Chronic Wounds Treated With a Physiologically Relevant Concentration of Platelet-rich Plasma Gel: A Prospective Case Series
Abstract
Chronic wounds are characterized by a long inflammatory phase that hinders regenerative wound healing. The purpose of this prospective case series was to evaluate how a physiologically relevant concentration of an autologous platelet-rich plasma (PRP) gel affects initial wound healing trajectories of chronic, nonhealing wounds of various etiologies and in different care settings.
Using convenience sampling methods, 49 patients (average age: 60.6 years, SD 14.7) with 65 nonhealing wounds (mean duration 47.8 weeks, range 3 to 260) at eight long-term acute care (LTAC) hospitals and three outpatient foot or wound clinics who were prescribed PRP gel for their nonhealing wound were enrolled. The majority of patients had low albumin, hematocrit, and/or hemoglobin levels. After wound assessments and measurements were obtained and the gel prepared, a skin barrier was applied to the periwound skin and the gel applied and protected with cover dressings. The most common wounds were pressure ulcers (n = 21), venous ulcers (n = 16) and diabetic foot ulcers (n = 14). Mean wound area and volume were 19 cm2 (SD 29.4) and 36.2 cm3 (SD 77.7), respectively. Following a mean of 2.8 (SD 2.4) weeks with 3.2 (SD 2.2) applications, reductions in wound volume (mean 51%, SD 43.1), area (39.5%, SD 41.2), undermining (77.8%, SD 28.9), and sinus tract/tunneling (45.8%, SD 40.2) were observed. For all wound etiologies, 97% of wounds improved. The results of this study suggest the application of this PRP gel can reverse nonhealing trends in chronic wounds.
Potential Conflicts of Interest: Ms. Fylling, Ms. Rappl, and Dr. Clausen are employees of Cytomedix, Inc. Relevant Concentration of Platelet-rich Disclaimer: The contents do not represent the views of the Department of Veterans Affairs or the Indian Health Service of the United States Government.
Chronic wounds come with cost and morbidity for patients and for society. In 2006, the Advanced Medical Technology Association1 (Advamed) reported that the management and treatment of chronic and complex wounds cost the US an estimated $20 billion per year. These wounds are found in all types of healthcare settings and are a challenge for the healthcare provider.
Since the 1980s, efforts to improve clinical outcomes have explored the use of growth factor-based therapies.2 Approaches include: 1) single growth factors, 2) multiple growth factors in releasates derived from purified platelets, and growth factor-rich products made from platelet-rich plasma (PRP) produced using various methods. Approaches to therapies using single growth factors have included the clinical evaluation of platelet-derived growth factor (PDGF [becaplermin], marketed as Regranex®, Systagenix Wound Management, Quincy, MA), basic fibroblast growth factor (bFGF), epidermal growth factor (EGF), granulocyte-macrophage colony stimulating factor (GM-CSF), and keratinocyte growth factor -2 or KGF-2 (studied as Repifermin, Human Genome Sciences, Rockville, MD). Unfortunately, the promising pre-clinical data of single growth factors for wound healing used in animal models have not been realized clinically.3 In a review of published clinical studies on topical application of individual growth factors and hormones, Braund et al3 reported that epidermal growth factor (EGF), bFGF, and acidic fibroblast growth factor (aFGF), and PDGF all have shown mixed results; transforming growth factor-beta (TGF-b) showed no significant differences; and human growth hormone (hGH) impeded wound healing. KGF-2 has shown positive results. To date, recombinant PDGF is the only single-growth-factor therapy approved by the US Food and Drug Administration (FDA) for use in wound healing.4
A multitude of growth factors, including vascular endothelial cell growth factor (VEGF), EGF, PDGF, fibroblast growth factor (FGF-2), and dozens of others are released by platelets at sites of wounding. In vitro analysis has shown that each growth factor is a signaling molecule responsible for a specific activity in the wound healing cascade of events necessary to natural organized wound healing.3,5-7 Everts et al8 postulated that the need for these multiple growth factors to drive effective healing may explain the limited effectiveness of single growth factors to improve wound healing.
