Pressure Ulcer Occurrence Following the Great East Japan Earthquake: Observations from a Disaster Medical Assistance Team
Abstract
Persons with limited mobility are at risk for pressure ulcers. The development of pressure ulcers following earthquakes has been reported secondary to disaster-related spinal cord injury. In the aftermath of the Great East Japan Earthquake, members of a Disaster Medical Assistance Team (DMAT), which included plastic surgeons and wound, ostomy, and continence (WOC) nurses working in acute care hospitals, temporary clinics, evacuation centers, and the community noticed an increase in the number of requests for pressure ulcer care. A review of hospital records and verbal reports from the community suggested that the incidence of Stage III and Stage IV pressure ulcers was 7.7% in an acute care hospital and 26.4% in home care patients — almost 10 times higher than the normal reported incidence in Japan. Patients were mostly elderly and did not have spinal cord injuries. Alternating-pressure air mattresses stopped working, alternative pressure-redistribution devices could not be delivered, caregivers could not reach the homebound, and evacuation centers did not have enough mattresses. It is believed that the high percentage of elderly living in the affected areas of Japan, combined with limited resources, manpower, and the absence of utilities, increased the number of persons with deep pressure ulcers. Following natural disasters, DMAT wound care specialists can make important contributions to the prevention of these wounds while providing much-needed care to prevent pressure ulcer-related complications. Clinician observations suggest that the risk of pressure-related injuries following a natural disaster is high, especially among the elderly.
Potential Conflicts of Interest: none disclosed
Background
On March 11, 2011, Japan experienced the Great East Japan Earthquake, one of the most powerful earthquakes anywhere in the world in recorded history. The tsunami that followed the earthquake destroyed the Pacific coast of northeast Japan. Japan’s national police agency reported that 15,854 people died in the earthquake, with 3,143 people still missing (as of March 21, 2012).1 The damage to buildings was severe, and utilities (electricity, gas, and water), communications, and transportation were nonfunctional. In particular, earthquake-triggered power failures persisted for several weeks over large areas of the Tohoku region. The disaster also inflicted serious damage to the region’s health infrastructure. Many hospitals either collapsed or were flooded, and doctors, nurses, and other health workers were injured, lost their lives, or were living in evacuation shelters.2
Stricken areas received aid from all over Japan as well as from overseas. The government mobilized the Japan Self-Defense Forces in various earthquake disaster zones. In addition, Japan received offers of assistance from a range of international leaders. The United States provided a military response to the earthquake and tsunami as part of Operation Tomodachi (friendship in Japanese). The humanitarian response included the continuous dispatch of generators, blankets, clothes, food, water, and other daily essentials from all over the world.
 Disaster Medical Assistance Teams (DMAT) also were assembled to facilitate the medical relief work required after a natural disaster of such epic proportions. The teams comprised multidisciplinary specialists: doctors and nurses to provide medical care, public health nurses offering health and sanitation advice, dietitians and nutritionists to manage nutrition-related problems, psychiatrists offering psychological help and support, pharmacists, dentists, and many other health specialists.
Disaster Medical Assistance Teams (DMAT) also were assembled to facilitate the medical relief work required after a natural disaster of such epic proportions. The teams comprised multidisciplinary specialists: doctors and nurses to provide medical care, public health nurses offering health and sanitation advice, dietitians and nutritionists to manage nutrition-related problems, psychiatrists offering psychological help and support, pharmacists, dentists, and many other health specialists.
Most of the victims died. Survivors were generally healthy or had suffered only minor injuries. At first, it appeared as if the role of healthcare professionals in the transient clinic at the evacuation area would be limited. However, within a week following the earthquake, many elderly patients residing in the evacuation centers developed pressure ulcers. An increase in the incidence of pressure ulcers also was observed in the community and in acute care hospitals. 
The Disaster Medical Assistance Team
Background. The first author joined a Disaster Medical Assistance Team (DMAT) in one of the hardest hit municipalities, Kesennuma, a coastal city in Miyagi Prefecture. Kesennuma city covers an area of 333.37 square km and has a population of 75,298 people. The percentage of elderly persons (those 65 years or older) is 30.2%. As of April 24, 2011, 856 deaths had been confirmed, and 1,137 people were officially missing in the city. Furthermore, 10,672 houses were washed away by the tsunami or destroyed by the earthquake (see Figure 1). A total of 5,739 evacuees could not return home and had to stay at one of the 67 evacuation centers.
