Internal Medicine Interns’ and Residents’ Pressure Ulcer Prevention and Assessment Attitudes and Abilities: Results of an Exploratory Study
Abstract
To evaluate and determine differences between attitudes of internal medicine interns and residents toward pressure ulcer (PU) prevention and to evaluate the interns’ abilities to accurately identify wounds and stage PUs, an exploratory, quantitative study was conducted in a 639-bed, safety net academic center. Participants (21 internal medicine interns and 21 internal medicine residents) attending an educational session on PU prevention and care were eligible to participate. The 1-hour conference session was prepared and provided by a physician and wound care nurses. Before the lecture, participants were asked to complete an 11-question paper-and-pencil PU attitude survey. Following the lecture, they were asked to identify 11 wounds and stage PUs using the inpatient admission history and physical template used in the hospital’s electronic medical record. An audience response system was used to record correct and incorrect responses. Nineteen (19) interns and 20 residents completed the survey. Twenty-one (21) interns successfully completed the wound assessment quiz. Descriptive statistics were used to examine the survey data and residents’ and interns’ average attitude scores were compared using independent group t-test. The results suggest that interns and residents have a positive attitude toward and are concerned about PU prevention. The significantly higher overall score among interns compared to residents (average 43.8 versus 38.8 respectively, P = 0.002) suggests interns have a more positive attitude than residents. Statistically significant differences between item scores showed that, compared to residents, interns perceived PU prevention to be more time-consuming (P = 0.01), less of a concern in practice (P = 0.02), and a lower priority than other areas of care (P = 0.003). Compared to residents, interns also were more likely to agree to with statement, “In my opinion, patients tend to not get as many pressure ulcers nowadays” (P = 0.0006). Both groups agreed that PU prevention is a greater priority than treatment and that using risk assessment tools is better than relying on clinical judgment. Wound assessment and PU staging results varied greatly, ranging from 100% for correct staging of a Stage I PU to 20% correct staging of an unstageable PU and 3% correct identification of a diabetic foot ulcer. Overall, internal medicine interns and residents have a favorable attitude toward PU prevention. Despite the limitations of this study, results suggest that enhanced medical school and residency wound care curricula are needed.
Potential Conflicts of Interest: none disclosed
Introduction
On October 1, 2008, the Centers for Medicare and Medicaid Services (CMS) added Stage III and Stage IV pressure ulcers (PUs) to the list of preventable hospital-acquired conditions, proposing to deny payment to hospitals if these conditions develop.1,2 The regulation also mandated that coders examine physician documentation for PUs.3 Historically, nurses have documented skin and wound assessments, and wound care has been an important part of nursing culture. The new CMS guideline requires physicians to be more involved and to not completely defer PU prevention and management to nursing.
 Historically, physician education has not prioritized skin and wound assessment. Per a 2005 survey of 50 American medical schools, on average, the curriculum included 2.5 hours of education on the physiology of tissue injury and 4 hours on the physiology of wound healing. Both topics were taught during the first 2 years of medical school.4 In a 2003 study involving 48 geriatric fellows,5 48% correctly identified the Braden Scale as a PU risk factor screening instrument, 67% correctly identified a description of a Stage I PU, and 52% correctly identified a Stage IV PU description. Results of a 1997 survey6 of family physicians documented that 70% did not feel adequately prepared to care for patients with PUs.
Historically, physician education has not prioritized skin and wound assessment. Per a 2005 survey of 50 American medical schools, on average, the curriculum included 2.5 hours of education on the physiology of tissue injury and 4 hours on the physiology of wound healing. Both topics were taught during the first 2 years of medical school.4 In a 2003 study involving 48 geriatric fellows,5 48% correctly identified the Braden Scale as a PU risk factor screening instrument, 67% correctly identified a description of a Stage I PU, and 52% correctly identified a Stage IV PU description. Results of a 1997 survey6 of family physicians documented that 70% did not feel adequately prepared to care for patients with PUs.
The Association of American Medical Colleges (AAMC) Geriatric Competencies for Medical Students7 acknowledges the importance of skin and wound information in undergraduate medical education. Hospital Care for Elders, one of the eight competency domains, includes PUs. Upon graduation, the medical student must be able to “conduct a surveillance examination of areas of the skin at high risk for PUs, and describe existing ulcers” in the context of caring for an older adult. How institutions are implementing these consensus recommendations has not been evaluated.
Although the limited wound and skin knowledge among medical students, geriatric fellows, and practicing family medicine physicians has been documented, medical residents’ understanding of PU prevention and care remains unclear. The purpose of this exploratory, cross-sectional study was to describe the attitudes of postgraduate medical trainees toward PU prevention and assesses their ability to correctly identify wound types and PU stage using photographs.
