Telemedicine in Patients With an Ostomy During the COVID-19 Pandemic: A Retrospective Observational Study
Abstract
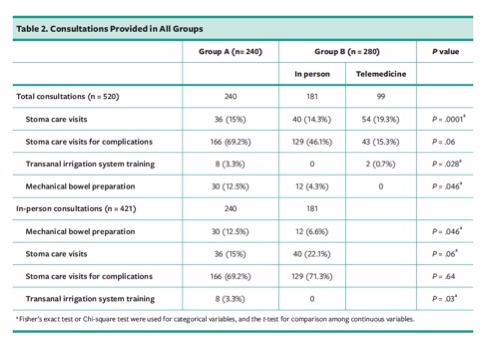
BACKGROUND: Italy instituted a lockdown from March 10 to May 3, 2020, due to the coronavirus disease-19 pandemic. All nonessential businesses were closed during this time, and health care services were reorganized. On March 11, the Stoma Care Center started providing telehealth services for patients with a stoma. PURPOSE: This retrospective observational study describes the experience of the Stoma Care Center of the University Hospital Federico II, Naples, Italy, before and during the lockdown. METHODS: Consultation records from January 1 through April 29 were retrieved, patient demographics and reasons for consultation abstracted, and pre-lockdown (January 1 to February 29) and lockdown (March 1 to April 29) information was compared. Patients who used telehealth services were also asked to rate their satisfaction with these services on a scale of 0 (extremely dissatisfied) to 4 (extremely satisfied). The authors analyzed all consultations provided from January to April 2020 and evaluated the use of telemedicine services for patients with an ostomy. Consultations were divided into 2 groups. Group A included consultations provided from January 1 to February 29. Group B included consultations provided from March 1 to April 29, which included the lockdown period. Group B included both in-person and telemedicine consultations. RESULTS: During the pre-lockdown period, 240 in-person consultations were provided. During the lockdown period, 181 in-person and 99 telemedicine consultations were provided. The number of in-person consultations for mechanical bowel preparation and transanal irrigation system training was lower (12.5% vs 6.6% [P = .046] and 3.3% vs 0% [P = .03]), whereas the number of consults for stoma care follow-up and stoma complications was higher (202 [84.1%] vs 266 [95%]). Of the 65 patients who completed the questionnaire, 82% indicated being extremely satisfied. CONCLUSIONS: The reorganization of stoma care services, including the availability of telemedicine, did not result in a decrease in the number of consultations provided. The results suggest that stoma care services using telemedicine may provide valid support for patients with an ostomy in the future.
Introduction
In December 2019, the Wuhan Municipal Health Commission, Hubei, China, reported the first cases of pneumonia of an unknown etiology.1 The responsible pathogen was identified as severe acute respiratory virus coronavirus 2 (SARS-CoV-2) and, on February 11, 2020, the World Health Organization named it coronavirus disease-19 (COVID-19).2,3 On March 11, 2020, the World Health Organization declared the COVID-19 pandemic.4 On June 4, more than 6 million cases had been confirmed in the world, with 382,867 deaths.5 Also on June 4 in Italy, a total of 234,013 cases had been reported; of these, 161,895 patients recovered, 33,689 died, and 38,429 had active infection.6 COVID-19 spread rapidly throughout the world, and the Italian government imposed extraordinary measures to restrict viral spread, including limitation of social activities (eg, the closures of schools, bars, restaurants, cinemas, museums, parks, and cemeteries). Although these restrictions were initially limited to Northern Italy, they were eventually extended to the rest of the country until, on March 10, a national lockdown was declared.
Lockdown is an emergency situation in which people are not allowed to move freely, and all nonessential businesses are closed.7 In Italy, the lockdown officially started on March 10, 2020, and ended on May 18, 2020; however, outpatient services were suspended on March 2 and restarted on May 4. In the Campania Region, which is where the hospital in the present study is located, the first 3 cases of COVID-19 were reported on February 27. As of June 4, 2020, the Campania Region had 4822 positive cases and 420 deaths.6
This situation demanded a rapid reorganization of health care systems, and surgical practices underwent several changes. The number of in-person outpatient visits was reduced and replaced with telemedicine when possible. Endoscopic procedures were limited to cases deemed urgent. Elective procedures were postponed or cancelled, limiting the activities mainly to emergency and oncological cases.8
During this period, the General Surgery Department of the University Hospital Federico II, Naples, Italy, continued to provide surgical care. Colorectal surgery was limited to oncological cases, complicated cases of inflammatory bowel disease (IBD), and emergencies. All these conditions often require the creation of an ostomy. Patient education about proper stoma care is intended to improve outcomes and enhance quality of life for patients with ostomy. Therefore, stoma care centers also needed to adapt their activities to ensure appropriate education and care during the pandemic. The aim of this study was to demonstrate how the Stoma Care Center at the University Hospital Federico II, Naples, Italy, responded before and during the COVID-19 lockdown and to emphasize the potential benefits of telemedicine as a tool for further enhancement of stoma care.9 The stoma care center is composed of 2 stoma therapists (nurses) and 3 surgeons who care for almost 20 outpatients weekly. The center has a catchment area of 800 patients and performs almost 1000 stoma-related procedures yearly. To evaluate and document the experience of the Stoma Care Center of the University Hospital Federico II, Naples, Italy, before and during the lockdown, a retrospective observational study was conducted.