Team members worked in acute care hospitals, temporary clinics, evacuation centers, and the community. Management of the homebound elderly presented a special challenge to the medical support team. Public health nurses visited every house in the city. They conducted interviews to identify potential medical problems; for patients who could not visit hospitals or clinics by themselves, medical care was provided through home visits by doctors and nurses.
DMAT pressure ulcer observations. Attention was soon drawn to the high incidence of pressure ulcers in the stricken area.
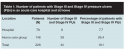 Acute care. Wound care specialists (the first author, a plastic surgeon, and wound, ostomy, and continence [WOC] nurses) in the DMAT received requests to treat patients with severe pressure ulcers in an acute care hospital (Keijinkai Otomo Hospital). Because several hospital staff members were themselves affected by the earthquake and tsunami, the number of staff members available to provide medical services was limited. The hospital had no backup power supply, and the electricity failure persisted for more than 1 month. Alternating-pressure air mattresses stopped functioning; stock of nonelectrical support surfaces was limited. Other pressure-relief devices could not be delivered for several weeks because of logistical issues arising from the disaster. Consequently, some high-risk inpatients developed pressure ulcers. Because of limited manpower, only patients with Stage III and Stage IV pressure ulcers could be treated by the DMAT wound care specialists (plastic surgeons and WOC nurses). For patients with pressure ulcers (all Stage III and Stage IV patients and some Stage I and Stage II patients), photographs of the ulcers were taken at every visit. The medical records, photographs, and plans of care were reviewed with all DMAT members during the daily morning and evening meetings. A count was kept of the number of patients with Stage III and Stage IV pressure ulcers, and facility and community pressure ulcer incidence in the aftermath of the earthquake was calculated. At the time of the authors’ hospital visit, there were 78 inpatients, six of whom developed Stage III and Stage IV pressure ulcers during the power failure (see Table 1). Four patients underwent bedside surgical debridement.
Acute care. Wound care specialists (the first author, a plastic surgeon, and wound, ostomy, and continence [WOC] nurses) in the DMAT received requests to treat patients with severe pressure ulcers in an acute care hospital (Keijinkai Otomo Hospital). Because several hospital staff members were themselves affected by the earthquake and tsunami, the number of staff members available to provide medical services was limited. The hospital had no backup power supply, and the electricity failure persisted for more than 1 month. Alternating-pressure air mattresses stopped functioning; stock of nonelectrical support surfaces was limited. Other pressure-relief devices could not be delivered for several weeks because of logistical issues arising from the disaster. Consequently, some high-risk inpatients developed pressure ulcers. Because of limited manpower, only patients with Stage III and Stage IV pressure ulcers could be treated by the DMAT wound care specialists (plastic surgeons and WOC nurses). For patients with pressure ulcers (all Stage III and Stage IV patients and some Stage I and Stage II patients), photographs of the ulcers were taken at every visit. The medical records, photographs, and plans of care were reviewed with all DMAT members during the daily morning and evening meetings. A count was kept of the number of patients with Stage III and Stage IV pressure ulcers, and facility and community pressure ulcer incidence in the aftermath of the earthquake was calculated. At the time of the authors’ hospital visit, there were 78 inpatients, six of whom developed Stage III and Stage IV pressure ulcers during the power failure (see Table 1). Four patients underwent bedside surgical debridement.
The DMAT also found that many housebound individuals in the community developed pressure ulcers. Although most were superficial or partial-thickness (Stage I and Stage II), a substantial number of patients developed Stage III and Stage IV pressure ulcers. The capacity of the hospitals was limited; all beds were occupied. Thus, patients with pressure ulcers could not be transferred to hospitals and had to be treated at home. Interviews by public health nurses revealed that 148 patients in Kesennuma City required medical care at home. Of those, 39 (26.4%) were found to have developed a Stage III or Stage IV pressure ulcer after the earthquake.
