence of distant organ failure is typically respiratory failure followed by hepatic failure, intestinal failure, and finally renal failure. Heart and hematopoetic failure may occur later. This sequence may be influenced by pre-existing conditions.6 A systemic inflammatory response syndrome usually precedes MODS. The most common condition leading to MODS is sepsis; however, not all patients with MODS have evidence of infection. Other risk factors are severity of illness, severe trauma, major operations, age >65 years, persistent lack of oxygen availability after circulatory shock, and pre-existing end-stage liver failure.7
Several hypotheses have been posed concerning the cause of MODS, and overlap exists in some theories of causality. The endotoxin macrophage hypothesis proposes endotoxin as a primary mediator due to the formation and release of cytokines. In the gut hypothesis, bacteria or endotoxin derived from the intestine initiate the septic state. The vulnerability of the intestines to ischemia promotes bacterial translocation. This helps explain why a specific source of septicemia is not identified for many septic patients with MODS.8 The two event hypothesis assumes that an event such as hypotension readies the immune system, so a second insult such as infection at a vulnerable time will result in systemic inflammation that leads to MODS. Finally, the tissue hypoxia microvascular hypothesis states that microvascular changes result in an inadequate oxygen supply and cause tissue hypoxia that may lead to organ dysfunction and cellular death.7
Identifying patients susceptible to failure of more than one organ system is key to preventing additional organ system failure, including MODS. In a case presentation and literature review, Walsh9 noted various risk factors for the development of MODS, including advanced age, presence of chronic diseases, tissue hypoperfusion, immunosuppression, multiple blood transfusions, infections, burns, and sepsis.
Skin failure. The skin helps maintain homeostasis within the body and protects against external assaults. The skin measures approximately 3,000 square inches and “receives one third of the body’s circulating blood volume”10 via the capillaries. Because the skin covers such a large area and receives only capillary blood flow, many factors affect the skin’s and its supporting structures’ ability to remain intact, including factors that affect tissue perfusion such as hemoglobin levels, interstitial and lymphatic flow, oxygen supply and demand, and the presence of endotoxins.11
Langemo and Brown12 conducted a systematic review of terms associated with acute, chronic, and end-stage skin failure. They defined acute skin failure as “an event in which skin and underlying tissue die due to hypoperfusion concurrent with a critical illness.” They noted that when patients become critically ill, they develop risk factors for PUs as well as skin failure, such as poor tissue perfusion, decreased nitrogen balance, and immobility. Critically ill patients with multi-organ failure/dysfunction and sepsis are especially at risk for hypoperfusion due to microvascular dysfunction, increased oxygen demand, and vasoconstriction. This phenomenon has been noted by Reger et al13 in an analysis of support surface interface pressure, Lamblin et al14 in a study of 10 sedated ICU patients, and Campbell et al15 in a review article on the metabolic response to trauma and sepsis.
Compromised skin integrity may be closely associated with mortality. A nonexperimental, retrospective analysis16 of PU data involving 74 patients showed that patients who develop full-thickness PUs had a 180-day mortality rate of 68.9%, and the deaths were unrelated to the PUs — ie, the development of a full-thickness PU was a precursor, not a cause, of death.
Many patients in the ICU are mechanically ventilated and require sedation. A recent prospective observational study14 of 10 patients demonstrated that medications used to sedate ICU patients also cause changes in microcirculation and postulated this also may alter tissue perfusion. Critically ill patients also frequently develop symptoms of poor nutrition such as loss of lean tissue and reduced body mass; a review of the literature15 on nutritional support of patients experiencing multiple organ failure found that patients with multi-organ failure/dysfunction, sepsis, or systemic inflammatory response syndrome are especially at risk for malnutrition due to alterations in metabolism and absorption.15
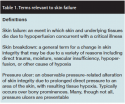 In 2008, a panel of experts17 developed a consensus statement on the concept of skin changes at life’s end (SCALE). The panel included a number of wound care experts and developed several position statements to enhance understanding and management of the physiologic changes affecting the skin and soft tissue as a result of the dying process. These changes can result in a specific type of skin ulcer known as a Kennedy Terminal Ulcer (KTU). The panel noted that not all conditions typically described as PUs are preventable. Similarly, as Yastrub16 describes in her viewpoint paper defining terminal ulcers, many clinicians mistake a KTU for a PU. However, KTUs are hypothesized to be caused by a shunting of blood away from the skin to other organs during the process of dying.18 The author further noted times during which skin damage is unavoidable. It is evident that some forms of skin failure are not well understood, and further research into the various causes of skin failure is needed. Table 1 presents definitions developed and adopted for the current study based on a compilation and analysis of sources in the literature.
