A Clinically Relevant Wound Assessment Method to Monitor Healing Progression
Accurate and clinically relevant wound assessment is an important if challenging aspect of wound management.1 Wound assessment terminology is not uniform and continues to inspire questions regarding wound assessment techniques. Clinicians do not all agree on the key wound parameters to measure in clinical practice and the accuracy and reliability of available wound assessment techniques vary.1
Wound healing progress currently is assessed dimensionally, visually, and physiologically.2 These methods involve the measurement of several parameters and review of subjective criteria, 2-5 usually specific to a wound type,2,3 and can be costly to the institution in terms of the time-intensive factors involved in obtaining, coordinating, and computing measurements and assessing wound characteristics.2 A review of the literature1 shows that several methods have been created to evaluate wound healing progress. These methods involve measuring the wounds by length and width, surface area, and/or volume. Each of these methods involves a scoring algorithm based on a series of criteria that may or may not include physiological observations such as presence of necrotic tissue, exudate type, epithelialization, and other pertinent factors. Regardless of method, monitoring wound progression is consistent with NPUAP guidelines.6
2-5 usually specific to a wound type,2,3 and can be costly to the institution in terms of the time-intensive factors involved in obtaining, coordinating, and computing measurements and assessing wound characteristics.2 A review of the literature1 shows that several methods have been created to evaluate wound healing progress. These methods involve measuring the wounds by length and width, surface area, and/or volume. Each of these methods involves a scoring algorithm based on a series of criteria that may or may not include physiological observations such as presence of necrotic tissue, exudate type, epithelialization, and other pertinent factors. Regardless of method, monitoring wound progression is consistent with NPUAP guidelines.6
Healing Assessment Tools
Pressure Sore Status Tool. In 1990, Bates-Jensen7 introduced the Pressure Sore Status Tool (PSST) to assess pressure ulcer healing. The tool consists of 13 scored parameters comprising two wound measurements (size and volume) and 11 observable wound conditions (ie, necrotic tissue type, exudate type, color of skin surrounding the wound, and the like). A score of 13 out of 65 points indicates regeneration. The validity and reliability of the PSST tool were established through a multicenter database review of more than 990 patients.4
Pressure Ulcer Scale for Healing. The Pressure Ulcer Scale for Healing (PUSH) was developed in 1997 by a task force of the National Pressure Ulcer Advisory Panel6 as a clinical tool to assist clinicians with routine evaluation of healing Stage II to Stage IV pressure ulcers. The PUSH tool evaluates three parameters consisting of two wound measurements (surface area – length x width – and depth) and tissue type. A score of 0 out of 16 is an indication of a completely healed wound. Content validity, prospective validity, and sensitivity to change were established in a research study of 37 subjects as reported by Thomas et al.8-10
Sessing Scale. In 1995, Ferrell et al11 developed the Sessing Scale in response to a request to standardize the procedures used for evaluating pressure ulcers. This assessment method was based on a seven-point series of interview parameters including descriptions of granulation tissue, infection, drainage, necrosis, and eschar developed by clinical wound specialists. Each parameter is assigned a value of 0 to 6, with 0 indicating normal skin at risk for a wound and 6 indicating breaks in skin with the presence of infection, drainage, necrosis, and possible sepsis. Scores are determined by calculating the change in numerical value of assessments over time. Positive scores indicate wound healing progression; negative scores indicate worsening of the wound. The test-retest reliability of the Sessing Scale has been ascertained.9
Wound Healing Scale. Krasner12 developed the Wound Healing Scale (WHS) in 1997 as an easy-to-use methods to assess healing in all types of wounds. The WHS was intended to provide an alternative to reverse wound staging. The WHS procedure comprises eight descriptive alphabetical modifiers for particular wound stages, which can be subjectively assigned individually or as a multiple alphabetical score.
