A Simple Device for Closure of a Colocutaneous Fistula within the Laparotomy Wound: A Case Report
Abstract
Colocutaneous fistulas within laparotomy wounds are rare and difficult to treat. Surgical repair may be contraindicated or not desired and negative pressure wound therapy may not be successful. A simple device made from a silicone, flexi-aid hand exerciser was used to close a colocutaneous fistula within the laparotomy wound of a 50-year old man following surgery of an esophageal carcinoma and a surgical history of Whipple’s procedure for adenocarcinoma of the ampulla of Vater.
His wound developed 9 days postoperatively, measured 8 cm x 3 cm x 2 cm, and was contaminated with fecal material. Initial efforts involving cleansing and the use of negative pressure wound therapy were unsuccessful and the patient refused additional surgery. In this patient, a silicone occlusion device, used in conjunction with a silver hydrofiber dressing, prevented fecal soiling and facilitated closure of the colocutaneous fistula and the laparotomy wound. He was discharged on postop day 22 and healed by postop day 64. This was the first time this approach was used. Studies to optimize nonsurgical management approaches of these complicated conditions are needed.
Please address correspondence to: Dr. Ming-Ho Wu, 670 Chung-Te Rd, Tainan, Taiwan, 701 ROC; email: m2201@mail.ncku.edu.tw.
A colocutaneous fistula resulting from leakage of the colocolostomy within the laparotomy wound after esophageal reconstruction is rare (in the authors’ facility, three colocutaneous fistula in 150 esophageal reconstructions, approximately 2%).1 Because negative pressure therapy is not always successful in the treatment of open abdominal wounds and colocutaneous fistula,2 a major laparotomy with intestinal resection as well as resection of the colocutaneous fistula often is necessary. Surgical treatment of these fistulas is difficult and associated with high morbidity and mortality rates.3 Fecal soiling from the colocutaneous fistula usually interferes with the patient’s daily activities.4 In consideration of these challenges, a nonsurgical modality for management of a colocutaneous fistula and laparotomy wound involving the design of an occlusion device is presented.
Case Report
History. Four years before presenting to the authors, another surgeon performed a Whipple’s procedure for adenocarcinoma of the ampulla of Vater on 50-year-old Mr. H; subsequently, Mr. H received adjuvant chemoradiotherapy. More recently, Mr. H, who had no additional comorbidities, underwent a thoracoscopic subtotal esophagectomy and transverse colon interposition for squamous cell carcinoma of the esophagus. On postoperative day 9, a colocutaneous fistula developed at the upper middle portion of the laparotomy wound, which was an upper middle line incision. The wound, which measured 8 cm x 3 cm x 2 cm, was contaminated with stool from the fistula. Initial efforts (postoperative days 9  through 11) were directed toward cleansing and irrigation. To address drainage containment, negative pressure wound therapy (20 mm Hg) was administered on postoperative days 12 through 17 and throughout this period Mr. H required dressing changes every 2 to 3 hours, which disturbed his sleep. The periwound skin was irritated and painful. When he began oral intake of food, the drainage thickened and stool passed through the fistula, not the anus. Abdominal CT and colon study demonstrated the presence of a colocutaneous fistula within the laparotomy wound. Mr. H refused surgery to address the occurrence of the fistula in the laparotomy wound.
through 11) were directed toward cleansing and irrigation. To address drainage containment, negative pressure wound therapy (20 mm Hg) was administered on postoperative days 12 through 17 and throughout this period Mr. H required dressing changes every 2 to 3 hours, which disturbed his sleep. The periwound skin was irritated and painful. When he began oral intake of food, the drainage thickened and stool passed through the fistula, not the anus. Abdominal CT and colon study demonstrated the presence of a colocutaneous fistula within the laparotomy wound. Mr. H refused surgery to address the occurrence of the fistula in the laparotomy wound.
Management. On day 18, the fistula was treated using a silicone occlusion device made from a flexi-aid hand exerciser (see Figure 1) aided with AQUACEL® Ag (ConvaTec, Skillman, NJ). Scissors were used to cut the occluder portion of the silicone device as necessary to fit the fistula wound as wound size decreased. The device was cleansed using 75% alcohol while the dressing was changed.
The laparotomy wound and fistula improved; within 4 days, wound size decreased to 7.5 cm x 2.0 cm x 1.5 cm (see Figure 2). Mr. H was discharged on postoperative day 22. His wife handled his at-home care of the wound using the silicone device and hydrofiber dressing with silver. The fistula was healed on postoperative day 48 and the laparotomy wound was completely healed on postoperative day 64.
Discussion
Risk factors for postoperative fistula formation include inadequate blood supply to the anastomoses, tension on the suture line, distal obstruction, improper suturing technique, transverse position of the intestine with the anastomosis beneath a laparotomy wound, hematoma or abscess formation in the mesentery or anastomotic area, and malnutrition.4 Of the 152 patients who underwent esophageal reconstruction after corrosive injury at the authors’ facility, three had a 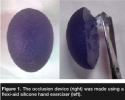 colocutaneous fistula in the laparotomy wound.1 The postoperative complications of these three patients were successfully treated by second surgery involving revision of the ileo-colostomy.
colocutaneous fistula in the laparotomy wound.1 The postoperative complications of these three patients were successfully treated by second surgery involving revision of the ileo-colostomy.