In 2008, a panel of experts17 developed a consensus statement on the concept of skin changes at life’s end (SCALE). The panel included a number of wound care experts and developed several position statements to enhance understanding and management of the physiologic changes affecting the skin and soft tissue as a result of the dying process. These changes can result in a specific type of skin ulcer known as a Kennedy Terminal Ulcer (KTU). The panel noted that not all conditions typically described as PUs are preventable. Similarly, as Yastrub16 describes in her viewpoint paper defining terminal ulcers, many clinicians mistake a KTU for a PU. However, KTUs are hypothesized to be caused by a shunting of blood away from the skin to other organs during the process of dying.18 The author further noted times during which skin damage is unavoidable. It is evident that some forms of skin failure are not well understood, and further research into the various causes of skin failure is needed. Table 1 presents definitions developed and adopted for the current study based on a compilation and analysis of sources in the literature.
Other Common ICU Complications
Sepsis can induce MODS and can be an independent complication of a patient’s stay in the ICU. In a review of the components and sequelae of sepsis, Sharma and Eschun19 described sepsis as an auto-destructive process that allows extension of the patient’s response to an infection. Organ dysfunction or failure can result, and may be the first sign of sepsis. The authors point out that any organ system may be affected by sepsis, but the microcirculatory system is the key target. Sepsis affecting this system may negatively affect the ability to extract oxygen from the circulatory system, leading to tissue edema and hypoxia.
Systemic inflammatory response syndrome (SIRS) independently can lead to organ damage. Schulman and Hare’s20 review of SIRS noted “a greater incidence of sepsis in the ICU population than any other major disease”; sepsis is the main cause of ICU deaths, and more than $16 billion is spent annually in the US to manage this complication and its sequelae. The inflammatory response involved in sepsis often results in high mortality rates, even with appropriate treatment.
Acute respiratory failure (ARF) is another common complication in ICU patients. In a prospective, multicenter observational cohort study, Vincent et al21 reviewed characteristics of 458 patients admitted with ARF to participating ICUs. Characteristics associated with ARF included older patients, presence of neurologic failure, and a history of an infection during or before the ICU stay. Patients with and without ARF had mortality rates of 34% and 16%, respectively. Factors associated with death from ARF include multi-organ failure, hematologic malignancy, chronic renal failure, liver cirrhosis, circulatory shock, infection, and old age. The authors noted the presence of ARF in 56% of ICU patients. Extrapulmonary factors were found to be related to ARF and to mortality.
During a serious illness, ICU patients are also at risk for developing adrenal insufficiency (AI). In their study of 104 surgical ICU patients, Rivers et al22 found that up to 28% of seriously ill patients are found to have occult or unrecognized AI; the authors also found abnormally low levels of serum cortisol in 34 patients (32.7%). All patients in this sample met the criteria for SIRS and experienced sepsis or septic shock.
Finally, several authors have addressed malnutrition as both a cause and a consequence of ICU complications. In their prospective study, Wøien and Bjørk23 collected nutritional data from 21 critically ill patients during the first 3 days of the ICU stay and tested a feeding algorithm to enhance nutritional intake. The authors concluded that use of a method such as a nutritional support algorithm improved the delivery of nutrients in ICU patients.
Methods and Procedures
This prospective, descriptive, 18-month study consisted of a concurrent chart review of patients in adult critical care units (ICUs) who were diagnosed with acute skin failure by certified wound care nurses. The study took place in a large, tertiary care center in the southeastern US. After review and approval by a joint university and hospital Institutional Review Board, informed consent for participation was obtained from patients or family members with authority to grant consent.
All patients admitted to the adult intensive care units age 18 years or older with acute skin failure were eligible for study participation. Exclusion criteria included patients with co-existing dermatologic diagnoses such as burn wounds, exfoliative drug rashes, dermatitis, psoriasis, or Stevens-Johnson Syndrome.