Sussman Wound Healing Tool. In 1997, Sussman and Swanson13 developed the Sussman Wound Healing Tool (SWHT) as a diagnostic instrument to predict and track the impact of physical therapy on pressure wound healing over time. The SWHT is based on an acute wound healing model consisting of 10 categories describing the presence or absence of tissue attributes (eg, necrosis, maceration, hemorrhage) and 11 wound measurement characteristics (eg, depth, location, wound healing phase).
Wound depth. Several prospective studies14,15 have found wound depth to be a significant predictor of final healing and the time to healing. In addition, retrospective studies4 have shown that wound depth is related to healing characteristics and that change in depth is significantly associated with healing time. Reduction in wound area early in a patient’s course of treatment also has been shown to be a robust predictor of reaching final healing (100% closure).9,16 Thus, wound volume, which incorporates both wound area and wound depth, is a clinically useful measure that would allow a clinician to track the healing process of an individual wound.
Progression over time. An essential element in wound management is using measurement to assess wound progression over time. Measuring progress toward healing is fundamental to the management of wounds because it alerts the clinician to stalled healing and a need to adjust the care protocol. A method that is easily incorporated into clinical practice and allows the provider to assess progress of an individual wound over time has been lacking.3 The present measuring tools use calculated scores; at quick glance, the numbers presented must be interpreted per their designated scales. Wound area and depth are considered in some present measuring tools but not for use as a percent of healing measurement. The clinician gathers the wound information and must make it “fit” the parameters of the measurement tool, subjectively deciding, for example, whether exudate is moderate or heavy; plus, existing instruments may be considered information heavy. Key elements in developing an instrument include simplicity of use in a clinical setting and validity for measuring whether wounds are improving or worsening.9
The purpose of this case study is to describe the development and use of a clinical tool – the Barber Measuring Tool© – that can easily be added to current wound management practices in any institution. The tool uses variables collected in most clinical settings to examine an individual patient’s wound progression.
Patient Care Setting
The Carolina Specialty Hospital is a 40-bed, long-term acute care private hospital (LTACH) created for the patient who is too sick to go to a step-down facility or home. The facility is served by approximately 100 admitting and consulting physicians. Patients admitted to this LTACH have access to respiratory services, rehabilitation services (including physical therapy, occupational therapy, and speech therapy) and wound care – 96% of all patients admitted to this facility are wound care patients. The facility cares for approximately 198 to 215 wounds in any given month; the author has seen as many as 325 wounds in 1 month.
Tool Application
The Barber Measuring Tool© involves the calculation of wound volume using the initial wound measurements or more specifically, the greatest length, greatest width, and the depth of the wound upon admission. To find the greatest depth, a cotton-tipped applicator swab is placed into the wound’s deepest point. The applicator is marked at the skin level and then compared to a ruler.17 If undermining or tunneling is present, the measured amount of undermining tunneling is added to the depth measurement before being recorded on the Barber Measuring Tool© documentation instrument – originally a pen-and-paper tool that is now computerized software that calculates wound volumeand graphs wound progress in addition to storing patient information and providing a spreadsheet of information for the clinician. A simple formula is used to calculate the volume (volume = length x width x depth). This establishes the patient’s baseline volume and corresponds to 0% healing (see Figure 1).
A hard copy of the form is incorporated into the patient’s chart to make tracking part of the standard wound care. To track wound progression of the wound, weekly measurements are taken. Each set of weekly measurements then are used to determine current 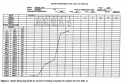 wound volume. The current wound volume is divided by the baseline wound volume and subtracted from 100% to compute the percent healed: 100% x (Current Volume)/(Volume Day 0). Thus, a line that moves up indicates that the wound is progressing to 100% healing or 100% closure (see Figure 2).
wound volume. The current wound volume is divided by the baseline wound volume and subtracted from 100% to compute the percent healed: 100% x (Current Volume)/(Volume Day 0). Thus, a line that moves up indicates that the wound is progressing to 100% healing or 100% closure (see Figure 2).
The software comes with a tutorial and directory to facilitate training. Basically, the clinician enters the wound measurements (length, width, and depth) and the software calculates volume and graphs the results, as well as stores the formulated information. To address regulatory guidance issues, there is also a section for notes that allows the clinician to document other factors (eg, exudate color, odor, condition of periwound tissue).