Early efforts to develop a multiple growth factor therapy considered that platelets — as first responders in the wound healing process — release hundreds of growth factors, chemokines, and cytokines that regulate angiogenesis, new tissue deposition, and regeneration.9,10 Investigators created releasates (platelet-derived wound healing formula – PDWHF) from purified platelets to access the natural complement of all growth factors inherent within the platelet.11 Results of prospective, randomized, controlled trials (RCTs) involving wounds of various wound etiologies,12-15 retrospective wound healing,11,16-18 and amputation prevention studies19,20 involving more than 10,000 patients have shown that growth factor-rich releasates from thrombin-activated platelets are effective in healing a variety of chronic wounds and preventing amputations. Although this PDWHF showed promise, difficulties around production, characterization, and commercial availability made it obsolete and led to the need for improvements in the formulation of growth factor-rich products by activating autologous PRP.
There are many methods to derive PRP and process that plasma into a product for topical wound application. All involve the use of a centrifuge to fractionate blood, separating the red blood cells from the platelet-rich plasma. Important differences in centrifugation methods involve speed, velocity, acceleration, deceleration, and angulation and radius of the rotor of the centrifuge.21,22 Other differences in methods of processing the plasma involve the activation of the platelets by adding various kinds of thrombin, thrombin with calcium chloride, calcium chloride alone, or baproxobin to the PRP and using a freeze-thaw method that lyses the platelets to access the contents. This last method creates a lysate rather than a releasate, which provides a different biologic end-product.22-25 Some preparations include red blood cells and/or leukocytes in the resulting gel; preparations vary in their platelet concentrations and the consistency of the resulting gel. Several authors have stated that much of the reported variability in wound healing outcomes following the use of PRP likely is due to the diversity of devices, methods, and clinical strategies used to obtain and apply PRP derived products.22,26-28 Thus, results obtained using one method may not be representative of all methods used for preparation of PRP. Thoughtful consideration of the method, PRP end-product, and documented clinical results is important to distinguish the appropriate system and formulation.
In late 2007, the AutoloGel™ System (Cytomedix, Inc. Rockville, MD) for the preparation of PRP gel received FDA clearance for marketing and use of the gel on exuding wounds, such as leg ulcers, pressure ulcers, and diabetic ulcers and for the management of mechanically or surgically debrided wounds.29 This system uses a proprietary method that produces autologous PRP gel from plasma containing a physiological concentration of platelets that comprise a full complement of growth factors, chemokines, and cytokines. This nonconcentrated, physiologically equal, or “physiologically relevant” strength is important in light of severalin vitro studies that have shown that gels derived from platelet concentrates can negatively impact cell growth and migration.30-32 This PRP gel produces a clean end-product containing minimal or no contaminating erythrocytes or leukocytes. In contrast, other FDA-cleared systems are used to produce PRP for orthopedic indications where the PRP often is mixed with bone graft materials. These systems yield concentrates containing supra-physiological levels of growth factors in addition to varying levels of contaminating erythrocytes and leukocytes.33
In 2006, Driver et al34 published the results of a prospective, multicenter, randomized, blinded, controlled trial of this PRP gel (n = 35). In the most common-sized diabetic foot ulcers, healing occurred in 81.3% of the wounds treated with PRP gel versus 42.1% treated with saline gel (P = 0.036). The results of this study increased interest in the use of autologous PRP gel for the care of diverse wounds, especially difficult-to-heal wounds in patients with comorbid conditions.
The purpose of this prospective case series was to evaluate how autologous PRP gel derived from physiological concentrations of platelets affects initial wound healing trajectories of chronic or nonhealing wounds of any etiology in any care setting.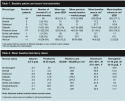
Methods and Procedures
Enrollment. Using convenience sampling methods, patients at eight long-term acute care (LTAC) hospitals and three outpatient foot or wound clinics who were prescribed PRP gel for their nonhealing wound between December 15, 2008 and June 18, 2009 were enrolled. Persons were eligible for the study if: 1) they had an open, cutaneous wound that the clinician determined was not progressing toward healing, 2) the wound had a mostly clean wound bed just before product application, and 3) their wound(s) were without clinical signs and symptoms of active infection — all criteria must be met. Exclusion criteria were: 1) malignancy in the wound bed or 2) current use of chemotherapy. Each treating clinician was familiar with the patient and/or had first-person knowledge or records of prior treatment with other therapeutic interventions and the response of the wound to those treatments that indicated the lack of healing progress of the wound.
During this study, the rights and dignity of all patients involved were protected by compliance with the Health Insurance Portability and Accountability Act (HIPAA) regulations vis-à-vis sharing de-identified aggregate data for study purposes as per the National Institutes of Health Authorization for Research Uses and Disclosures. According to the HIPAA Privacy Rule,35 Internal Review Board approval and informed consents were not required because the data were gathered by clinicians during normal clinical care and all protected health information about the patients were de-identified before analysis.
