Heel Ulcer Incidence Following Orthopedic Surgery: A Prospective, Observational Study
Abstract
People undergoing orthopedic surgery receive care at many points along the healthcare continuum. Although heel pressure ulcer (HPU) incidence in the orthopedic population has been reported to be 13.3%, information is limited. The purpose of this prospective observational study was to evaluate: 1) the cumulative incidence of HPUs in orthopedic patients across the continuum of care, and 2) the outcome of HPUs once they occurred.
Of the 72 study participants (average age 76 ± 16 years, 60% women, 53% required surgery for hip fractures), 57 were recruited consecutively upon admission to a rehabilitation center from one of two acute care facilities and 15 were assessed upon admission to one of the acute care sites and at discharge to the home. All but two study participants were followed-up in the community 1 month after discharge from the acute care or rehabilitation facility. Medical charts were reviewed and study participants underwent a bedside assessment, with direct examination of both heels and staging of the ulcer at admission and discharge. The cumulative incidence of HPUs was 17% (95% CI 8%–26%). All ulcers were identified upon admission to the rehabilitation center; 41% of HPUs were either suspected deep tissue injury (sDTI) or unstageable. Both of the Stage I and two of the five Stage II ulcers were resolved at the time of follow-up; three of the five sDTI or unstageable ulcers were unresolved. HPUs occurred in 17% of people undergoing orthopedic procedures. All ulcers occurred in acute care and severe ulcers persisted while patients received rehabilitation and community care. This is the first study to follow orthopedic patients across the continuum of care.
Potential Conflicts of Interest: This research project was funded by the Registered Nurses Association of Ontario, Canadian Nurses Foundation, London Health Sciences Center, and St. Joseph’s Health Care London.
 Pressure ulcers (PU) are a common and serious health concern. Prospective studies involving acute surgical patients have provided similar estimates of cumulative PU incidence in the Netherlands (21.2%)1 and in the U.S. (21.5%).2,3 In other prospective research conducted in European countries, cumulative HPU incidence in acute care patients with fractured hips was found to range from 16% to 66%.4,5-7 The highest incidence of PU (66%) was observed in an acute care study conducted in England among older participants (70 to 94 years).4 A Pan European study7 involving six countries in the north and south of Europe prospectively followed a large sample (635 participants) from admission to discharge and reported a 16% cumulative PU incidence, the majority of PUs classified as Stage I, suggesting they were less severe.
Pressure ulcers (PU) are a common and serious health concern. Prospective studies involving acute surgical patients have provided similar estimates of cumulative PU incidence in the Netherlands (21.2%)1 and in the U.S. (21.5%).2,3 In other prospective research conducted in European countries, cumulative HPU incidence in acute care patients with fractured hips was found to range from 16% to 66%.4,5-7 The highest incidence of PU (66%) was observed in an acute care study conducted in England among older participants (70 to 94 years).4 A Pan European study7 involving six countries in the north and south of Europe prospectively followed a large sample (635 participants) from admission to discharge and reported a 16% cumulative PU incidence, the majority of PUs classified as Stage I, suggesting they were less severe.
Several US studies8-10 have reported a prospectively determined 0% cumulative PU incidence in rehabilitation centers and the community. Cumulative PU incidence in retrospective studies has been estimated to be 6% in rehabilitation centers11,12 and 3.2% in individuals living in the community.13 In a retrospective study of a similar population of community-dwelling seniors in the UK, Margolis et al14 reported an incidence rate of 0.58 PU per hundred persons. Although study comparison is hampered by the different methods employed, this research might suggest that PU incidence in all anatomical locations tends to be lower in rehab and community care settings compared to acute care facilities.