After a certified wound and ostomy care nurse (CWOCN) identified eligible patients, a member of the WOCN team collected the data directly from the patient and the medical record. The data were abstracted to a collection form designed for this purpose. Demographic data abstracted from the patient’s chart included age, gender, ethnicity, date of ICU admission, date the skin problem was noted, and days spent in ICU before skin failure. Laboratory data were collected for the day skin failure was noted. In addition, based on a review of the literature, six factors were selected for investigation: organ system failures (identified by the investigators based on the medical diagnosis on the chart), nutritional status (based on feeding method and diagnoses of malnutrition or generalized edema), presence of mechanical assistive devices (eg, hemodialysis or ventilator use), support surfaces used (specialty mattresses or restraints), and provision of vasopressive or sedative drugs (as noted in the medication record).
A total sample size of 30 was desired. This size was calculated assuming an 80% power with an alpha of 0.05 for a test of significance of Pearson’s correlation coefficient against a value of zero. Calculations utilized a moderate correlation coefficient of 0.5 as an explanation of the strength of the relationship between two variables. This convenience sample satisfied the sample size required to observe significant differences.
Data analysis. Data were analyzed using PASW 17 (SPSS, Inc, Chicago, IL USA). Measures of central tendency were conducted for descriptive statistics of the sample including mean, standard deviation, and variance. Pearson’s correlation coefficients were analyzed to determine the strength of the relationship between ratio level study variables. Spearman’s rho rank-order correlation coefficient was used for categorical variables and to analyze cross-category relationships. The significance level for all correlations was set a priori at P <.05. Laboratory data were analyzed for basic statistical parameters, including mean and standard deviation. 
Results
At the conclusion of the data collection period, the total sample size was 29 patients — 20 men (69%), nine women (31%), mean age of 59 years. The average time between ICU admission and observed signs of skin failure was 7.7 days (range 0 – 30 days) (see Table 2). Patient weights ranged from 50.7 kg to 218.2 kg, with a mean of 96.3 kg (218.2 lb). Only five patients (17.2%) weighed <68 kg (150 lb); 14 patients (48.3%) weighed more than 90.7 kg (200 lb).
 Laboratory values. The majority of patients (21) had a white blood cell (WBC) count >10.5k/mcL. The mean WBC count was 18.5 k/mcL. High average BUN (mean = 48.7, range 13–126), an elevated creatinine level (mean = 2.42 mg/dL, range 0.4 – 6.0 mg/dL), and a low average albumin level (mean = 2.14 g/dL, range 1.0 – 3.9 g/dL) also were noted (see Table 2). Organ system failures observed were predominately renal failure (n = 26, 89.7%) and respiratory failure (n = 26, 89.7%). Cardiac failure (n = 10, 34.5%), hepatic failure (n = 8, 27.6%), and enteric failure, defined as a diagnosis of ileus (n = 4, 13.8%), also were observed. Sepsis was present in 18 patients (62.1%) (see Table 3).
Laboratory values. The majority of patients (21) had a white blood cell (WBC) count >10.5k/mcL. The mean WBC count was 18.5 k/mcL. High average BUN (mean = 48.7, range 13–126), an elevated creatinine level (mean = 2.42 mg/dL, range 0.4 – 6.0 mg/dL), and a low average albumin level (mean = 2.14 g/dL, range 1.0 – 3.9 g/dL) also were noted (see Table 2). Organ system failures observed were predominately renal failure (n = 26, 89.7%) and respiratory failure (n = 26, 89.7%). Cardiac failure (n = 10, 34.5%), hepatic failure (n = 8, 27.6%), and enteric failure, defined as a diagnosis of ileus (n = 4, 13.8%), also were observed. Sepsis was present in 18 patients (62.1%) (see Table 3).
Organ system failure. Five patients experienced two organ system failures at the time that skin failure was noted. Fifteen patients experienced either three organ system failures or two system failures plus sepsis, and nine patients were experiencing four or more organ system failures and/or sepsis.