Methods
All consultations provided by the stoma care center from January to April 2020 were reviewed and abstracted. Patient variables (age, sex, reason for consultation) and consultation methods were retrieved. Reason for consultations included mechanical bowel preparation, transanal irrigation system training for people with fecal incontinence and constipation (Peristeen; Coloplast, Minneapolis, MN), stoma care (first visit and follow-up), or stoma care complications. Consultations were grouped. Group A included all consultations provided from January 1 to February 29, 2020. Group B included those provided from March 1 to April 29, which corresponds to the Italian lockdown period.
Starting on March 11, telemedicine was offered to all patients, and 65 of 164 patients accepted with verbal informed consent. Telemedicine consultation was offered through WhatsApp and Skype apps because of the wide availability of these platforms among patients and the possibility of video consultations. Skype and WhatsApp were used due to the lack of secure telemedicine software, which was made available in the authors’ unit in June 2020.
To investigate patients’ satisfaction with telemedicine, a simple questionnaire was administered to patients via a telephone call 20 days after the consultation took place. Twenty (20) days was chosen because the staff had to adapt quickly to changing events, and it was preferred to gather data on patients’ experiences with telemedicine services in a short time (approximately 3 weeks). In this way, the authors hoped that quality of care with respect to telemedicine could be continuously improved. Patients were asked to score their experience with 5 points (0 = extremely dissatisfied, 1 = dissatisfied, 2 = neither satisfied nor dissatisfied, 3 = satisfied, and 4 = extremely satisfied).
Data analysis. All variables were entered in Excel.
Statistical analyses were performed with the Number Cruncher Statistical System (NCSS) 2020 data analysis version 20.0.1. Descriptive statistics were used to analyze patient satisfaction scores and patient demographics and reason for consultation were compared between Group A and B using Fisher’s exact test or Chi-square test for categorical variables and the t-test for comparison among continuous variables. A P value less than .05 was considered statistically significant.
The study was performed in accordance with the principles of the Declaration of Helsinki and its appendices. Approval was obtained from the Institutional Review Board and Ethics Committee of the University of Naples, Federico II.
Results
During the study period, 250 patients were managed, with 421 total in-person consultations at the Stoma Care Center. Starting on March 11, all patients requiring a consultation received a preliminary telephone call, and 65 of 164 patients accepted the telemedicine service. During Italy’s lockdown, 99 telemedicine consultations were performed. Table 1 shows demographic data for the participants. No statistical differences for patient age or sex were found between groups A and B. Group B includes both in-person visits and telemedicine consultations.
Telemedicine stoma care consultations involved patients’ and caregivers’ proper stoma management training, such as stoma positioning. Consultations for stoma care complications were related to stomal or parastomal skin alterations (dermatitis, erythema, ulcerations), hernias, or prolapses.
Prior to and after the lockdown (January 1, 2020 to February 29, 2020 and March 1, 2020 to April 29, 2020) a total of 520 consultations were performed. During both periods, the majority were stoma care visits for complications; 166 of 240 (69%) prior to the lockdown and 172 of 280 (61%) after lockdown (Table 2). Other reasons for in-person consultations included general stoma care visits (15% pre- and 22% post-lockdown), mechanical bowel preparation (30 [12.5%] in group A vs 12 [6.6%] in group B; P = .046) and transanal irrigation system training (8 in group A and zero in group B; P = .03). A total of 99 telemedicine consultations were performed. Of those, 54 (54.5%) were regular stoma care visits and 43 (43.4%) were for complications. Telemedicine represented 35.3% (99 of 280) of the consultations with 36.6% of patients (65 of 164). Adding consultations performed through telemedicine, there were significantly more consultations, especially for stoma care visits, during the 2 months after compared to the 2 months before the lockdown (P < .0001).