Heel pressure ulcer (HPU) incidence is of particular interest in the orthopedic population but information about HPU incidence in the orthopedic population in Canada is limited. Campbell et al15 conducted a prospective study among orthopedic patients in an acute care facility in Canada and followed participants from admission to the average length of stay (LOS = 5 days) or discharge, whichever came first. The estimated HPU incidence in this population was found to be 13.3%. Because people undergoing orthopedic surgery receive care at many points along the healthcare continuum and in many healthcare settings, it is important to understand when and where most HPUs develop. Care sites often blame each other for causing HPU. The purpose of this prospective study was to evaluate: 1) the cumulative incidence of HPUs in orthopedic patients across the continuum of care, and 2) the outcome of HPUs once they occurred.
Wide variations in PU incidence estimates may be due to clinical practice change and the type of healthcare setting where PU incidence is estimated. In a prospective, randomized, controlled study5 that followed 146 patients over the age of 65 with fractured hips in Sweden, a change in practice was found to significantly reduce the incidence of all PUs from 55% to 29%; unfortunately, details about the change in practice were not completely described in this study. One practice that seems to affect PU incidence in the hip fracture population is wait time for emergency surgery. In Ontario, once patients are admitted they may have to wait in the emergency department for a bed. Once a bed is available, they wait to be cleared medically for the operating room (OR) and then for OR time to be made available, all the while bedbound in pain and potentially without being able to eat or drink. Results from a prospective study (N = 850) conducted by Al-Ani et al16 demonstrated that the cumulative incidence of PU occurring in people with hip fractures was 6% when participants waited less than 24 hours for surgery and 10% for those who waited longer.
Unique features of clinical practice within different healthcare delivery models may help explain large variations in PU incidence reported in different countries. For example, in Canada demand for total joint replacement surgeries has increased markedly. Between 1994 and 2004, knee and hip surgeries increased 51% and 114%, respectively.17 This has created a need for a specific strategy to reduce wait times for elective joint replacement surgeries in Canadian acute care facilities; this strategy has resulted in progressive decline in average LOS in acute care to 5 days, with some patients discharged home as early as 24 hours post surgery. Given the variations in clinical practice that exist across geographical locations, national estimates of PU incidence in each specific country need to be obtained.
In studies conducted in Europe, the US, and Canada,1,6,18-22 the heel has been identified as the most common or second most common site for PU. HPUs are different than those located on other parts of the body. The shape of the heel makes offloading pressure more difficult unless the heel is lifted directly off the bed. The calcaneus bone has a pointed shape with little subcutaneous fat, which makes it vulnerable to pressure.23 In two studies of heel perfusion, blood flow was found to be highest with complete pressure relief.1,24 This explains why prevention strategies with the PU located on the heel require a specialized approach different than prevention strategies for other parts of the body.
A recent publication by Campbell et al15 suggests a need to develop heel ulcer prevention programs for this acute orthopedic patient population. However, people undergoing orthopedic surgery receive care at many points along the healthcare continuum and in many healthcare settings. For example, patients can enter the system through the emergency department (ED) or through the OR. Once discharged from acute care, people can go to long-term care, rehabilitation, home with home care services, or home with no further care. This patient population’s care continuum makes prevention planning challenging — the complexity of implementing a prevention program across facilities and in different levels of care can be prohibitive. A simpler approach would be to focus prevention strategies where and when an orthopedic population is at greatest risk of developing a HPU. For this to be accomplished, it must be determined where across the continuum of care HPUs most commonly occur. Because HPUs can take time to fully develop, it is difficult to discern whether a specific point of care is associated with heel ulcer development or if HPUs develop gradually over an extended postoperative period.
Methods
A sample of orthopedic patients was followed as they entered or exited acute care hospitals and rehabilitation centers and after they returned home to the community.