Treatment procedure. A verbal treatment description was provided to every patient in preparation for the procedural steps and to maximize the patient’s role in positioning, offloading, and cover dressing changes. The patient was positioned comfortably and dressings were removed. Before initial and subsequent gel treatments, the wound bed was cleaned thoroughly using sharp debridement (aggressive or conservative), mechanical debridement, cleansing with a wound cleanser and gauze, or ultrasound. The treating clinician measured the wound, recorded the results, and applied a moisture barrier preparation on the intact periwound skin. Clinicians previously trained by the manufacturer on appropriate preparation and handling prepared the PRP gel in accordance with the Instructions for Use included within the product’s dressing kit. A venipuncture was performed on the patient and ≤20 mL of blood was drawn. Collected blood was spun for 60 seconds in a specially designed centrifuge calibrated to provide physiological concentration of platelets dispersed through a plasma fraction that is readily discernable from the red blood cells and buffy coat containing leukocytes. The PRP fraction was transferred into a mixing chamber and ascorbic acid and calcified thrombin were added to activate the platelets, convert fibrinogen to fibrin, and ensure appropriate formation of the PRP gel. Immediately after the PRP liquid converted to a clear gelatinous consistency (usually within 15 to 30 seconds), the gel was applied topically to the wound and covered with a nonabsorbent contact layer dressing to help hold the gel in place followed by a moisture vapor-permeable film dressing and a secondary absorbent dressing to manage any strikethrough. Appropriate offloading devices such as support surfaces, heel lifts, or plantar surface offloading shoes or braces needed for the individual wound were used. For the patients described here, the PRP gel was applied once or twice a week depending on the characteristics of the wound and the physician’s or treating clinician’s judgment.
Wound measurements. Treating clinicians who had been provided training and materials on the measurement technique described obtained all measurements. Cotton-tipped applicators were used to probe and disposable paper rulers with centimeter markings were used to measure length, width, and depth of the visible wound as well as undermining, and sinus tracts and tunneling (ST/T). Measurements were taken and recorded just before each gel application as well as before each dressing change and when gel treatment was discontinued at the clinician’s discretion.
Length and width of the wound opening were measured using the standard “clock face” method described by Sussman.36 Length was 12:00 to 6:00 with 12:00 toward the head, width was 3:00 to 9:00. Depth measurement was taken from the deepest point of the wound bed to the level of usual skin surface and at a 90° angle to skin surface.
In wounds with undermining or ST/T, a more thorough measurement was taken. A clock face was superimposed over the wound bed and measurements of undermining at each of four points (12, 3, 6, and 9 o’clock) were recorded. These measurements then were totaled to arrive at a single number, the linear totalfor undermining, to be used in data analysis of this parameter. Locations of ST/T also were noted using the same four points and measurements taken and recorded. The measurements of the ST/T also were totaled to arrive at a single number, the linear total for ST/T, to be used in data analysis of this variable.
 Other variables. If available at the time of the first patient treatment, the following variables also were collected: age, treatment facility type and location, wound etiology, wound location, wound severity (by grading or full-/partial-thickness with exposed tendon or bone), previous wound duration, and laboratory tests including hemoglobin, hematocrit, platelet counts, and albumin or pre-albumin levels. If more than one wound on a patient was treated with PRP gel, the wounds were numbered consecutively for identification. In this study, data on more than one wound per patient are included. Other documented clinician observations including comments on exudate, periwound condition, maceration, tissue color, and healing pattern also were collected.
Other variables. If available at the time of the first patient treatment, the following variables also were collected: age, treatment facility type and location, wound etiology, wound location, wound severity (by grading or full-/partial-thickness with exposed tendon or bone), previous wound duration, and laboratory tests including hemoglobin, hematocrit, platelet counts, and albumin or pre-albumin levels. If more than one wound on a patient was treated with PRP gel, the wounds were numbered consecutively for identification. In this study, data on more than one wound per patient are included. Other documented clinician observations including comments on exudate, periwound condition, maceration, tissue color, and healing pattern also were collected.