Of the participants who had telemedicine consultations (group B), 4 required in-person care and an additional 1 patient was admitted to the emergency unit for intestinal occlusion. Only 1 patient in group A required an emergency admittance due to intestinal occlusion.
The questionnaire was completed by 65 patients. Of those, 54 (83.2%) reported being extremely satisfied, 4 (6.1%) were satisfied, 2 (3.1%) were neither satisfied nor dissatisfied, 4 (6.1%) were dissatisfied, and 1 (1.5%) were extremely dissatisfied. A majority of patients (60, [92%]) stated that they would use telemedicine in the future.
Discussion
The COVID-19 pandemic has put a strain on patients, their families, and health care providers. The rapid spread of COVID-19 has created unprecedented challenges for medical and surgical health care systems.10 Hospitals not only have to care for patients with COVID-19, but also must guarantee optimal continuity of care.
Di Saverio et al11 stated that according to a nationwide analysis from China, 18 (1%) of 1590 patients with COVID-19 had a history of cancer; among these, 3 (16.7%) had a history of colorectal cancer. Patients with COVID-19 and previous or active cancers seemed to have more serious adverse events.11 According to data from the Italian National Institute of Health (Istituto Superiore di Sanità, ISS), out of a total of 2003 COVID-19–related deaths that occurred in Italy from March 10 to May 18, 2020, 72 patients (20.3%) had a history of active cancer in the past 5 years.10
The current study sought to explore changes that the COVID-19 pandemic has caused in a stoma care center in Italy. In our department, as well as in all Italian hospitals, surgical activity has been limited to emergency and oncological cases since March 11. From January to April 2020, the department performed 40 colorectal surgical procedures: 20 for colorectal (4 rectal cancer, 5 right colon, 7 left colon, 1 splenic flexure, 1 explorative laparoscopy for intestinal occlusion, and 2 synchronous colorectal cancers and subsequently cecostomy) and 20 for IBD (8 for ileocolic Crohn disease, 5 for perianal fistulizing Crohn disease, and 7 for ulcerative colitis). From these procedures, 18 new ostomies were created (8 for colorectal cancer and 10 for IBDs). The department continued to treat new patients: 20 patients from our department as well as patients from other departments (12 patients [7 from gynecology, 3 from oncology, and 2 from clinical medicine]) and other hospitals (8 patients). During this period, the stoma care center performed 280 consultations for 164 patients. There was a reduction of 32.6% of the total in-person visits when compared with the past 3 months, and 99 telemedicine consultations were performed.
During the COVID-19 pandemic, telemedicine represented 35.3% of the consultations with 36.6% of patients. These were preventive in an attempt to reduce nonurgent endoscopic procedures and mechanical bowel preparations. In addition, many patients preferred to adopt telemedicine to avoid leaving the house during the pandemic.
Because of the fragility of patients with an ostomy, the stoma care center remained functional by adopting safety protocols for both patients and hospital staff and offering telemedicine. Since 2006, the center has provided stomal rehabilitation, including mechanical bowel preparation, management and consultations for stomal rehabilitation, and transanal irrigation system training for people with bowel dysfunction.12 The team consists of 2 stoma therapist nurses and 3 surgeons. There is a dedicated outpatient clinic and services are provided in the hospital wards, rehabilitation outpatient clinic, and patients’ homes. Care encompasses preoperative, intraoperative, and early and late postoperative periods and continues until discharge. Fourteen (14) years ago, the center started with only 31 patients. The center has now seen 1454 patients in the past 2 years who mainly come from the health districts of the Campania region (96.6%), while 3.4% come from other regions.
Since the beginning of the lockdown in Italy, the measures adopted for limiting medical visits consisted of telephone triage, limited hours, and limited numbers of patients as well as identifying suitable routes in the building for in-person patient visits that reduce the amount of physical contact; these factors all increased the use of telemedicine services.8 Because stoma management should be considered a high-risk procedure in terms of infective transmission,12 telemedicine should be encouraged. In addition, there is evidence relating to patients with ostomy that telemedicine provides consistent benefits, such as a decrease in readmission rates and mobility-related costs as well as empowerment of the relationship between patients and health care professionals.13–16 Telemedicine often uses resources that are free and accessible to most patients of any age and level of education (eg, WhatsApp and Skype).