Setting. The research took place in an urban center in Ontario, Canada. Two levels of care within three sites in the city were included in the study. One location was an academic tertiary care facility with a total of 850 beds that has two acute care sites in same city. The first acute care site (AC1) features 36 inpatient acute orthopedic surgery beds; in this non-trauma center, 1,300 elective hip and knee replacements are performed annually and 200 patients with fractured hips are treated each year. The second acute care site (AC2) is the trauma center for the region; the orthopedic unit has 35 beds for people undergoing non-elective surgeries and four beds in the Critical Care Trauma Unit. The rehabilitation (Rehab) center has 50 beds and receives most of its patients from AC1. The criteria for admission to rehabilitation are 1) the need for rehabilitation in a center with 24-hour care and/or 2) the need for rehabilitation and simultaneous geriatric inpatient care.
Ethics approval. Before beginning the study, ethics approval for the project was obtained from the research ethics board at the local university as well as the individual review boards at the three hospitals.
Inclusion/exclusion criteria. Recruitment took place at AC2 and the Rehab center. Individuals at AC2 who underwent lower extremity orthopedic surgery due to an elective or emergency procedure were recruited to participate in the study. Participants were included if they were >18 years of age and they or their substitute decision maker provided written informed consent to participate in the research study. Individuals were excluded if they were actively dying, already had a heel ulcer, or if it was impossible to examine their heels due to extreme pain or because a cast or other device covered the heels.
Study design. In this prospective observational study, a convenience sample of patients (n = 72) admitted to AC2 and the Rehab center were approached from December 2006 to August 2007 (see Figure 1). Participants either were discharged directly home from AC2 (n = 15) or were referred to the Rehab site (n = 57) before going home. The majority of study participants (n = 57) were recruited consecutively upon admission to the Rehab center from either AC1 (n = 35) or AC2 (n = 22) and not assessed in AC2; a subset of participants (n = 15) was assessed on admission and discharge form AC2. These participants went directly home and were assessed there 1 month later. If the participant had an HPU on admission to Rehab, it was assumed to have occurred in one of the two acute care sites. Patients were reassessed at discharge from Rehab to see if a HPU had occurred while the patient was in rehabilitation. If a HPU was noted on admission to Rehab, researchers reported whether the HPU evolved or resolved over the course of rehabilitation. Fifteen (15) participants were recruited while in AC2 and were assessed at admission and at discharge or at the average LOS (7 days). Because these patients did not require an inpatient rehabilitation stay, they were discharged and followed at home for 1 month. All but two of the 70 study participants were followed in the community 1 month after discharge from either AC2 or Rehab.
Study procedures. Each individual underwent a bedside assessment, including direct examination of both heels, completion of the Braden Risk Assessment Scale, and a medical chart review. The use of any therapeutic surfaces or heel protective devices also was noted. A skin assessment of both heels was again performed at the bedside on admission at AC2 or Rehab and at discharge from the facility (or after average LOS).
All noted HPUs were staged according to 2007 National Pressure Ulcer Advisory Panel (NPUAP) definitions.25 All evaluations were conducted by seven wound care experts who had participated in a training session involving several patients who had PUs located on any part of the body. During this training session, consensus was reached among all assessors regarding the interpretation of the new NPUAP staging definitions. Stage I PUs were identified using a clear transparent disk to ensure that nonblanchable erythema was actually present. This method has been tested by Vanderwee et al,26 who suggested that the clear disk was better than using a finger for observing nonblanchable erythema. This method had been rated as more reliable in the sacrum than the heel; the authors suggested that patients’ heels be assessed with the participant lying supine, which makes direct observation of the heel more difficult.
Statistical analysis. Data were entered into SPSS, version 13 (SPSS, Inc., Chicago, IL). Descriptive statistics were utilized to describe all variables. The incidence estimates were expressed as percentages of people with HPUs with 95% confidence intervals (CI).27
Results
Demographic information. The average age of all study participants was 76±16 years, 60% were women, and 53% required surgery after sustaining a hip fracture (see Table 1). Participants admitted from AC2 who went directly home were younger than persons from AC1, the majority were men (77%), and they were admitted most often for fractures to the lower limbs. Of patients who were referred from the acute care facilities to the Rehab, 61% had undergone surgery following a hip fracture. Participants recruited in the Rehab Center had more frequent neurological problems, were over- or underweight, and had blood transfusions; participants in AC2 had more frequent problems with delirium, dementia, peripheral vascular disease (PVD), and diabetes than participants who went directly home.