Data analysis. The data were collected using a paper/pencil data collection sheet and then entered into a Microsoft Excel spreadsheet containing formulas to calculate area, volume, linear totals for undermining and ST/T, and provide descriptive statistics. Wound area was calculated using the formula for an ellipse: length x width x 0.7854 (an ellipse is closer to a wound shape than a square or rectangle that would be described by simple length x width). The use of an ellipse for calculating wound measurement has been used in a database of more than 120,000 wounds37 and in RCTs in wound healing literature.38 Volume was calculated using the formula (length x width x 0.7854) x depth. The figures used for analyzing undermining or ST/T were the linear totals taken at the four points described. Treatment outcome was defined as percent of change for area, volume, undermining, and ST/T and was calculated as initial measurement minus assessment day measurement divided by initial measurement. Descriptive statistics were used for all demographic variables, change in the wound measurements, length of treatment time, and the number of treatments with PRP gel. Descriptive statistics also were used to describe outcomes by wound etiology, lab values (eg, low or normal albumin), and to compare outcomes for patients with low or normal lab values and patients older/younger than 65 years because the latter two are characteristics associated with poor wound healing.39,40
Clinical relevance, defined as the potential of a therapy providing positive results in a group of patients, the magnitude of the response, the length of time, and the number of treatments to achieve the response also was evaluated. In a healthcare system trying to save time and money with the best impact of a modality, this concept assists clinicians in determining efficient modalities of treatment.41 All patients enrolled were included in the analysis.

Results
Study enrollees comprised 49 patients with 65 chronic wounds, 35.4% of which had areas of undermining and 15.4% had ST/T. Pressure ulcers, venous ulcers, and diabetic foot ulcers were the most prevalent wounds. The mean previous wound duration without healing was 47.8 weeks (SD 62.4). Mean baseline wound area was 19 cm2 (range: 0.2 to 194.8 cm2) and volume was 36.2 cm3 (range: <1.0 to 447.7 cm3). For patients for whom age was reported, the mean age was 60.6 years (SD 14.7) (see Table 1). The mean age of patients <65 years of age (n = 22) was 50.2 years (SD 8.5; range: 25 to 63) and of patients ≥65 years of age (n = 14) was 74.8 years (SD 8.0; range 65 to 89). The laboratory values of the majority of patients, irrespective of wound etiology, were below normal in all categories except platelet count (see Table 2).
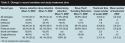
For all etiologies combined during a mean treatment time of 2.8 weeks (SD 2.4) with 3.2 (SD 2.2) PRP applications, mean wound volume decreased 51% (SD 43.1), area decreased 39.5% (SD 41.2), undermining decreased 77.8% (SD 28.9), and ST/T decreased 45.8% (SD 40.2) (see Table 3). Treatment time ranged from 1.9 weeks for dehisced wounds to 3.9 weeks for diabetic wounds (see Table 3).
In the same timeframe, the proportion of wounds responding and the amount of the response for all etiologies included: in 58 out of 65 (89.2%) of the wounds, volume decreased 62% (SD 30.5), in 55 out of 65 (84.6%) area decreased 50.9% (SD 32.1), and in 23 out of 23 (100%) of the wounds with undermining and/or ST/T was reduced 77.8% (SD 28.9) and 45.8% (SD 40.2), respectively (see Table 4). No systemic or wound site side effects were noted. Occasionally, maceration around the periwound was noted if that tissue was not protected with moisture barriers or if the dressings were not changed according to directions. Only two of 65 wounds either increased in size or remained unchanged. In the patient with sickle-cell disease, wound volume decreased 82.6% and in the two patients with arterial disease wound volume decreased 65.2% with four treatments.
Patients with low albumin levels (<3.5 g/dL), in 11 out of 15 (73.3%) average wound volume decreased 64% (SD 35.1) in 1.7 weeks (SD 0.9) with 3.2 treatments (SD 1.3). In 19 out of 24 (79.1%) patients with low hemoglobin (<12 g/dL), average volume decreased 64.4% (SD 30.8) in 2.1 weeks (SD 1.0) with 3.4 treatments (SD 1.5). In 17 out of 21 (81%) patients ≥65 years, average volume decreased 74.4% (SD 31) in 3 weeks (SD 3.0) with 3.3 treatments (SD 2.7)
Discussion
Inflammation is a normal initial phase in the cycle of events needed to heal a wound. In normal wound healing, the inflammatory phase resolves within a few days, the wound stops sending pro-inflammatory signals, and new tissue synthesis or proliferation begins. Chronic wounds tend to be characterized as being “stuck” in the inflammatory phase; this is believed to be the most significant factor in delaying the healing of chronic wounds.42 The wounds in this study had a mean previous wound duration of 47.8 weeks and mean baseline area of 19 cm2 and volume of 36.2 cm3, representative of chronic wounds. The response of these long-standing wounds to, on average, 3.2 PRP gel treatments over 2.8 weeks suggests they moved out of the inflammatory phase and resumed progress toward healing.