When the occurrence of various combinations of organ system failures was evaluated, it was found that 23 of the 29 patients (79.3%) had diagnoses that included renal and respiratory system failures, while 15 patients (52%) had diagnoses including renal and respiratory failure as well as sepsis. Of the numerous combinations of organ system failures, these were the most frequently noted combinations.
Nutritional status. Information collected on nutritional status showed that 24 patients (82.8%) experienced generalized edema and five (17.2%) were considered malnourished at the time skin failure was noted. A total of eight patients (27.6%) were receiving enteral feeding and six (20.7%) were receiving parenteral feeding at the time the skin failure was observed.
Mechanical system assistive devices. The most prevalent device used was a ventilator. The majority of patients (25, 86.2%) were on a ventilator when skin failure was observed, and 16 (55.2%) were on continuous renal replacement therapy (CRRT). Two other assistive devices found to be in use in skin failure patients were hemodialysis (n = 6, 20.7%) and a ventricular assistive device (n = 1, 3.4%).
Pressure redistribution. Several different pressure redistribution/support surfaces were in use in the facility. Most of the patients with skin failure were on a TotalCare (Hill-Rom, Batesville, IN) mattress (n = 18, 62.1%). Others were on a Sof-Care® overlay (Gaymar Industries, Orchard Park, NY) (n = 4, 13.8%), Excel Care® with air (Hill-Rom, Batesville, IN) (n = 2, 6.9%), Excel Care® with foam (n = 1), Envision® (Hill-Rom, Batesville, IN) (n = 1), and Flexicare® (Hill-Rom, Batesville, IN) (n = 1) support surface. Wrist restraints were in use on five patients (17.2%).
Vasopressive medications. Eleven patients (11, 37.9%) were being treated with more than one vasopressive agent, nine patients (31%) were not receiving any vasopressive medication, and nine were prescribed a single agent at the time that skin failure was noted. The most common vasopressive medication in use was norepinephrine (n = 17, 58.6%), followed by vasopressin (n = 9, 31.0%). Dopamine and phenylephrine each were used in five cases (17.2%). Dobutamine and epinephrine each were used in two cases (6.9%). Milrinone was in use in one patient (3.4%) (see Table 3).
Sedatives. Sedative medications also were in common use, especially fentanyl (n = 21, 72.4%). Other sedating medications used included propofol (n = 13, 44.8%), lorazepam (n = 6, 20.7%), morphine (n = 2, 6.9%), midazolam (n = 1, 3.4%), and hydromorphone (n = 1, 3.4%) (see Table 3).
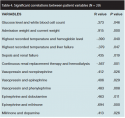 Data analysis. Analysis of the continuous variables (laboratory values, highest recorded temperature, and lowest recorded mean arterial pressure) showed a significantly positive correlation between glucose level and white blood cell count (r = .373, P = .046) and between admission weight and current weight (r = .915, P = .000 (see Table 4). However, current weight information was missing for 14 patients. Significantly negative correlations were found between highest recorded temperature and hemoglobin level (r = -.390, P = .040) and highest recorded temperature and liver failure (r = -.379, P = .047), while a positive correlation was found between sepsis and renal failure (r = .435, P = .019).
Data analysis. Analysis of the continuous variables (laboratory values, highest recorded temperature, and lowest recorded mean arterial pressure) showed a significantly positive correlation between glucose level and white blood cell count (r = .373, P = .046) and between admission weight and current weight (r = .915, P = .000 (see Table 4). However, current weight information was missing for 14 patients. Significantly negative correlations were found between highest recorded temperature and hemoglobin level (r = -.390, P = .040) and highest recorded temperature and liver failure (r = -.379, P = .047), while a positive correlation was found between sepsis and renal failure (r = .435, P = .019).
No significant correlations were found among nutritional status variables. With regard to mechanical assistive devices, only one significant correlation was found between CRRT and hemodialysis (r = -.567, P = .001). The sample size was too small and the number of variables (medication choices) too high to identify significant correlations regarding sedating medications, but several significantly positive correlations were noted with respect to vasopressive drugs. Use of vasopressin was strongly correlated with use of norepinephrine (r = .412, P = .026) and also correlated with use of epinephrine (r = .406, P = .029) and phenylephrine (r = .483, P = .008). Similarly, epinephrine was found to be positively correlated with use of dobutamine (r = .463, P = .011), and milrinone (r = .694, P = .000); the latter was also positively correlated with dopamine use (r = .413, P = .026).