In the authors’ center, the stoma therapist nurse calls the patient the day before each visit to perform telephone triage.9 The questions asked concern respiratory symptoms (cough, fever, dyspnea), gastrointestinal symptoms, dysgeusia and anosmia, recent contacts with patients who tested positive for COVID-19, and any trips made to areas initially considered “red areas.” On the day of the visit triage is repeated, and body temperature is measured. While in the hospital building, patients must wear a face mask without exhalation valve and gloves. The patient passes through an independent entrance to reach the stoma therapy clinic. This route was created to help patients avoid contact with other patients because patients with a stoma often have several comorbidities. No relatives are permitted to accompany the patient. The stoma therapist nurse and the surgeons use different personal protective equipment for each patient. Appointment times are scheduled so that patients do not have to stop in the waiting room. Rooms are sanitized between all patients.9
Telemedicine services can be used in almost any medical specialty, but they are best suited for those with a consultation that requires a high visual component.12 Telemedicine has created an opportunity to offer patients such comprehensive and multidisciplinary care.17 There have been considerable advances in the implementation of telemedicine and the development of technology. Telemedicine applications have been applied in new areas, such as surgical telemonitoring, emergency medicine collaboration, education of medical personnel, multidisciplinary team meetings, and postoperative follow-up.17 Postoperative follow-up by telemedicine has the potential to improve care, and the technology has become user-friendly.12 showed that the use of telemedicine increases patient satisfaction and decreases the need for laboratory tests.18 Also in a randomized trial, Sun et al19 showed that a telehealth approach has a positive impact on the unique physical, psychological, social, and spiritual needs of cancer survivors living with a permanent ostomy.19 In a recent randomized clinical trial on telemedicine in postoperative follow-up of STOMa PAtients (the STOMPA trial), the authors showed that telemedicine did not affect quality of life but did reduce the readmission rate and burden of travel.16 Nevertheless, it has to be recognized that telemedicine has some limitations, including the absence of physical interactions or the presence of internet connection problems; however, in a time of crisis, these factors can be overcome.20
In the current study, telemedicine was offered to all patients with a stoma starting in March 2020. Not only did telemedicine reduce the flow of patients to the department, but it also provided an important service. Stoma care consultations increased in this period. Moreover, 83.2% of patients treated with telemedicine were extremely satisfied and 92% would use it in future.
The present study describes management approaches using telemedicine during the COVID-19 pandemic. To the best of the authors’ knowledge, there is only 1 case study in the literature about telemedicine management of postoperative complications in urostomy during the COVID-19 pandemic.21 Therefore, the current work could be the first retrospective study on the use of telemedicine in patients with an ostomy during the pandemic.
Limitations
Limitations of this study include it being retrospective, the administration of the satisfaction questionnaire by telephone, and having a homogeneous sample.
Conclusion
COVID-19 has led to rapid change in health care systems. The authors describe the experience of a stoma care center in Italy before and during a COVID-19–related lockdown. Following regional directives and department protocols to prevent the spread of infection (including the use of telehealth services) allowed for a continuity of care in patients with ostomy, and the number of stoma care visits and consultation for stoma complications increased in the month after compared to the month before the lockdown. The authors conclude that telemedicine proved to be an excellent method of evaluating patients with an ostomy and ensured continuity of care. Telemedicine could also be considered a valid support for patients with an ostomy in the future.
Affiliations
Dr. Dinuzzi, Dr. Palomba, and Dr. Amendola are surgeons, Endoscopic Surgery Unit, Department of Clinical Medicine and Surgery; Ms. Minischetti is head nurse, Endoscopic Surgery Unit, Department of Clinical Medicine and Surgery; Dr. P. Aprea is postgraduate assistant, Endoscopic Surgery Unit, Department of Clinical Medicine and Surgery; Dr. Luglio is assistant professor of surgery, Department of Clinical Medicine and Surgery; Dr. De Palma is full professor of surgery and head of the Endoscopic Surgery Unit, Department of Clinical Medicine and Surgery; Dr. G. Aprea is associate professor of surgery, Endoscopic Surgery Unit, Department of Clinical Medicine and Surgery, University of Naples, Federico II, Naples, Italy. VPD and GP contributed equally to this study and are both considered first authors. Address all correspondence to: Giuseppe Palomba, MD, Department of Clinical Medicine and Surgery, Federico II, University of Naples, Sergio Pansini 5- 80131 Naples, Italy; Tel: +39 081 7462710; fax: +39 081 7462710; email: giuseppepalomba3@virgilio.it.