The wounds described herein comprised all common chronic wound types — ie, arterial, dehisced, diabetic, pressure ulcers, sickle cell-related, surgical/trauma, and venous, many with undermining and/or ST/T. Different wound etiologies have characteristic shapes. Diabetic foot ulcers typically have a small area and a large volume due to their depth. In contrast, venous ulcers have a large area but the volume is small due to shallow depth. Pressure ulcers and some diabetic ulcers also have undermining and/or ST/T. Reviewing only area or volume changes does not reflect the changes in these dimensions of the wound. The data collected and analyzed in this study included multiple measurement parameters: area, volume, undermining, and ST/T. This strategy provides sensitivity to changes in wound progress for each of the considered parameters.
The decrease in mean wound size documented in this analysis is more rapid than reported in previous literature. For example, in a retrospective study of 400 persons with pressure ulcers, diabetic ulcers, and venous ulcers receiving a wide variety of treatment modalities, Jones et al43 documented that only 12.75% of the wounds healed in 3 months.
In the present case series, a majority of the patients for whom lab results were available had below-normal values for albumin, pre-albumin, hemoglobin, and hematocrit. Low blood chemistry values have been equated with diminished wound healing.39 The results in this study demonstrate that wounds in compromised patients can progress toward wound healing with PRP gel. Similarly, although the sample size was small, wound area reductions were observed in patients with arterial (n = 2) and sickle-cell disease (n = 1), well-known risk factors for poor healing.44,45
 Subjective clinician observations also were noted. Many reported seeing a change in undermining and ST/T respond first, volume second, and area last. In addition, during the first week of treatment, a noticeable decrease in exudate and increase in healthy granulation tissue were observed. Through experience, clinicians discovered it was important to protect the surrounding tissues and apply the dressing correctly. Experience also improved the speed of processing PRP gel.
Subjective clinician observations also were noted. Many reported seeing a change in undermining and ST/T respond first, volume second, and area last. In addition, during the first week of treatment, a noticeable decrease in exudate and increase in healthy granulation tissue were observed. Through experience, clinicians discovered it was important to protect the surrounding tissues and apply the dressing correctly. Experience also improved the speed of processing PRP gel.
The PRP gel for this case series was produced from a physiologically equal concentration of platelets, a distinguishing feature compared to other PRP preparations. This aspect of the end-product is of importance, considering well-established findings that many cellular receptors, including those critical to wound healing, respond to their growth factor, cytokine, and chemokine ligands with bell-shaped dose response kinetics.46-49 This means that too little ligand produces little or no response, physiologic amounts of ligand produce optimal response, and high concentrations of ligand produce little or no response. Such bell-shaped dose-response kinetics are explained by several mechanisms of receptor down-regulation and desensitization50,51 and it is not surprising that this basic tenent in cell biology is consistent with observations made about PRP products produced with calcified thrombin and various concentrations of platelets. For example, in vitro studies30,52-55 from several different laboratories demonstrate that thrombin-activated PRP derived from high concentrations of platelets can negatively affect cell proliferation and chemotaxis and can even cause programmed cell death.
The use of this activated gel derived from physiologic concentrations of platelets is intended to provide growth factors, cytokines, and chemokines at concentrations within the therapeutic limits of bell-shaped dose-response curves. Consideration of the use of platelet gels derived from physiologic concentrations of platelet may be prudent for indications such as wound healing where PRP is not diluted but applied directly to the site of tissue damage. In addition, the gel formulation utilized in the present study incorporates ascorbic acid, which preserves the consistency of the PRP gel and drives deposition of granulation tissue by increasing collagen expression,56,57 collagen hydroxylation, and export of collagen for the incorporation of appropriately folded collagen fibrils.58
The results of this case series appear to confirm observations from the basic science of wound repair; in >97% of wounds, a positive change in wound variables was observed following application of physiologically relevant concentration of platelets, even in wounds in older and medically compromised patients.