Discussion
This study expanded on previous work by other authors in exploring specific factors correlated with the phenomenon of skin failure.1,3,6 It is clear skin does not fail on its own but is dependent on a number of other factors. All patients in this study (100%) were experiencing either a combination of two other organ system failures or another organ system failure plus sepsis at the time skin failure was observed. This study extends the literature on MODS by documenting specific circumstances under which the skin, as an organ system, fails. Of note: Several review articles include a discussion of skin failure, but actual research is lacking.
The following factors were present in 90% or more of patients experiencing skin failure: renal failure, respiratory failure, failure of more than one organ system (not including skin failure), or an albumin level <3.5 g/dL. Wøien and Bjørk23 previously noted that malnutrition states can be a cause of or an effect of ICU care. In this group of patients, compromised nutritional status as evidenced by a below-normal albumin level was an existing condition before skin failure in more than 90% of patients and may be a risk factor for skin failure.
Age >50 years, generalized edema, ventilator use, or a mean arterial pressure <70 mm Hg were identified in 80% or more of patients in this sample. Because ventilator use was associated with use of one or more of the sedating or analgesic medications studied, this characteristic also was found in 80% or more of the patients studied.
Additional factors associated with skin failure in 75% or more of patients included creatinine >1.5 mg/dL, weight >150 lb (68 kg), or a combination of both renal and respiratory failure (see Table 5). In his review of multiple organ failure, Deitch6 noted that identifying susceptible individuals is critical to preventing further organ system failure.
Limitations
The results of this study were subject to several limitations, including a modest sample size, restriction to a single hospital’s ICU environment, and the absence of a control group (ICU patients who did not experience skin failure). In addition, demographic variables such as gender or ethnicity were not included, and variations in the anatomic location of skin failure were not investigated. Future studies should include a larger sample size and explore time lines for skin failure, other organ system failure, and additional information about the skin lesions.
Conclusion
The skin is the body’s largest organ and it, like other organs, may experience complications, become dysfunctional, and ultimately fail. Patients in ICUs are susceptible to skin failure for a variety of reasons. Skin failure has been correlated with other organ system failures and individual patient factors. In this study, all patients had organ system failures at the time the skin failure was observed. In addition, the albumin level of 90% of the patients with skin failure was <3.5 mg/dL. The results of this study suggest that skin failure can be expected in patients with renal failure, respiratory failure, or failure of more than one organ system other than skin.
Altered nutritional status and requirements for ventilator and blood pressure/tissue perfusion support are factors known to be associated with risk for skin failure. Further research is needed to investigate this phenomenon in larger samples and in a variety of facilities. Correlations between the identified risk factors should continue to be explored, and methods to assist in preventing skin failure in susceptible individuals such as skin care, pressure-relieving surfaces, and improved nutritional management should continue to be investigated.
It is important to distinguish between skin failure, skin breakdown, and PUs, because they are not synonymous. This investigation revealed several factors associated with skin failure, a type of organ system failure that is a distinct clinical entity associated with other organ system failures and high-risk conditions. The practical implications of this study are to provide direction for enhanced management and early intervention of physiologic states found to be predictive of skin failure. Providers can be better positioned to prevent as many factors as are controllable. It is critically important to provide timely and effective management of controllable risks, because not all factors associated with skin failure are controllable in critically ill patients.
Further research is needed to investigate this phenomenon in larger samples and in a variety of facilities. Correlations between the identified risk factors should continue to be explored, and methods such as skin care, pressure-relieving surfaces, and improved nutritional management to assist in preventing skin failure in susceptible individuals should continue to be investigated.
Dr. Curry is Associate Professor/Associate Director, Department of Nursing, The University of Tampa, Tampa, FL. Ms. Kutash is a Nurse Specialist Nursing Research, College of Nursing, Tampa General Hospital, Tampa, FL. Ms. Chambers, Ms. Evans, and Ms. Holt are Wound Care Specialists, Tampa General Hospital, Tampa, FL. Ms. Purcell is a Research Resident, University of South Florida. Please address correspondence to: Kim Curry, PhD, ARNP, Department of Nursing, The University of Tampa, 401 W. Kennedy Boulevard, Box 10F, Tampa, FL 33606; email: kcurry@ut.edu.
