A Proposal for Classifying Peristomal Skin Disorders: Results of a Multicenter Observational Study
How well ostomy patients adapt to their new life depends, to a great extent, on the preservation of peristomal skin integrity. The incidence of peristomal complications that can compromise that integrity cannot be easily determined; a review of literature indicates a complication incidence ranging from 18% to 55%.1
This extreme variability is related to significant differences in study populations and parameters assessed – eg, ostomy characteristics, time of lesion onset post surgery (early, 1 to 15 days, versus late, >15 days), types of complications, and types of diversions (eg, intestinal versus urinary). It appears evident that many patients undergoing urinary or intestinal diversions experience at least one type of complication after surgery. In the authors’ experience caring for nearly 700 patients per year over a mean period of 10 years, it is estimated that at least one third of colostomy patients and up to two thirds of urostomy and ileostomy patients are affected by at least one peristomal lesion. A published prospective audit of numerous stomas to assess risk factors associated with peristomal skin complications demonstrated the close correlation between retractions and obesity (P = 0.036), late skin excoriation and diabetes (P = 0.02), stoma in crease, and ostomies performed as emergency procedures (P = 0.022).2 
After consulting national and international professionals and conducting a careful review of the literature, it became clear that peristomal skin complications are one of the least studied postoperative complications. Skin disorders are generally recognized dermatologically and classified as “simple” inflammatory skin disorders related to mechanical, chemical, infectious, or allergic factors.3 In recent years, management/classification based on the stages of skin lesions borrowed from other fields was attempted.4,5 Currently, a classification system is used where complications are subdivided in terms of the timing of their occurrence. Early complications (occurring within 1 to 15 days after surgery) include edema, intra- and peristomal bleeding, ischemia or necrosis, retraction, detachment of mucocutaneous junction, suppuration and peristomal abscess, complications due to malposition, acute dermatitis, and skin lesions. Late complications (occurring more than 15 days after surgery) include hernia, prolapse, fistula, stenosis, granuloma, folliculitis, trauma, hemorrhage, and chronic dermatitis.6
In the authors’ opinions, this approach is not acceptable for the classification of peristomal complications. Ostomy care professionals need a peristomal skin lesion stage classification that is universally recognized and shared to facilitate lesion interpretation and detection that includes topography. This classification could be a standardized and objective tool useful for a proper monitoring and follow-up of complications. A study group – Studio osservazionale multicentrico sulle alterazioni cutanee post-enterostomie (Study on Peristomal Skin Disorders [SACS]) – comprised of seven Enterostomal Therapy (ET) nurses and four surgeons from eight facilities was created to: 1) study and classify skin disorders secondary to the creation of an enterostomy and, 2) determine, through the analysis of blood chemistry and clinical parameters, if a correlation exists between the severity of peristomal skin lesions and clinical metabolic disorders. This report shows results relevant to the first study objective – namely, the classification of peristomal skin disorders.
Materials and Methods
Time and setting. A prospective, observational study was conducted between December 2003 and February 2006. The eight national ostomy centers participating in this clinical study were located uniformly across Italy in order to prevent a possible geographic or environmental bias.
Patients. All enterostomy patients who accessed the participating clinics during the observation period were evaluated. The Ethics Committee of each participating hospital approved the study and all patients read and signed a written informed consent in compliance with privacy regulations.
Patients were assigned to one of two observational arms of the study according to the time elapsed since surgery (Group 1: <1 year; Group 2: >1 year) to differentiate between early and late skin lesions. Skin lesions were examined at set intervals (weeks 0, 4, 12, 24) and their changes noted over time by clinical observation and the acquisition of digital images. Blood chemistry was obtained as part of routine postoperative procedure because the results may be suggestive of tissue proliferation and regeneration factors. Laboratory values including blood glucose, iron, and hemoglobin levels, as well as patient weight and stoma variables such as burning, itching, pain, and bleeding, were recorded in the electronic data entry form provided to participating centers (see Figure 1).

Procedure. At the end of the 24-week observational period, study group members (the experts from the eight participating ostomy centers) attempted to validate the early/late classification system. During three consensus conferences, the expert panel developed and unanimously accepted the classification definitions based on their clinical observations and knowledge of the mechanisms of peristomal skin injury.
After the classification definitions were accepted, the first task was to examine and validate classification of the 800 digital images of injuries representative of all different typologies of injuries and topography that were contributed by the participating centers. After three additional consensus conferences, a common and shared criterion for the classification of the 800 images was achieved. Each component of the study group agreed on how the images were to be classified and that the classification system accurately classified the images. Subsequently, in order to enhance the reproducibility and objectivity of the classification, a multiple-choice questionnaire was sent via email to four experts outside the study group (two surgeons and two ET nurses) with experience in the field. They were asked to classify 20 images of injuries using the draft classification scheme accompanying the questionnaire. The results of the questionnaire were analyzed by a clinician coordinating responses.
Data analysis. Descriptive statistical analyses were conducted using the software SPSS 14.0 (SPSS, Chicago, Ill).
Results
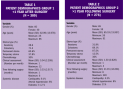
By the end of the study period, 656 ostomy patients had been observed: 380 in Group 1 – early complications – and 276 in Group 2 – late complications. Of all patients observed, 70% had colostomies; of these, 65% had undergone a Miles’ procedure.7 The remaining 30% of observed patients had ileostomies. Of all patients observed, 339 patients (52%, 272 men and 67 women) had peristomal skin disorders and were therefore included in the study for the development of the classification scheme. Group 1 comprised 194 patients (51%, average age 63, range 25 to 85) and group 2 included 145 patients (52%, average age 65, range 26 to 91). Of all patients observed in Group 1 and Group 2, 30% and 36.1%, respectively, were receiving adjuvant chemotherapy (see Table 1 and Table 2). The laboratory data collected are not part of this report but will be used for the analysis of the second endpoint in future report. After reviewing and classifying all the images, five lesions (L) were most commonly observed (see Figure 2).