Results of Case Studies
The Barber Measuring Tool© has been used to track five different wound types (three different wound types are included in Table 1). The initial tracking form (see Figure 1) was constructed using a spreadsheet  software program capable of performing simple calculations to determine the wound volume range to percent of wound healing. For illustration purposes, wound assessments from a single patient seen in the author’s LTACH were used to demonstrate the usefulness of the method (see Figure 2). Weekly measurements were obtained and the volume calculated, at that point with a simple calculator. The wound healing results then were plotted by placing an x in the box containing the correct range and week number, providing an easy-to-read interpretable result on the rate of wound healing. Now, the software performs computation and graphing.
software program capable of performing simple calculations to determine the wound volume range to percent of wound healing. For illustration purposes, wound assessments from a single patient seen in the author’s LTACH were used to demonstrate the usefulness of the method (see Figure 2). Weekly measurements were obtained and the volume calculated, at that point with a simple calculator. The wound healing results then were plotted by placing an x in the box containing the correct range and week number, providing an easy-to-read interpretable result on the rate of wound healing. Now, the software performs computation and graphing.
To further illustrate the usefulness of this measuring tool over different wound types and 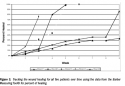 healing methods, the results from the five patients (see Table 1) were plotted on the instrument’s graph (see Figure 3). The results indicate that the Barber Measuring Tool© can show healing rates (percentage over time) across different wound types using different wound healing therapy options.
healing methods, the results from the five patients (see Table 1) were plotted on the instrument’s graph (see Figure 3). The results indicate that the Barber Measuring Tool© can show healing rates (percentage over time) across different wound types using different wound healing therapy options.
Discussion
One of the most important principles of wound management is periodic assessment of wound healing to document healing progress and assess the effectiveness of care. Terminology describing wound assessment is not standardized nor has consensus been reached on the most appropriate wound healing parameters to monitor,18 with the exception of wound area.19 In clinical practice, regular wound assessment using a consistent technique system is the only way to monitor healing outcomes.10 A number of measures of wound healing have been proposed and used in practice. However, none has been firmly established for either clinical or research purposes.
This graphical representation of wound healing directly on the instrument seems to be ideal for clinicians responsible for making treatment decisions. This method is individualized to the wound because wound volume upon admission serves as the baseline for all follow up measurements. The visual representation allows more immediate physician/clinician interpretation of wound progress than a score calculated from a standardized instrument. In practice, seeing a wound reach 98% healing by week 5 may be more meaningful than seeing a PUSH score move from 14 to 9.7. This simple evaluation allows clinicians to monitor the progression of the wound over time, which can lead to better decisions concerning current treatment options.
Although wounds can be shaped irregularly, wound shape is not reported to influence wound healing dynamics.17 Thus, using a simple measure of wound volume (length x width x depth) is consistent with clinical practice. Additionally, because volume is used as a means to calculate healing rate in terms of percent healed, the raw volume measures of different wounds are not compared. However, the percent healed (percent reduction from baseline) could be averaged across patients and compared between patient groups. As an institution, a goal may be to consider wound care treatments that may lead to faster healing; Table 1 includes description of five wounds to show how this may be done in practice.
Limitations
The Barber Measuring Tool has not been scientifically/statistically analyzed for reliability or validity. However, the author has used the tool to track the progress of more than 400 wounds, including surgical, burn, and chronic wounds (ie, pressure ulcers), and has found it to appropriately represent healing progression. The tool is based on a formula of volume: length x width x depth. As the measurements decrease, the volume of the wound base decreases and healing increases. As epithelialization occurs, the wound base becomes more shallow and area decreases. Calculating these measurements provides a percent of healing. However, the accuracy of the measurements must be considered. In addition, clinicians must remember wound size (ie, healing) does not take into account or address causes for non-healing (eg, comorbidities, patient age, nutrition) – only that the wound is or is not progressing – or consider the wound may appear to be healing despite other factors.