These findings are important because, while prospective RCTs remain the gold standard for determining treatment efficacy,59 these studies often do not include the medically compromised patients treated in the current case series. Carter et al59 reviewed inclusion/exclusion criteria from 17 wound-care RCTs and found that more than 50% of 3,210 patients from 18 outpatient wound centers would have been excluded from 15 of the 17 studies because of common comorbidities and the complexity of their wounds.
In an economic analysis60 considering the total care of a patient when a diabetic ulcer remains nonhealing, including the potential for infection, amputation, and death, the same PRP gel formulation was found to be the most cost effective therapy compared to standard care using wet-to-moist dressings and offloading and other advanced therapies over a 5-year period. Its impact on stalled negative pressure wound therapy-treated wounds also has been demonstrated in a case series61 of three patients.
Limitations
A limitation of the study is that patients were not available for ongoing follow-up to the endpoint of complete healing due to early discharge from facilities. In addition, clinicians determined treatment and dressing change frequency. Long-term outcomes studies of higher-risk patients with multiple comorbidities and large wounds using prospective RCTs are needed to evaluate the efficacy of various advanced wound treatment modalities.
Conclusion
A study of PRP gel derived from physiological concentrations of platelets showed the product can be utilized by healthcare providers in various healthcare settings to restart the healing process in complex chronic wounds, even wounds recalcitrant to other treatments, and in patients with advanced age, compromised lab values, and comorbidities. Sixty-three (63) of 65 wounds (97%) responded with reductions in area, volume, undermining, and/or ST/T in a mean of 2.8 weeks with 3.2 treatments. These results have important clinical implications and suggest this treatment can reverse the nonhealing trend in chronic wounds.
Acknowledgements
The authors acknowledge Judy M. Beriou, RN, MHA, CLNC, Cytomedix, Inc. for assistance in data gathering and tabulation, and the staff of the 11 sites that provided the care and gathered the data.
1. AdvaMed Advanced Medical Technology Association. Advanced Wound Management: Healing and Restoring Lives. Available at: www.advamed.org. Accessed June 9, 2010.
2. Hunt T, Van FL. Enhancement of wound healing by growth factors. N Engl J Med. 1989;321(2):111–112.
3. Braund R, Hook S, Medicott NJ. The role of topical growth factors in chronic wounds. Curr Drug Delivery. 2007;4:195–204.
4. Papanas N, Maltezos E. Becaplermin gel in the treatment of diabetic neuropathic foot ulcers. Clin Interv Aging. 2008;3(2):233–240.
5. Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev. 2003;83(3):835–870.
6. Singer AJ, Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341(10):738–746.
7. Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008;16(5):585–601.
8. Everts PA, Brown Mahoney C, Hoffmann JJ, et al. Platelet-rich plasma preparation using three devices: implications for platelet activation and platelet growth factor release. Growth Factors. 2006;24(3):165–171.
9. Knighton DR, Fiegel VD, Phillips GD. Regulation of cutaneous wound healing by growth factors. Clin Materials. 1991;8(3-4):229–241.
10. Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004;91:4–15.
11. Knighton DR, Ciresi KF, Fiegel VD, Austin LL, Butler EL. Classification and treatment of chronic nonhealing wounds. Successful treatment with autologous platelet-derived wound healing factors (PDWHF). Ann Surg. 1986;204(3):322–330.
12. Knighton DR, Ciresi K, Fiegel VD, Schumerth S, Butler E, Cerra F. Stimulation of repair in chronic, nonhealing, cutaneous ulcers using platelet-derived wound healing formula. Surg Gynecol Obstet. 1990;170(1):56–60.
13. Atri SC, Misra J, Bisht D, et al. Use of homologous platelet factors in achieving total healing of recalcitrant skin ulcers. Surgery. 1990;108:508–512.
14. Steed DL, Goslen JB, Holloway GA, Malone JM, Bunt TJ, Webster MW. Randomized prospective double-blind trial in healing chronic diabetic foot ulcers. CT-102 activated platelet supernatant, topical versus placebo. Diabetes Care. 1992;15(11):1598–1604.
15. Holloway GA, Steed DL, DeMarco MJ, et al. A randomized, controlled dose response trial of activated platelet supernatant, topical CT-102 in chronic, nonhealing, diabetic wounds. Wounds. 1993;5:160–168.
16. Keyser, JE. Diabetic wound healing and limb salvage in an outpatient wound care program. South Med J. 1993;86:311–317.
17. Glover JL, Weingarten MS, Buchbinder DS, et al. A four-year multicenter retrospective study of topical multiple growth factor therapy for chronic wounds. Adv Wound Care. 1997;10(1):27–32.