Incidence. The cumulative incidence of HPU in these orthopedic patients was 17% (95% CI 8%–26%). All HPUs were identified on admission to the Rehab center. Of those, 10 out of 12 (83%) came from AC1. Specifically, of the 35 participants admitted to Rehab from AC1, 30% had a HPU compared to two of the 22 (5%) admitted from AC2. One participant with a HPU that was noted in acute care later developed a second ulcer on the opposite heel. In this case, the second HPU was not counted in the incidence estimate. Three participants with heel ulcers on both heels were counted only once. No heel ulcers were identified during assessments of patients in AC2 and no patients discharged directly to their homes from AC2 had a HPU. However, two of the 22 people with HPUs detected on admission to Rehab were discharged from AC2. The incidence of new HPUs in Rehab and in the community was 0%.
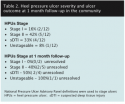
Pressure ulcer severity. Of the HPUs that occurred, 41% were classified as sDTI or as unstageable (see Table 2). The sDTI ulcers had intact skin with tissue damage below the dermis. The most frequent type of PU observed was a relatively superficial Stage II (42%). Only 16% of HPUs identified were Stage I PU. Of the HPUs believed to occur in acute care, six out of 12 (50%) were still present after rehabilitation (average LOS 30 days) and/or 1 month after returning home. At 1 month after discharge to the community, both Stage I ulcers had resolved, two out of five (40%) Stage II ulcers had not resolved, and three out of five (60%) of the sDTI and unstageable ulcers had not resolved. Of the four sDTI ulcers, two resolved and two were unstageable; one ulcer that was initially found to be unstageable remained unstageable 1 month after discharge to the community.
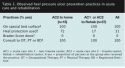
Facility practices. All study participants (100%) were provided therapeutic surfaces (see Table 3). All beds in AC1 and AC2, as well as the Rehab facility, had at least a high-specification foam replacement mattress. HPU prevention device use was common in AC2 — 72% of participants utilized devices such as regular hospital pillows for heel elevation. Despite a system-wide hospital initiative to assess all patients for PU risk, no risk assessment was completed by nurses at any site. All participants were referred for either physical or occupational therapy. In AC2, no participants were referred to the rehab department (RD); whereas, 41% of participants were referred to an RD while in the Rehab setting.
Discussion
Study findings support results of previously published reports5,7 that HPUs in orthopedic patients occur in the acute care facility. Results also suggest that prevention efforts should focus on acute care facilities and that current efforts to prevent these ulcers in the community and rehabilitation facilities are effective.
Incidence estimates. The cumulative HPU incidence in this orthopedic patient population was 17% (95% CI 8%–26%). This estimate for HPUs is similar to, but slightly higher than, results from the authors’ previous study15 conducted among orthopedic patients (HPUs incidence of 13.3%, (95% CI to be 8%–18%) but within the confidence interval.
The current estimate of HPUs incidence in the orthopedic population is higher than the 0% to 9.1% previously reported by Frain et al,28 who used a prospective design to examine HPUs occurrence in orthopedic patients in a US long-term care facility (n = 40).
In the current study, the HPUs incidence estimate in this specific orthopedic population is similar to previous reports of HPUs incidence occurring in a general acute care population. In a retrospective chart audit29 reviewing skin surveys of all patients admitted to medicine or surgery in an acute care facility (N= 237), the cumulative HPUs incidence was found to be 13.5%. A prospective study by Tourtual et al30 estimated the cumulative incidence of HPUs in a US acute care facility was higher (26.8%), but this study included only patients from four care units (n = 291) that had the highest prevalence of PU, and selecting high-risk care units may account for the relatively high HPUs incidence reported.