The peristomal complication classification system developers agreed to identify the quadrants around the stoma in a manner similar to the system used for breast cancer patients to facilitate topographical description of the lesions (see Figure 2).
Using recurrent clinical manifestations (L) and topographical location (T), the most frequently observed lesion in both Groups was L1 (a hyperemic lesion) followed by L2 (an erosive lesion) (see Table 3 and Table 4). Classification as “intact” indicated the absence of lesions on peristomal skin.

The subsequent validation study results of the non-study group members validated the classification system. The validity of classification was measured by reporting agreement among diagnoses; strength of agreement was rated “very good” (K value = 0.91). Once it was ascertained that the classification system was a helpful tool, a pocket ruler guide for the classification was created to provide a brief summary and practical explanation on the classification system to be used by ET nurses in daily work.
As mentioned previously, the information obtained from the blood samples includes 10,848 bits of clinical and blood chemistry data and will be used by the SACS study group to investigate the possible correlation of blood test results with the severity of peristomal skin lesions. This study is ongoing.
Discussion
Although relevant literature was replete with descriptions of clinical pictures of irritative manifestations of the peristomal skin,9,10 an objective, clinical, easy-to-interpret classification of peristomal lesions was lacking. This is the first large-sample study to identify a simplistic, rapid way to document peristomal lesion change over time and provide an ability for healthcare personnel to compare and discuss lesion change. This classification instrument was not only developed but also validated to allow future use and study, as well as results, to be repeated by other clinicians. The parameters for classification (L and T) facilitate postsurgical assessment of lesions in a non-subjective, reproducible way. Incidentally, study data include a large sample of incidence and prevalence data of peristomal skin conditions. The study represents the first-time availability of a standardized classification system that is not based on individual opinion. Having a universal definition of peristomal complications offers clinicians a way to report and monitor complications – an important and effective tool for enterostomal therapists playing a pivotal role in the management of peristomal disorders.
Conclusions
Improving and maintaining the integrity of peristomal skin is an important objective for both ostomy patients and ostomy care professionals. Peristomal skin integrity plays a fundamental role in the improvement of quality of life of a patient with an abdominal ostomy. Having a way to classify peristomal skin disorders provides a tool for an objective assessment that, in turn, offers a new guideline for the correct interpretation and diagnosis of skin disorders. Additionally, the pocket ruler guide for peristomal skin disorder classification enhances the practicability of the guidelines.
The quality of professional service always must be supported by scientific research and professional ethics. An objective classification system is fundamental to proper diagnosis and characterization of peristomal skin disorders, standardization of terminology, and incidence or prevalence studies.
Furthermore, this classification scheme could be used to help identify mechanisms and biomarkers associated with the various classes of peristomal skin complications – topics for further research.
1. Colwell JC, Goldberg M, Carmel J. The state of the standard diversion. J WOCN. 2001;28(1):6-17.
2. Arumugam PJ, Bevan L, Macdonald L, et al. A prospective audit of stomas-analysis of risk factors and complications and their management. Colorectal Dis. 2003; 5(1):49-52.
3. Hampton B. Peristomal and stomal complications. In: Hampton B, Bryant R, eds. Ostomies and Continent Diversions: Nursing Management. St. Louis, Mo.: Mosby;1992:105-123.
4. Lyon CC, Beck MH. Dermatological problems in stoma patients. Br J Dermatol. 1999;140:536.
5. Rolstad BS, Erwin-Toth PL. Peristomal skin complications: prevention and management. Ostomy Wound Manage. 2004;50 (9):68-77.
6. Lyon CC, Smith AJ. Abdominal Stomas and Their Skin Disorders. An Atlas of Diagnosis and Management. London, UK. Martin Dunitz Ltd; 2001.
7. Miles WE. A method of performing abdominoperineal excision for carcinoma of the rectum and the terminal portion of the pelvic colon. Brit Med J. 1908;2:1812-1814.
8. Veronesi U, Saccozzi R, Del Vecchio M, et al. Comparing radical mastectomy with quadrantectomy, axillary dissection, and radiotherapy in patients with small cancers of the breast. N Engl J Med. 1981;305(1):6-11.
9. Turnbull G. Stomal complications: at what price? Ostomy Wound Manage. 2003;49(4):17-18.
10. Marquis P, Marrel A, Jambon B. Quality of life in patients with stomas: the Montreux study. Ostomy Wound Manage. 2003;49(2):48-55.