Case Reports
Typically, patients with Stage III and Stage IV pressure ulcers had necrotic tissue. Some patients had signs of systemic infection. Wound management required debridement of necrotic tissue and control of infection. The following are example case reports.
 Case 1. Mr. S was a 74-year-old man with cerebral infarction. He had been confined to bed because of joint contractures, limiting his mobility, and he was transferred to an evacuation center after the earthquake. He had several risk factors for pressure ulcers: paralysis, poor nutrition, and incontinence.3 Nevertheless, no pressure-relieving support surfaces were available at the evacuation center. Prolonged food shortages lead to nutritional impairment and weight loss. Moreover, the hygiene in the stricken area was worsened by the lack of water, gas, and hygiene products. The patient had not bathed since the earthquake, let alone used sufficient diapers and incontinence pads. Therefore, proper skin care was impossible. Three weeks after the disaster, the patient was transferred to the hospital with a high fever. He was found to have a Stage IV pressure ulcer measuring 24 cm x 14 cm on his sacral/coccygeal area (see Figure 2). The pressure ulcer had soft necrotic tissue and exhibited inflammatory redness from cellulitis. A purulent foul-smelling exudate covered the wound. The necrotic tissue was surgically debrided at the patient’s bedside under local anesthesia. The wound infection was successfully treated with systemic antibiotics and local wound care.
Case 1. Mr. S was a 74-year-old man with cerebral infarction. He had been confined to bed because of joint contractures, limiting his mobility, and he was transferred to an evacuation center after the earthquake. He had several risk factors for pressure ulcers: paralysis, poor nutrition, and incontinence.3 Nevertheless, no pressure-relieving support surfaces were available at the evacuation center. Prolonged food shortages lead to nutritional impairment and weight loss. Moreover, the hygiene in the stricken area was worsened by the lack of water, gas, and hygiene products. The patient had not bathed since the earthquake, let alone used sufficient diapers and incontinence pads. Therefore, proper skin care was impossible. Three weeks after the disaster, the patient was transferred to the hospital with a high fever. He was found to have a Stage IV pressure ulcer measuring 24 cm x 14 cm on his sacral/coccygeal area (see Figure 2). The pressure ulcer had soft necrotic tissue and exhibited inflammatory redness from cellulitis. A purulent foul-smelling exudate covered the wound. The necrotic tissue was surgically debrided at the patient’s bedside under local anesthesia. The wound infection was successfully treated with systemic antibiotics and local wound care.
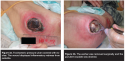 Case 2. Mr. K, a 77-year-old man, was hospitalized with pneumonia 3 months before the earthquake. He recovered from pneumonia and underwent physical rehabilitation for disuse syndrome. The earthquake hit the hospital on March 11. Many staff members were affected by the disaster, and manpower was limited. All of the alternating-pressure air mattresses stopped functioning due to power failure. The number of nonelectrical pressure-relieving devices was inadequate. The nursing staff immediately initiated a plan of care for the patient to prevent the development of pressure ulcers. The plan included placement of a standard foam mattress as a substitute for the air mattress, with repositioning every 2 hours. However, the patient could not be repositioned according to plan because of manpower shortage. He developed a trochanteric pressure ulcer covered with eschar. The wound exhibited inflammatory redness from cellulitis (see Figure 3). The eschar was removed surgically, and the purulent exudate was drained. The patient recovered from septic shock and the cellulitis was improved after the debridement.
Case 2. Mr. K, a 77-year-old man, was hospitalized with pneumonia 3 months before the earthquake. He recovered from pneumonia and underwent physical rehabilitation for disuse syndrome. The earthquake hit the hospital on March 11. Many staff members were affected by the disaster, and manpower was limited. All of the alternating-pressure air mattresses stopped functioning due to power failure. The number of nonelectrical pressure-relieving devices was inadequate. The nursing staff immediately initiated a plan of care for the patient to prevent the development of pressure ulcers. The plan included placement of a standard foam mattress as a substitute for the air mattress, with repositioning every 2 hours. However, the patient could not be repositioned according to plan because of manpower shortage. He developed a trochanteric pressure ulcer covered with eschar. The wound exhibited inflammatory redness from cellulitis (see Figure 3). The eschar was removed surgically, and the purulent exudate was drained. The patient recovered from septic shock and the cellulitis was improved after the debridement.