Methods
The study was conducted during the July 2009–June 2010 academic year at Boston Medical Center (BMC), a 639-bed, safety net academic center affiliated with Boston University School of Medicine. This project was deemed exempt from review by the Boston University Medical Center IRB because 1) the research was conducted in an established educational setting involving normal education practice, and 2) evaluation results were anonymous. There was no consent process because the educational session was part of the interns’ and residents’ usual academic curriculum.
Using a convenience sampling method, all members of the Internal Medicine residency training program rotating at BMC were eligible to participate (40 interns, 60 residents). Attendance for these conferences generally ranges from 20 to 25 participants.
Procedures. Two 1-hour educational sessions (one for residents, one for interns) were developed in collaboration with the Boston Medical Center wound care nurses. The junior (PGY2) and senior (PGY3) medical residents participated in the first session, held December 28, 2009. The interns participated in the second education session, held January 12, 2010. At the beginning of each session, participants anonymously completed an attitudes survey. Following a lecture on PU documentation and staging, they completed a visual assessment quiz.
 Instruments and data collection.
Instruments and data collection.
Attitude survey. The 11-question paper-and-pencil attitude survey, taken from the AHRQ Preventing Pressure Ulcers in Hospitals Quality Improvement Implementation Toolkit8 was used to assess the interns and residents’ attitudes regarding PU prevention. Moore and Price9 created this survey to evaluate nurses’ attitudes toward PU prevention and content validity, and survey reliability was established. The interns and residents completed this survey anonymously at the beginning of their conference. The survey uses a 5-point scale, ranging from strongly agree (1) to strongly disagree (5) (see Table 1). The lowest and highest possible scores for the attitude survey are 11 and 55, respectively. Higher scores represent a more positive attitude toward issues including preventability and participation in PU prevention.
 Visual assessment quiz. The wound care nurses created a 12-question, multiple choice, visual assessment quiz (see Figure 1). Participants completed a question about the length of time it takes for a PU to develop before the lecture part of the conference, because the wound care nurses wanted to stress the brief time period involved in this occurrence. The remaining questions, completed after the lecture, were based on 11 photographs projected onto a screen.
Visual assessment quiz. The wound care nurses created a 12-question, multiple choice, visual assessment quiz (see Figure 1). Participants completed a question about the length of time it takes for a PU to develop before the lecture part of the conference, because the wound care nurses wanted to stress the brief time period involved in this occurrence. The remaining questions, completed after the lecture, were based on 11 photographs projected onto a screen.
The wound care nurses used public domain photographs, as well as their own collection of various stages of PU and skin conditions, such as incontinence-related dermatitis, venous, vascular, or diabetic ulcers. Three wound care nurses evaluated slide accuracy/clarity without dispute. No patient details were included on the slide. The wound care nurses informed participants about the location of the wound when it was unclear from the picture. One photograph appeared on each slide for a total of 11 slides [Ed. Note: Copies of the slides are available by contacting Dr. Suen at winnie.suen@bmc.org.]
Each wound question had six to 10 possible answers based on the inpatient Admission History and Physical template in the electronic medical record. Arterial ulcers are documented as vascular ulcers in the electronic medical record; therefore, in this paper they will be referred to as vascular ulcers. If the question pertained to a PU, a follow-up question appeared asking participants to stage the PU. The staging question was provided independent of whether the participant accurately identified the picture as a PU. Participants could choose one answer per slide using the Turning Point Audience Response system™ software (Turning Technologies, Ohio) to anonymously record the percentage of participants that chose each possible answer. Residents were provided with the same visual assessment quiz, but due to technological issues with the response system, the results were not recorded and thus are missing from this analysis.
Data analysis.
Attitude survey. All responses were entered and means and standrad deviations were tabulated in a Microsoft Excel spreadsheet for Mac 2011, version 14.1.4 A free online independent group t-test calculator (Evans Research Associates, San Francisco, CA) also was used. Questions 1, 6, 7, and 11 were reverse-scored. Responses to each question were summed and averaged. Means were compared to determine variation in attitudes toward different aspects of PU care and across cohorts. Response percentages by group (interns or residents) also were calculated.
Visual assessment quiz. The percentage of correct responses to each question were retrieved from the response system software and categorized.
Results
A total of 19 internal medicine interns and 21 residents participated. All 19 interns and 20 residents completed the attitude survey. All 21 residents completed the visual assessment quiz.

Attitudes. The average attitude survey score for the interns and residents was 43.8 (range 38–51) and 38.8 (range 28–50), respectively (P <0.002) (see Table 1). Statistically significant differences between item scores showed that interns more than residents perceived PU prevention to be more time-consuming, less of a concern in practice, and a lower priority than other areas of care. Residents and interns responded fairly equally (3.84 and 3.1, respectively) to the statement, “In my opinion, patients tend to not get as many pressure ulcers nowadays.”