The current study did not identify any new heel ulcers in these patients while they were in rehabilitation or at home. Prospective studies8-10 have reported an incidence of 0% in all PU in rehabilitation facilities, and retrospective chart reviews11,12 have estimated the incidence of all PU in rehabilitation settings to be 6%. The results of the current study are also consistent with a prospective study9 that estimated a 0% cumulative PU incidence in any anatomical location in community-dwelling patients. These findings are lower than the estimated cumulative incidence of 3.2% reported in the results of a retrospective study31 (n = 1,711) that examined the overall cumulative incidence of PU in the community with patients receiving home care.
Impact of data collection methods. Data collection methods seem to be an important determinant in estimating PU incidence. Prospectively determined cumulative incidence estimates are reported to be 8.8% to 19.1% lower than those of researchers using retrospective chart reviews8,9 to examine PU in the hip fracture population. Research in Sweden32 that compared a retrospective chart audit to a prospective study using direct physical exam of patients in surgical, orthopedic, medical, and geriatric departments found a 14.3% PU prevalence using retrospective chart audit and a 33.3% prevalence when patients were examined prospectively. These results suggest that PU incidence estimates using a retrospective approach that relies on accurate PU charting may not provide an accurate estimate of the extent of the problem.
To further confound this area of research, one must be aware of how the incidence value is reported. Although incidence is consistently defined as “the proportion of a group initially free of the condition that develops the condition over a period of time,”32 the manner by which it is estimated can vary. Most often, cumulative incidence is provided, which is defined as the probability of developing the disease over a period of time27; in hospital, the time frame is often the average length of stay (LOS). Some studies report the incidence rate, defined as the rate at which new cases of a disease occur in a population within a specific timeframe.27,33 Although both approaches to estimating incidence are valid, values derived from the different calculations cannot be compared.
Ulcer resolution. The outcome of all HPUs detected in this orthopedic population also was reported. All Stage I HPUs had resolved; these findings are similar to work done in Holland where researchers found that half (50%) of the Stage I ulcers resolved 1 week after initial assessment.33 In the current study, 40% of participants with Stage II HPUs, seen 1 month after discharge, still had HPUs and 60% of sDTI or unstageable ulcers were unresolved after 1 month in home care. These results suggest that more severe ulcers are less likely to resolve quickly and may require continued care for many weeks in rehabilitation and community care.
Staging. Of all HPUs seen in the current study, 16% were Stage I, a much lower estimate than reported in other studies. Two other studies15,29 of HPUs in acute care found that 85% to 100% of the HPUs were classified as Stage I. In the current study, a clear disk rather than the finger method was used to determine whether a PU was a Stage I. The earlier descriptive study26 suggests the clear disk has advantages over using the finger when observing nonblanchable erythema but that it has lower inter-rater reliability with HPUs compared to PUs located over the sacrum. Differences in the method of assigning Stage I PUs may account for variations in the proportion of HPUs that were considered Stage I PU.
Limitations
Limitations to this study include the fact that two of the 57 patients were lost to follow-up; it is possible these individuals could have developed HPUs without the authors’ knowledge.
Also, no subjects were discharged home from AC2 with a HPUs — an unexpected finding because this acute care site received acutely ill patients following an unexpected fracture or trauma.
The accuracy of the HPUs incidence estimate for AC2 is questionable because a sampling bias may have occurred in this patient population. The sample population recruited at AC2 site represented a very small proportion of the total orthopedic population. Because of competing studies involving this patient population at this acute care site, only 15 participants were recruited over a 9-month period; as a result, AC2 participants were younger and healthier and used heel protection more frequently than those in AC1. Because subjects were recruited consecutively as they entered the Rehab Center from AC1 or AC2, the authors believe this HPUs incidence estimate is more accurate. Also, because the sample populations recruited from the Rehab center and AC2 were so different, their information was reported separately.