Fistula management can include large pouches that cover the entire wound, skin barriers to protect the surrounding skin, and the use of transparent dressings.4 A case series5 of five patients reported the use of negative pressure wound therapy (75 mm Hg) to manage patients with a fistula in an open abdominal wound. Covering the wound and fistula with pouches helps achieve and maintain wound hygiene by preventing drainage from contaminating the wound.4 The basis for management is the prevention of sepsis and fistula effluent management by open drainage, as well as nutritional support during the acute stage. Early surgery should be limited to abscess drainage and proximal defunctioning stoma formation. Definitive procedures for persistent enterocutaneous fistula should be performed several months later with resection of the fistulous segment and reanastomosis of the healthy bowel when feasible.5 Many techniques for surgical closure of fecal colocutaneous fistula have been reported.5-7
In the authors’ experience, nonsurgical therapeutic modalities usually are the first choice of patients. Streza et al8 has reported using silicone casting of abdominal wall defects around enteric fistulas to control fistula output and observed that it tends to prolong the presence of an open fistula when compared to other means of care.
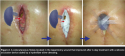 The silicone occlusion device from the flexi-aid hand exerciser is soft and easily made to fit the wound. The device prevents fecal soiling and facilitates normal passage of the stool to the distal colon. The silver dressing was used to promote growth of granulation tissue and abalation of necrotic tissue and exudate. This initial trial of this approach caused no discomfort. The silver dressing has been shown to improve the rate of granulation tissue formation while reducing the amount of necrotic tissue and exudate. The open abdominal wound shrinks, repaired by fibrotic tissues.9,10
The silicone occlusion device from the flexi-aid hand exerciser is soft and easily made to fit the wound. The device prevents fecal soiling and facilitates normal passage of the stool to the distal colon. The silver dressing was used to promote growth of granulation tissue and abalation of necrotic tissue and exudate. This initial trial of this approach caused no discomfort. The silver dressing has been shown to improve the rate of granulation tissue formation while reducing the amount of necrotic tissue and exudate. The open abdominal wound shrinks, repaired by fibrotic tissues.9,10
Conclusion
In this patient, a nonsurgical approach to fistula healing using an occlusion device used with a silver hydrofiber dressing provided a viable wound care option that prevented fecal soiling and facilitated easy closure of a colocutaneous fistula and laparotomy wound after previous management methods had failed. Continued research to optimize nonsurgical management of challenging wounds involving this device and other care methods is warranted.
Acknowledgment
The authors thank graphic designer Ms. Fang-Chun Kuo for her valuable support in providing the illustrations.
1. Wu MH, Tseng YL, Lin MY, Lai WW. Esophageal reconstruction for hypopharyngoesophageal strictures after corrosive injury. Euro J Cardiothorac Surg. 2001;19:400–405.
2. Tachi M, Hirabayashi S. Enterocutaneous fistula treated with a fasciocutaneous turnover flap. Ann Plast Surg. 2002;48:554–556.
3. Lynch AC, Delaney CP, Senagore AJ, Connor JT, Remzi FH, Fazio VW. Clinical outcome and factors predictive of recurrence after enterocutaneous fistula surgery. Ann Surg. 2004;240:825–831.
4. Reed T, Economon D, Wiersema-Bryant L. Colocutaneous fistula in a dehisced wound: a case study. Ostomy Wound Manage. 2006;52:60–64.
5. Goverman J, Yelon JA, Platz JJ, Singson RC, Turcinovic M. The “fistula VAC,” a technique for management of enterocutaneous fistulae arising within the open abdomen: report of 5 cases. J Trauma. 2006;60:428–431.
6. Kumar R, Naik S, Tiwari N, Sharma S, Varsheney S, Pruthi HS. Endoscopic closure of fecal colo-cutaneous fistula by using netal clips. Surg Laparosc Endosc Percutan Tech. 2007;17:447–451.
7. Weerd LD, Kjæve J, Aghajan E, Elvenes OP. The sandwich design: a new method to close a high-output enterocutaneous fistula and an associated abdominal wall defect. Ann Plast Surg. 2007;58:580–583.
8. Streza GA, Laing BJ, Gilsdorf RB. Management of enterocutaneous fistulas and problem stomas with silicone casting of the abdominal wall defect. Am J Surg. 1977;134:772–776.
9. Lansdown AB, Williams A, Chandler S, Benfield S. Silver absorption and antibacterial efficacy of silver dressings. J Wound Care. 2005;14:155–160.
10. Miller PR, Meredith JW, Johnson JC, Chang MC. Prospective evaluation of vacuum-assisted fascial closure after open abdomen planned ventral hernia rate is substantially reduced. Ann Surg. 2004;239(5):608–616.