1. Keller B, Wille J, van Ramshorst B, van der Werken C. Pressure ulcers in intensive care patients: a review of risks and prevention. Intensive Care Med. 2002;28(10):1379–1388.
2. Langouche L, Van den Berghe G. The dynamic neuroendocrine response to critical illness. Endocrinol Metab Clin N Am. 2006;35:777–791.
3. Tilney N, Bailey G, Morgan A. Sequential system failure after rupture of abdominal aortic aneurysms: an unsolved problem in postoperative care. Ann Surg. 1973;178:117–122.
4. Cerra F. Multiple organ failure syndrome. Disease-a-month. 1992;38(12):847–895.
5. Bone R, Balk R, Cerra F, Delliner R, Fein A, Knaus W, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapy in sepsis. Chest. 1992;101(6): 1644–1655.
6. Deitch E. Multiple organ failure: pathophysiology and potential future therapy. Ann Surg. 1992;216 (2):117–134.
7. Varon J, Marik P. Multiple organ dysfunction syndrome. In: Irwin RS, Rippe JM. Intensive Care Medicine. Philadelphia, PA: Lippincott, Williams, and Wilkins;1999.
8. Cerra F. Metabolic manifestations of multiple systems organ failure. Crit Care Clin. 1989;5(1):119–131.
9. Walsh C. Multiple organ dysfunction syndrome after multiple trauma. Orthop Nurs. 2005;24(5):324–333.
10. Bryant R. Anatomy and physiology of skin and soft tissue. In: Bryant R, Nix D. Acute and Chronic Wounds: Current Management Concepts, 4th ed. Philadelphia, PA: Mosby;2010:39–55.
11. Morison M, Moffatt C, Bridel-Nixon J, Bale S. A Color Guide to the Nursing Management of Chronic Wounds, 2nd ed. Philadelphia, PA: Mosby;1997.
12. Langemo D, Brown G. Skin fails too: acute, chronic, and end-stage skin failure. Adv Skin Wound Care. 2006;19(4):206–211.
13. Reger S, Ranganathan V, Sahgal, V. Support surface interface pressure, microenvironment, and the prevalence of pressure ulcers: an analysis of the literature. Ostomy Wound Manage. 2007;53(10):50–58.
14. Lamblin V, Favory R, Boulo M, Mathieu D. Microcirculatory alterations induced by sedation in intensive care patients: effects of midazolam alone and in association with sufentanil. Crit Care. 2006;10(6):R176.
15. Campbell I. Nutrition support in patients with multiple organ failure. Curr Opin Clin Nutr Metab Care.1998;1(2):211–216.
16. Brown G. Long-term outcomes of full-thickness pressure ulcers: healing and mortality. Ostomy Wound Manage. 2003;49(10):42–50.
17. Sibbald RG, Krasner DL, Lutz J. SCALE: Skin Changes at Life’s End: final consensus statement. Adv Skin Wound Care. 2010;23:225–236.
18. Yastrub DJ. Pressure or pathology: distinguishing pressure ulcers from the Kennedy Terminal Ulcer. J WOCN. 2010; 37(3):249–250. 1
9. Sharma S, Eschun G. Multisystem Organ Failure of Sepsis. Available at: www.emedicine.com/med/topic3327.htm. Accessed September 15, 2007.
20. Schulman C, Hare K. New thoughts on sepsis: the unifier of critical care. Dimen Crit Care Nurs. 2003;22 (1):22–30.
21. Vincent J, Serdar A, Menoncca A, Haji-Michael P, Sprung C, Moreno R, et al. The epidemiology of acute respiratory failure in critically ill patients. Chest. 2002;121(5):1602–1609.
22. Rivers E, Gaspari M, Saad G, Mlynarek M, Fath J, Horst H, et al. Adrenal insufficiency in high-risk surgical ICU patients. Chest. 2001;119 3):889–896.
23. Woien H, Bjork I. Nutrition of the critically ill patient and effects of implementing a nutritional support algorithm in ICU. J Clin Nurs. 2006;15(2):168–177.