Discussion
The purpose of this study was to describe the occurrence and incidence of pressure ulcers following a natural disaster. Emergency medicine for victims must be a priority during the immediate aftermath of a disaster, with medical interventions focused on preventable deaths from trauma, crush syndrome, hypothermia, and drowning. However, medical requirements during the second phase (after 48 hours) change from saving lives to managing chronic medical problems.4 Many persons, even those who did not have a major acute injury or illness, could not obtain enough medication to manage chronic illnesses such as hypertension, diabetes, thrombosis, and Parkinson’s disease. Providing psychological healthcare also was challenging.5 In addition, the authors’ medical team struggled to treat many patients with pressure ulcers.
These findings suggest a high incidence of severe pressure ulcers in the devastated area during the aftermath of the earthquake. According to a report by the Japanese Society of Pressure Ulcers,6 the usual incidence of Stage III and Stage IV pressure ulcers in Japan is 0.55% in acute care hospitals and 1.67% in home care patients. These rates are similar to the reported incidence of Stage III and Stage IV pressure ulcers in the US (0.70% in acute care hospitals7 and 3.2% in home care patients8). The authors’ recent observations suggest that, following the disaster, pressure ulcer incidence was approximately 10 times higher.
An increase in pressure ulcer incidence also has been reported after other massive earthquakes, mostly as a complication of spinal cord injury sustained from the earthquakes.9,10 In contrast, most of the patients who developed pressure ulcers in the current catastrophe were elderly and did not have spinal cord injuries. This may be because fewer people suffered crush injuries in this disaster compared to the previous huge earthquakes. Japan’s National Police Agency11 reported nearly 93% of the victims of this catastrophe drowned in the tsunami.
There are several possible explanations for the observed increase in the incidence of pressure ulcers. First, the earthquake and tsunami mainly hit rural areas with a higher-than-average population of elderly residents.12 More than 30% of the population in the affected areas was elderly, versus the national average of 20.1%.2
Another possible explanation was the shortage of healthcare providers. Before the earthquake, the hardest hit areas already were trying to address a growing shortage of regional healthcare resources. That shortage was exacerbated by the destruction of hospitals, clinics, and nursing homes and loss of scarce healthcare staff.12 Manpower was limited both in the hospitals and the community during the aftermath of the disaster. Providing care for the elderly was in a chaotic state. Therefore, it appears that preventing the increased incidence of pressure ulcers was impossible from the early phase of the disaster.
Finally, the region’s infrastructure was devastated. Water, gas, and power supplies were unavailable. The logistical disruptions and supply shortages continued for several weeks after the earthquake. The evacuees had difficulty maintaining good hygiene. Food shortages led to nutritional impairments in the elderly, and some suffered weight loss and dehydration. Furthermore, alternating-pressure air mattresses, which are used widely as a standard intervention to prevent pressure ulcers in high-risk patients, stopped functioning because of the electricity failures. Substitute, nonpowered, pressure-relieving devices could not be obtained until the transportation system recovered. Most of the evacuees were forced to lie directly on the floor or on blankets.
Implications. Although emergency care immediately following disasters should remain a priority, awareness of the potential increased incidence of pressure ulcers and their subsequent complications in disaster-stricken areas should increase. Possible management strategies can be divided into four major areas: sharing information, identification of individuals at risk, relieving pressure, and proper skin care and wound treatment.
It is necessary to share knowledge and skills relating to pressure ulcer management among the medical team. Wound care specialists should play a prominent role in identifying high-risk patients and managing pressure ulcers within a multidisciplinary team. The DMAT team members had various backgrounds and specialties. A relatively small number of doctors and nurses had extensive experience in wound care. Medical records and wound photographs helped ensure consistent care.
Identifying individuals at risk for pressure ulcer development is essential. The evacuation centers received many potential high-risk individuals who may easily have been overlooked in the midst of a chaotic situation. In such circumstances, a care plan for pressure ulcer prevention should be initiated as soon as possible.