References
1. Guerci C, Maffioli A, Bondurri AA, Ferrario L, Lazzarin F, Danelli P. COVID-19: how can a department of general surgery survive in a pandemic? Surgery. 2020;167(6):909–911. doi:10.1016/j.surg.2020.03.012
2. Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020; 76:71–76. doi:10.1016/j.ijsu.2020.02.034
3. World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it. World Health Organization. Accessed June 4, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it
4. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. World Health Organization. Accessed June, 4, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
5. World Health Organization. WHO coronavirus disease (COVID-19) pandemic. World Health Organization. Accessed June 4, 2020. https://covid19.who.int/
6. Dipartimento della Protezione Civile. COVID-19 situazione Italia. Protezione Civile. Accessed June 4, 2020. http://opendatadpc.maps.arcgis.com/apps/opsdashboard/index.html#/b0c68bce2cce478eaac82fe38d4138b1
7. Di Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;18(1):229. doi:10.1186/s12967-020-02399-5
8. Spinelli A, Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg. 2020;107(7):785–787. doi:10.1002/bjs.11627
9. Palomba G, Dinuzzi VP, De Palma GD, Aprea G. Management strategies and role of telemedicine in a surgery unit during COVID-19 outbreak. Int J Surg. 2020;79:189–190. doi:10.1016/j.ijsu.2020.05.081
10. Wexner SD, Cortés-Guiral D, Gilshtein H, Kent I, Reymond MA. COVID-19: impact on colorectal surgery. Colorectal Dis. 2020;22(6):635–640. doi:10.1111/codi.15112
11. Di Saverio S, Pata F, Gallo G, et al. Coronavirus pandemic and colorectal surgery: practical advice based on the Italian experience. Colorectal Dis. 2020;22(6):625–634. doi:10.1111/codi.15056
12. Dale M, Morgan H, Carter K, White J, Carolan-Rees G. Peristeen transanal irrigation system to manage bowel dysfunction: a NICE medical technology guidance. Appl Health Econ Health Policy. 2019;17(1):25–34. doi:10.1007/s40258-018-0447-x
13. Pata F, Bondurri A, Ferrara F, Parini D, Rizzo G; Multidisciplinary Italian Study group for STOmas (MISSTO). Enteral stoma care during COVID-19 pandemic: practical advice. Colorectal Dis. Published online: July 21, 2020. doi:10.1111/codi.15279
14. Cavaliere D, Parini D, Marano L, et al; SICO (Italian Society of Surgical Oncology). Surgical management of oncologic patient during and after the COVID-19 outbreak: practical recommendations from the Italian Society of Surgical Oncology. Updates Surg. 2020;12:1–9. doi:10.1007/s13304-020-00921-4
15. Minissian MB, Ballard-Hernandez J, Coleman B, et al. Multi-specialty nursing during COVID-19: lessons learned in Southern California. Nurse Lead. Published online September 7, 2020. doi:10.1016/j.mnl.2020.08.013
16. Augestad KM, Sneve AM, Lindsetmo RO. Telemedicine in postoperative follow-up of STOMa PAtients: a randomized clinical trial (the STOMPA trial). Br J Surg. 2020;107(5):509–518. doi:10.1002/bjs.11491
17. Müller KI, Alstadhaug KB, Bekkelund SI. A randomized trial of telemedicine efficacy and safety for nonacute headaches. Neurology. 2017;89(2):153–162. doi:10.1212/WNL.0000000000004085
18. Wallace P, Haines A, Harrison R, et al. Virtual Outreach Project Group. Joint teleconsultations (virtual outreach) versus standard outpatient appointments for patients referred by their general practitioner for a specialist opinion: a randomised trial. Lancet. 2002;359(9322):1961–1968. doi:10.1016/s0140-6736(02)08828-1
19. Sun V, Ercolano E, McCorkle R, et al. Ostomy telehealth for cancer survivors: design of the ostomy self-management training (OSMT) randomized trial. Contemp Clin Trials. 2018;64:167–172. doi:10.1016/j.cct.2017.10.008
20. Guarino M, Cossiga V, Fiorentino A, Pontillo G, Morisco F. Use of telemedicine for chronic liver disease at a single care center during the COVID-19 pandemic: prospective observational study. J Med Internet Res. 2020;22(9):e20874. doi:10.2196/20874
21. Sims TW, Wilson K. Telehealth management of urostomy postoperative complications. J Wound Ostomy Continence Nurs. 2020;47(5):456–457. doi:10.1097/WON.0000000000000698