18. Margolis DJ, Kantor J, Santanna J, et al. Effectiveness of platelet releasate for the treatment of diabetic neuropathic foot ulcers. Diabetes Care. 2001;24:483–488.
19. Knighton DR, Fylling CP, Fiegel VD, et al. Amputation prevention in an independently reviewed at-risk diabetic population using a comprehensive wound care protocol. Amer J Surg. 1990;160:466–472.
20. Doucette MM, Fylling CP, Knighton DR. Amputation prevention in a high-risk population through a comprehensive wound healing protocol. Arch Phys Med Rehabil. 1989;70:780–785.
21. Roukis TS, Zgonis T, Tiernan B. Autologous platelet-rich plasma for wound and osseous healing: a review of the literature and commercially available products. Adv Ther. 2006;23(2):218–237.
22. Arora NS, Ramanayake T, Ren YF, Romanos GE. Platelet-rich plasma: a literature review. Implant Dent. 2009;18(4):303–310.
23. Anitua E, Sanchez M, Orive G, Andia I. The potential impact of the preparation rich in growth factors (PRGF) in different medical fields. Biomaterials. 2007;28(31):4551–4560.
24. Lundquist R, Dziegiel MH, Agren MS. Bioactivity and stability of endogenous fibrogenic factors in platelet-rich fibrin. Wound Repair Regen. 2008;16(3):356–363.
25. Frechette JP, Martineau I, Gagnon G. Platelet-rich plasma: growth factor content and roles in wound healing. J Dent Res. 2005;84(5);434–439.
26. Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg. 2004;114(6)1502–1508.
27. Ficarelli E, Bernuzzi G, Tognetti E, et al. Treatment of chronic venous leg ulcers by platelet gel. Dermatol Ther. 2008;21(suppl 1):S13–S17.
28. Smith S, Roukis T. Bone and wound healing augmentation with platelet-rich plasma. Clin Podiatr Med Surg. 2009;26(4):559–588.
29. FDA 510K clearance, BK060007. AutoloGel System. Rockville, MD: Cytomedix, Inc; September 20, 2007.
30. Han J, Meng HX, Tang JM, Li SL, Tang Y, Chen ZB. The effect of different platelet-rich plasma concentrations on proliferation and differentiation of human periodontal ligament cells in vitro. Cell Prolif. 2007;40:241–252.
31. Weibrich G, Hansen T, Kleis W, Buch R, Hitzler WE. Effect of platelet concentration in platelet-rich plasma on peri-implant bone regeneration. Bone. 2004;34(4):665–671.
32. Graziani F, Ivanovski S, Cei S, Ducci F, Tonetti M, Gabriele M. The in vitro effect of different PRP concentrations on osteoblasts and fibroblasts. Clin Oral Implants Res. 2006;17(2):212–219.
33. Savarino L, Cenni E, Tarabusi C, et al. Evaluation of bone healing enhancement by lyophilized bone grafts supplemented with platelet gel: a standardized methodology in patients with tibial osteotomy for genu varus. J Biomed Mater Res B Appl Biomater. 2006;76(2):364–372.
34. Driver VR, Hanft J, Fylling, Beriou JM, and AutoloGelTM Diabetic Foot Ulcer Group. A prospective, randomized, controlled trial of autologous platelet-rich plasma gel for the treatment of diabetic foot ulcers. Ostomy Wound Manage. 2006;52(6):68–87.
35. U.S. Department of Health and Human Service. National Institutes of Health. HIPAA Privacy Rule. Available at: http://privacyruleandresearch.nih.gov/pr_08.asp#8b. Accessed January 10, 2010.
36. Sussman C. Wound measurements. In: Sussman C, Bates-Jensen B (eds). Wound Care: A Collaborative Practice Manual for Physical Therapists and Nurses. Gaithersburg, MD: Aspen; 2001:120–141.
37. Margolis DJ, Kantor J, Berlin JA. Healing of diabetic neuropathic foot ulcers receiving standard treatment: a meta-analysis. Diabetes Care. 1999;22:692–695.
38. Blume PA, Walters J, Payne W, Ayala J, Lantis J. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: a multicenter randomized controlled trial. Diabetes Care. 2008;31(4):631–636.