Pressure relief had to be accomplished with limited resources. Blankets and pillows were used to relieve pressure on the heels and bony prominences. However, repositioning every 2 hours to relieve pressure was difficult to achieve with limited manpower, despite the best efforts of the healthcare personnel. The inability to use powered pressure redistribution devices when the electric supply is interrupted — regardless of the cause — might be an important impetus for healthcare facilities to also have a supply of nonpowered surfaces available.
Maintaining good hygiene was another challenge because the supply of fresh water and skin care products was limited. Poor hygiene and excessive moisture should be avoided to prevent skin problems. Wet wipes and commercial moisture barriers were useful for skin care. Timely debridement and wound drainage are indispensable for pressure ulcers with necrotic tissue. Sepsis is the most serious complication of pressure ulcers; patients should be monitored for signs of infection. In a normal setting, the mortality rate is 55% among inpatients with a pressure ulcer as the probable source for sepsis.13
Conclusion
A substantial increase in the incidence of deep (Stage III and Stage IV) pressure ulcers was observed following a natural disaster. Awareness of the potential for pressure ulcer development in disaster areas may help reduce the rate of this complication. Wound care specialists can play a prominent role in the prevention and management of these wounds as part of a multidisciplinary team.
Acknowledgement
The authors gratefully acknowledge the assistance of Yukiko Miura, RN, WOCN; Yukie Sakai RN, WOCN; and all members of the Disaster Medical Assistance Team.
Dr. Sato is an Assistant Professor; and Prof. Ichioka is a Professor of the Department of Plastic and Reconstructive Surgery, Saitama Medical University, Saitama, Japan. Please address correspondence to: Shigeru Ichioka, Department of Plastic and Reconstructive Surgery, Saitama Medical University, 38 Morohongo, Moroyama, Iruma-gun, Saitama, Japan; email: ichioka2006@yahoo.co.jp.
1. National Police Agency. Damage Situation and Police Countermeasures associated with 2011Tohoku district. Available at: www.npa.go.jp/archive/keibi/biki/higaijokyo_e.pdf. Accessed March 21, 2012.
2. McCurry J. Japan: the aftermath. Lancet. 2011;377(9771):1061–1062.
3. Allman RM. Pressure ulcer prevalence, incidence, risk factors and impact. Clin Geriatr Med. 1997;13(3):421–436.
4. Furukawa K, Arai H. Earthquake in Japan. Lancet. 2011;377(9778):1652.
5. Takeda M. Mental health care and East Japan Great Earthquake. Psychiatry Clin Neurosci. 2011;65(3):207–212.
6. Japanese Society of Pressure Ulcers Surveillance Committee. Surveillance Committee Report. Jpn J PU. In press.
7. Whittington K, Patrick M, Roberts JL. A national study of pressure ulcer prevalence and incidence in acute care hospitals. J WOCN. 2000;27(4):209–215.
8. Bergquist S, Frantz R. Pressure ulcers in community-based older adults receiving home health care. Prevalence, incidence, and associated risk factors. Adv Wound Care. 1999;12(7):339–351.
9. Raissi GR, Mokhtari A, Mansouri K. Reports from spinal cord injury patients: eight months after the 2003 earthquake in Bam, Iran. Am J Phys Med Rehabil. 2007;86(11):912–917.
10. Tauqir SF, Mirza S, Gul S, Ghaffar H, Zafar A. Complications in patients with spinal cord injuries sustained in an earthquake in Northern Pakistan. J Spinal Cord Med. 2007;30(4):373–377.
11. National Police Agency. Countermeasures for the Great East Japan Earthquake Web site. http://www.npa.go.jp/hakusyo/h23/youyakuban/youyakubann.pdf Accessed March 21,2012.
12. Matsumoto M, Inoue K. Earthquake, tsunami, radiation leak, and crisis in rural health in Japan. Rural Remote Health. 2011;11(2):1759.
13. Bryan CS, Dew CE, Reynolds KL. Bacteremia associated with decubitus ulcers. Arch Intern Med. 1983;143(11):2093–2095.