Conclusion
The proposed wound tracking method is straightforward and can be easily implemented into any practice. It is currently used for all patients in the author’s facility. This case series illustrates that the use of individual wound measurements such as the Barber Measuring Tool© may help clinicians monitor wound progress regardless of wound type or size. Such assessments provide an opportunity for clinical evaluation of wound care therapies and facilitate changes to the plan of care based on individual healing rates consistent with current NPUAP guidelines.
1. Keast DH, Bowering CK, Evans AW, Mackean GL, Burrows C, D’Souza L. MEASURE: A proposed assessment framework for developing best practice recommendations for wound assessment. Wound Repair Regen. 2004;12(3 Suppl):S1-S17.
2. Goldman RJ, Salcido R. More that one way to measure a wound: an overview of tools and techniques. Adv Skin Wound Care. 2002;15(5):236-243.
3. Gardner SE, Frantz RA, Bergquist S, Shin CD. A prospective study of the Pressure Ulcer Scale for Healing (PUSH). J Gerontol A Biol Sci Med Sci. 2005;60(1):93-97.
4. Bates-Jensen BM. The pressure sore status tool a few thousand assessments later. Adv Wound Care. 1997;10(5):65-73.
5. Kundin JI. A new way to size up a wound. Am J Nurs. 1989;89(2):206-207.
6. National Pressure Ulcer Advisory Panel. Available at: www.npuap.org. Accessed February 25, 2008.
7. Bates-Jensen BM. Indices to include wound healing assessment. Adv Wound Care. 1995;8(4):25-33.
8. Thomas DR, Rodeheaver GT, Bartolucci AA, Franz RA, Sussman C, Ferrell BA, Cuddigan J, Stotts NA, Maklebust J. Pressure ulcer scale for healing: derivation and validation of the PUSH Tool. The PUSH Task Force. Adv Wound Care. 1997;10(5):96-101.
9. Bates-Jensen BM. Quality indicators for prevention and management of pressure ulcers in vulnerable elders. Ann Intern Med. 2001;135(8 Pt 2):744-751.
10. Ratliff CR, Rodeheaver GT. Use of the PUSH tool to measure venous ulcer healing. Ostomy Wound Manage. 2005;51(5):58-63.
11. Ferrell BA, Artinian BM, Sessing D. The sessing scale for assessment of pressure ulcer healing. J Am Geriatr Soc. 1995;43(1):37-40.
12. Krasner D. Wound healing scale, version 1.0: a proposal. Adv Wound Care. 1997;10(5):82-85.
13. Sussman C, Swanson G. Utility of the Sussman Wound Healing Tool in predicting wound healing outcomes in physical therapy. Adv Wound Care. 1997;10(5):74-77.
14. Allman RM, Walker JM, Hart MK, Laprade CA, Noel LB, Smith CR. Air-fluidized beds or conventional therapy for pressure sores. A randomized trial. Ann Intern Med. 1987;107(5):641-648.
15. Sheehan P, Jones P, Caselli A, Giurini JM, Veves A. Percent change in wound area of diabetic foot ulcers over a 4-week period is a robust predictor of complete healing in a 12-week prospective trial. Diabetes Care. 2003;26(6):1879-1882.
16. Robson MC, Hill DP, Woodske ME, Steed DL. Wound healing trajectories as predictors of effectiveness of therapeutic agents. Arch Surg. 2000;135(7):773-777.
17. Doughty DB. Wound assessment: tips and techniques. Home Healthc Nurse. 2004;22(3):192-195.
18. Cukjati D, Rebersek S, Miklavcic D. A reliable method of determining wound healing rate. Med Biol Eng Comput. 2001;39(2):263-271.
19. Sheehan P. Early change in wound area as a predictor of healing in diabetic foot ulcers: knowing “when to say when”. Plast Reconstr Surg. 2006;117(7 suppl):245S-247S.