Visual assessment. Before the educational conference began, the intern conference audience was asked, “What length of time can it take a high-risk patient to develop a pressure ulcer?” The correct answer, “less than 2 hours,” was selected by only 13% of participants. The most common response was 4 hours (33%), followed by 8 hours (27%) and 48 hours (27%). Following the session, at least 50% of the interns were able to identify which pictures depicted a PU (range 40% to 85%). Stage I, Stage II, and Stage IV PUs and incontinence-related dermatitis were correctly identified by more than 60% of participants, but fewer than 38% of participants were able to identify Stage III, deep tissue injury, and unstageable PUs (see Table 2). When a picture of a Stage III was shown, 38% of participants chose the correct answer, but 43% chose Stage IV. When an unstageable PU picture was shown, 20% chose unstageable, but 60% of participants chose Stage IV. Lowest percent correct identification were scar tissue, venous ulcer, and diabetic foot ulcer. The percentage of correct responses to each question is shown in Figure 2. 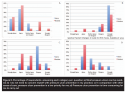
Discussion
The purpose of this study was to explore the attitudes of interns and residents toward PU prevention and their ability to correctly identify wound types and PU stage after attending a 1-hour educational session.
In general, both interns and residents at BMC had a favorable attitude toward PU prevention, but of the two groups, interns were more concerned and interested in PU prevention and treatment. In the Moore and Price study,9 the nurses had positive attitudes about PU prevention, but that did not ensure PU prevention practices were carried out; prevention was seen as too time-consuming. Interns and residents share this attitude regarding the time-consuming nature of PU prevention. A future study is needed to evaluate whether this attitude influences practice. Because this was a cross-sectional study, it is not known whether an erosion of attitudes occurs as training progresses or whether the results are reflective of this one cohort.
The main barrier toward participating in PU prevention was perceived to be and/or rooted in the attitude that it is believed to be time-consuming. Interns and residents need to learn their roles in PU prevention — through proper skin assessment and documentation — are important to the quality of care provided to patients. Although a skin assessment may take some time, depending on the patient’s functional capabilities and illness, it should be incorporated into a routine physical. Furthermore, the average score for the reverse-scored statement, “My clinical judgment is better than any pressure ulcer risk assessment tool available to me” was high in both groups (4 and 3.50 for interns and residents, respectively), suggesting that interns and residents believe in the potential benefits of using risk assessment instruments, although clinician input/judgment is valued.
Although the AAMC created a competency requirement in 2007 that includes identification of PUs as a hazard of hospitalization, those competencies are not reflected in the residents’ ability to correctly identify the wounds shown in this study, although average scores for the need to regularly assess PU risk and continuously assess patients were high (>4.0). Given the proximity of their medical school education with the 2007 AAMC competency creation, this class of intern participants may or may not have had a chance to participate in a PU curriculum. Therefore, further studies to evaluate the outcomes of these changes are needed.
Because the new CMS PU guideline requires physicians to document and stage PUs, it is imperative that physicians know how to accurately perform these tasks. In Massachusetts, the Department of Public Health considers the development of a Stage III or Stage IV PU in the hospital a “Serious Reportable Event,” based on the National Quality Forum’s10 definition of such events. Not only will each reported case be investigated, but also insurance companies may not reimburse the hospital for the full cost of the hospitalization. Misidentification of PUs can have important medical and treatment implications and financial consequences for the patient and the hospital. The potential costliness of misclassifying PUs further reinforces the importance of more extensive prevention, identification, and staging training for physicians. In this group of interns, gaps in wound identification and PU assessment skills were evident, suggesting limitations in education. The 1-hour didactic education program did not appear to be sufficient to overcome this knowledge gap.
Limitations
Several study limitations should be considered when interpreting the results. First, the sample size was small and may not be representative of all interns and residents, even at the authors’ institution. Also, the study involved only internal medicine interns and residents midway through their academic year. Perhaps resident trainees in other specialties and those later in the academic year would be more knowledgeable about PUs and have different PU prevention attitudes. Although conference topics are generally not known in advance, it is possible some participants had known the topics in advance and decided to attend the program because they are interested in the subject. Future studies should consider using a longitudinal design to assess interns’ PU prevention attitudes in their PGY2 and PGY3 years and include prevention and identification knowledge.
The limitation of assessing wounds and staging PUs using photographs is also important to consider. Studies have shown mixed inter-rater reliabilities in PU staging among general practice nurses using photographs.10-12 One study determined that, compared to noncertified nurses, certified wound, ostomy, or continence nurses had higher rates of accuracy in staging ulcers from photographs.13 Although the instrument for this study was created by an expert panel of certified wound care nurses, its validity and reliability were not tested with other wound care nurses or nonwound care experts. If the location of a wound was not clear and no one asked/clarified, the accuracy of the rating may have been compromised.