Conclusion
HPUs occurred in 17% of people undergoing elective (joint replacement surgery) or emergency (hip fracture repair) orthopedic procedures. All heel ulcers occurred in acute care; 41% were sDTI or unstageable. The more severe HPUs (60% of the ulcers studied) remained in patients who underwent rehabilitation and required continued treatment in community care. Prevention programs for HPUs should focus on acute care where new HPUs first occur. Research to increase understanding about the development of HPUs should be conducted with specific high-risk patient populations (eg, medicine, ICU, cardiovascular surgical procedures) and include prospectively assessments across the continuum of care.
Dr. Campbell is an Advanced Practice Nurse, London Health Sciences Center, University Hospital, London, Ontario, Canada. Dr. Woodbury is an Assistant Professor, School of Physical Therapy, University of Western Ontario; Adjunct Lecturer Dalla Lana School of Public Health, University of Toronto; and research consultant, Canadian Association of Wound Care, Toronto. Ms. Labate and Ms. LeMesureir are Nurse Clinicians, St. Joseph’s Health Care, London, Parkwood Hospital, London, Ontario. Dr. Houghton is Chair, Graduate Program, Health and Rehabilitation, School of Physical Therapy, University of Western Ontario. Please address correspondence to: Dr. Karen Campbell, London Health Sciences Center, University Hospital, 339 Windermere Road, London, Ontario NSX 1G2, Canada; email: Karen.campbell@sjhc.london.on.ca.
1. Schoonhoven L, Defloor T, Grypdonck MHF. Incidence of pressure ulcers due to surgery. J Clin Nurs. 2002;11(4):479–487.
2. Schultz A, Bien M, Dumond K, Brown K, Myers A. Etiology and incidence of pressure ulcers in surgical patients. AORN J. 1999;70(3):434–449.
3. Hicks DJ. An incidence study of pressure sores following surgery. ANA Clinical Sessions. 1970:49–54.
4. Versluysen M. How elderly patients with femoral fracture develop pressure sores in hospital. Br Med J. 1986;292(6531):1311–1313.
5. Gunningberg L, Lindholm C, Carlsson M, Sjödén P. Reduced incidence of pressure ulcers in patients with hip fractures: a 2-year follow-up of quality indicators. Int J Qual Health Care. 2001;13(5):399–407.
6. Versluysen M. Pressure sores in elderly patients. J Bone Joint Surg. 1985;67(1):10–13.
7. Lindholm C, Sterner E, Romanelli M, et al. Hip fracture and pressure ulcers — the Pan-European Pressure Ulcer Study — intrinsic and extrinsic risk factors. Int Wound J. 2008;5(2):315-328.
8. Hunter SM, Cathcart-Silberberg T, Langemo DK, et al. Pressure ulcer prevalence and incidence in a rehabilitation hospital. Rehabil Nurs. 1992;17(5):239–242.
9. Langemo DK, Olson B, Hunter S, Hanson D, Burd C, Cathcart-Silberberg T. Incidence and prediction of pressure ulcers in five patient care settings. Decubitus. 1991;4(3):25–30.
10. Cuddigan J, Berlowitz DR, Ayello EA. Prevalence, incidence, and implications for the future: an executive summary of the national pressure ulcer advisory panel. Adv Skin Wound Care. 2001;14(4):208–215.
11. Schue RM, Langemo DK. Prevalence, incidence, and prediction of pressure ulcers on a rehabilitation unit. J WOCN. 1999;26(3):121–129.
12. Schue RM, Langemo DK. Pressure ulcer prevalence and incidence and a modification of the Braden Scale for a rehabilitation unit. J WOCN. 1998;25(1):36–43.
13. Bergquist S, Frantz R. Pressure ulcers in community-based older adults receiving home health care. Prevalence, incidence, and associated risk factors. Adv Wound Care. 1999;12(7):339–351.