39. Fonder MA, Lazarus GS, Cowan DA, Aronson-Cook B, Kohli AR, Mamelak AJ. Treating the chronic wound: a practical approach to the care of nonhealing wounds and wound care dressings. J Am Acad Dermatol. 2008;58(2):185–206.
40. Pittman J. Effect of aging on wound healing: current concepts. J WOCN. 2007;34(4):412–415; quiz 416-417.
41. Snappinn SM, Jiang Q. Responder analysis and the assessment of a clinically relevant treatment effect. Trials. 2007;8:31.
42. Hart J. Inflammation 2: its role in the healing of chronic wounds. J Wound Care. 2002;11(7):245–259.
43. Jones KR, Fennie K, Lenihan A. Chronic wounds: factors influencing healing within 3 months and nonhealing after 5–6 months of care. Wounds. 2007;19(3):51–63.
44. Eckman JR. Leg ulcers in sickle cell disease. Hematol Oncol Clin North Am. 1996;10(6):1333–1344.
45. Chung C, Cackovic M, Kerstein MD. Leg ulcers in patients with sickle cell disease. Adv Wound Care. 1996;9(5):46–50.
46. Wu DT, Bitzer M, Ju W, Mundel P, Bottinger E. Concentration specifies differential signaling of growth arrest/differentiation and apoptosis in podocytes. J Am Soc Nephrol. 2005;16:1–11.
47. Lucas PA, Caplan AI. Chemotactic response of embryonic limb bud mesenchymal cells and muscle-derived fibroblasts to transforming growth factor-β. Connective Tissue Research.1988;18:1–7.
48. Brown RA, Kamaljit KS, Gwanmesia I, Raemdonck D. Enhanced fibroblast contraction of 3D collagen lattices and integrin expression by TGF-β1 and –β3: mechnoregulatory growth factors? Exper Cell Res. 2002;274:310–322.
49. Gruber B, Marchese M, Kew R. Angiogenic factors stimulate mast-cell migration. Blood. 1995;86:2488–2493.
50. Lin F, Butcher EC. Modeling the role of homologous receptor desensitization in cell gradient sensing. J Immunol. 2008;181:8335–8343.
51. Bohm S, Grady EF, Bunnett NW. Regulatory mechanisms that modulate signaling by G-protein-coupled receptors. Biochem J. 1997;322:1–18.
52. Choi BH, Zhu SJ, Kim BY, et al. Effect of platelet rich plasma (PRP) concentration on the viability and proliferation of alveolar bone cells, an in vitro study. Int J Oral Maxillofac Surg. 2005;34:420–424.
53. Krasna M, Domanovic D, Tomsic A, Svajger U, Jeras M. Platelet gel stimulates proliferation of human dermal fibroblasts in vitro. Acta dermatoven APA. 2007;16(3):105–110.
54. Rughetti A, Giusti I, D’Ascenzo SD, et al. Platelet gel-released supernatant modulates the antiogenic capability of human endothelial cells. Blood Transfus. 2008;6:12–17.
55. Clausen C, Hermund NU, Donatsky O, Nielsen H, Osther K. Homologous activated platelets stimulate differentiation and proliferation of primary human bone cells. Cell Tiss Organ. 2006;184:68–75.
56. Houglum KP, Brenner DA, Chojkier M. Ascorbic acid stimulation of collagen biosynthesis independent of hydroxylation. Am J Clin Nutr. 1991;54:1131S–1143S.
57. Murad S, Grove D, Lindberg KA, Reynolds G, Sivarajah A, Pinnell SR. Regulation of collagen synthesis by ascorbic acid. Proc Natl Acad Sci. 1981;78(5):2879–2882.
58. Canty EG, Kadler KE. Procollagen trafficking, processing and fibrillogenesis. J Cell Science. 2005;118:1341–1353.
59. Carter MJ, Fife CE, Walker D, Thomson B. Estimating the applicability of wound care randomized controlled trials to general wound-care populations by estimating the percentage of individuals excluded from a typical wound-care population in such trials. Adv Skin Wound Care. 2009;22(7):316 –324.
60. Dougherty EJ. An evidence-based model comparing the cost-effectiveness of platelet-rich plasma gel to alternative therapies for patients with nonhealing diabetic foot ulcers. Adv Skin Wound Care. 2008;21(12):568–575.
61.Gurvich L. Synergism in using negative pressure wound therapy with alternated applications of autologous platelet-derived growth factors in treating post-acute surgical wounds. Wounds. 2009;21(5):134–140