Also, the audience response system was a good way to get immediate feedback, but did not allow for provision of the correct answer. However, most of the responses were correct. The fact that the PU staging system has evolved also may affect the accuracy of the staging. The low accuracy regarding rating scar tissue, venous ulcer, and diabetic foot ulcer may be due to the fact that it was difficult to ascertain the type of wound, given that wound location was not provided upfront. Staging accuracy also may be affected by how and who taught residents about PU staging, considering the system has evolved over time.
Conclusion
Optimal PU prevention and identification are important components of patient care and require an interdisciplinary approach. The purpose of this exploratory cross-sectional study was to describe the postgraduate medical trainees’ attitudes toward PU prevention and assesses their ability to correctly identify wound types and PU stage using photographs. The results suggest that internal medicine interns and residents at one institution have favorable attitudes toward their role in PU prevention. The high reverse scores indicate a concern about PU prevention in practice and that risk assessment tools are more accurate than clinical judgment.
They believe that PU can be prevented, but that it takes too much time to do the associated prevention work. In addition, correct scores on the wound assessment quiz varied greatly, suggesting the need for additional wound assessment and PU staging education in medical training and through continuing medical education courses.
Dr. Suen is an Assistant Professor, Department of Medicine, Boston University Medical Center, Section of Geriatrics, Boston, MA. Ms. Parker is Associate Professor of Health Policy and Management, Boston University School of Public Health; and Boston University Medical Center, Section of Geriatrics. Ms. Laubenstein and Ms. Nevin are certified wound/ostomy nurses; Ms. Jansen is Director of Nursing for Inpatient Surgery; and Ms. Alexander is a certified wound/ostomy nurse, Boston University Medical Center, Nursing. Dr. Berlowitz is Center Director, Center for Health Quality Outcomes and Economic Research, Bedford, MA; Associate Chair for Research, Boston University School of Public Health; and Professor, Boston University Schools of Public Health and Medicine. Please address correspondence to: Winnie Suen, MD, MSc, LMT, Department of Medicine, Geriatrics Section, Boston University Medical Center, 88 East Newton Street, Robinson 2, Boston, MA 02118; email: winnie.suen@bmc.org.
1. Centers for Medicare and Medicaid Services (2010). Hospital Acquired Conditions. Available at: www.cms.gov/HospitalAcqCond/06_Hospital-Acquired_Conditions.asp#TopOfPage. Accessed September 1, 2010.
2. Centers for Medicare and Medicaid Services (2008). Hospital-Acquired Conditions (HAC) in Acute Inpatient Prospective Payment System (IPPS) Hospitals. Available at: www.cms.hhs.gov/HospitalAcqCond/Downloads/HACFactsheet.pdf. Accessed September 1, 2010.
3. Wound, Ostomy and Continence Nurses Society (2007). Inpatient Prospective Payment Changes: A Guide for WOC Nurse. Available at: www.wocn.org/About_Us/advocacy_and_policy/ipps_guidance/. Accessed September 1, 2010.
4. Patel N, Granick MS. American medical students are inadequately trained in wound care. Ann Plast Surg. 2007;59:53–55.
5. Odierna E, Zeleznik J. Pressure ulcer education: a pilot study of the knowledge and clinical confidence of geriatric fellows. Adv Skin Wound Care. 2003;16:26–30.
6. Kimura S, Pascala J. Pressure ulcers in adults: family physicians knowledge, attitudes, practice preferences, and awareness of AHCPR guidelines. J Fam Pract. 1997;44(4):361–368.
7. Leipzig RM, Granville L, Simpson D, Anderson MB, Sauvigne K, Soriano RP. Keeping granny safe on July 1: a consensus on minimum geriatrics competencies for graduating medical students. Acad Med. 2009;84(5):604–610.
8. AHRQ Preventing Pressure Ulcers in Hospitals Quality Improvement Implementation Toolkit (in publication). Available at: www.ahrq.gov/research/ltc/pressureulcertoolkit/. Accessed March 12, 2012.
9. Moore Z, Price P. Nurses’ attitudes, behaviors and perceived barriers towards pressure ulcer prevention. J Clin Nurs. 2004;13:942–951.
10. Allcock N, Wharrad H, Nicolson A. Interpretation of pressure-sore prevalence. J Adv Nurs. 1994;20(1):37–45.
11. Healy F. The reliability and utility of pressure sore grading scales. J Tissue Viabil. 1995;5:111–114.
12. Russell LJ, Reynolds TM. How accurate are pressure ulcer grades? An image-based survey of nurse performance. J Tissue Viabil. 2001;11(2):67–75.
13. Hart S, Bergquist S, Gajewski B, Dunton N. Reliability testing of the National Database of Nursing Quality Indicators Pressure Ulcer Indicator. J Nurs Care Qual. 2006;21(3):256–265.