14. Margolis DJ, Bilker W, Knauss J, Baumgarten M, Strom BL. The incidence and prevalence of pressure ulcers among elderly patients in general medical practice. Ann Epidemiol. 2002;12(5):321–325.
15. Campbell KE, Woodbury MG, Houghton PE. Incidence and risk factors of heel pressure ulcers in an acute orthopedic population. Ostomy Wound Manage. 2010:56(2):44–54.
16. Al-Ani AN, Samuelsson B, Tidermark J, et al. Early operation on patients with a hip fracture improved the ability to return to independent living: a prospective study of 850 patients. J Bone Joint Surg — Series A. 2008;90(7):1436–1442.
17. Bourne RB, DeBoer D, Hawker G, et al. Total hip and knee replacement. Access to Health Services in Ontario: ICES Atlas. 2005.
18. Vangilder C, MacFarlane GD, Meyer S. Results of nine international pressure ulcer prevalence surveys: 1989 to 2005. Ostomy Wound Manage. 2008;54(2):40–54.
19. Bours GJ, Halfens RJ, Lubbers M, Haalboom JR. The development of a national registration form to measure the prevalence of pressure ulcers in The Netherlands. Ostomy Wound Manage. 1999;45(11):28–36.
20. Barczak CA, Barnett RI, Childs EJ, Bosley LM. Fourth national pressure ulcer prevalence survey. Adv Wound Care. 1997;10(4):18–26.
21. Goodridge DM, Sloan JA, LeDoyen YM, McKenzie J, Knight WE, Gayari M. Risk-assessment scores, prevention strategies, and the incidence of pressure ulcers among the elderly in four Canadian health-care facilities. Can J Nurs Res. 1998;30(2):23–44.
22. Horn SD, Bender SA, Bergstrom N, et al. Description of the national pressure ulcer long-term care study. J Am Geriatr Soc. 2002;50(11):1816–1825.
23. Mayrovitz HN, Sims N. Effects of different cyclic pressurization and relief patterns on heel skin blood perfusion. Adv Skin Wound Care. 2002;15(4):158–164.
24. Huber J, Reddy R, Pitham T, Huber D. Increasing heel skin perfusion by elevation. Adv Skin Wound Care. 2008;21(1):37–41.
25. National Pressure Ulcer Advisory Panel. NPUAP Announces New Pressure Ulcer Definition and Staging. Adv Skin Wound Care. 2007;20:184–187.
26. Vanderwee K, Grypdonck MHF, De Bacquer D, Defloor T. The reliability of two observation methods of nonblanchable erythema, Grade 1 pressure ulcer. Appl Nurs Res. 2006;19(3):156–162.
27. Baumgarten M. Designing prevalence and incidence studies. Adv Wound Care. 1998;11(6):287–293.
28. Frain R. Decreasing the incidence of heel pressure ulcers in long-term care by increasing awareness: results of a 1-year program. Ostomy Wound Manage. 2008;54(2):62–67.
29. McElhinny ML, Hooper C. Reducing hospital-acquired heel ulcer rates in an acute care facility: an evaluation of a nurse-driven performance improvement project. J WOCN. 2008;35(1):79–83.
30. Tourtual DM, Riesenberg LA, Korutz CJ, et al. Predictors of hospital acquired heel pressure ulcers. Ostomy Wound Manage. 1997;43(9):24–34.
31. Gunningberg L, Ehrenberg A. Accuracy and quality in the nursing documentation of pressure ulcers: a comparison of record content and patient examination. J WOCN. 2004;31(6):328–335.
32. Frantz RA. Measuring prevalence and incidence of pressure ulcers. Adv Wound Care. 1997;10(1):21–24.
33. Halfens RJG. Relevance of the diagnosis 'stage 1 pressure ulcer': an empirical study of the clinical course of stage 1 ulcers in acute care and long-term care hospital populations. J Clin Nurs. 2001;10(6):748–757.














