Nutrition 411: Using Laboratory Data to Evaluate Nutritional Status
Optimizing a patient’s nutritional status is an integral part of modern medical care, particularly if the patient has a chronic wound. In order to determine the most appropriate medical nutrition therapy, a nutritional assessment is conducted to determine if the patient has any nutritional deficiencies or malnutrition. Typically, this determination is made, in part, by evaluating the patient’s biochemical or laboratory data. Healthcare professionals and registered dietitians (RDs) often rely on serum proteins such as albumin and prealbumin to identify a protein deficiency. As nutrition and medical science has evolved, the use of these markers has come into question. Many factors affect the levels of these serum proteins and their reliability as nutritional indicators may not be as high as once thought.
Between 23% and 85% of patients in long-term care facilities have protein energy undernutrition, making malnutrition one of the most serious problems facing nutrition and healthcare professionals working in that setting.1 The alarming nature of that statistic should prompt additional questions, including the criteria used to quantify and classify malnutrition. Before practitioners and RDs can begin to address malnutrition, it is critical to consider how it is diagnosed and how to measure improvement in patients.
Definition of Malnutrition
The American Dietetic Association’s (ADA) International Dietetics and Nutrition Terminology (IDNT) Reference Manual: Standardized Language for the Nutrition Care Process defines malnutrition as inadequate intake of protein and/or energy over prolonged periods of time resulting in loss of fat stores and/or muscle wasting.2 Malnutrition is categorized as uncomplicated or disease/trauma-related. Physical signs that differentiate these descriptions are listed in Table 1. 
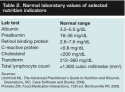
Common Biochemical Tests
When malnutrition is suspected, lab tests often are ordered. Historically, serum proteins — albumin, prealbumin (PAB), transferrin, and retinol-binding protein (RBP) — were used to measure malnutrition. C-reactive protein (CRP), total lymphocyte count (TLC), and serum total cholesterol are not serum proteins but sometimes are used as indicators of malnutrition. Normal ranges for these lab tests are listed in Table 2. Despite the standard use of lab tests to help diagnose malnutrition, experts have no consensus about which, if any, biochemical markers identify malnutrition, especially in the frail, elderly population.
Albumin frequently is ordered to assess protein stores and test results are found in virtually every patient’s medical record. Some medical professionals believe a low serum albumin level indicates a need for protein repletion. However, serum albumin (as well as other serum proteins) is a negative acute-phase reactant — ie, it decreases in the presence of inflammation, which occurs in situations that cause physical stress to the body, such as trauma, surgery, burns, or a chronic illness such as cancer, heart disease, or hepatic failure. This complicates the usefulness of serum proteins as indicators of malnutrition or protein status. In addition, albumin levels are sometimes inaccurate in cases of underhydration, overhydration, ascites, and nephrotic syndrome.3,4 Table 3 lists additional factors that affect the accuracy of albumin levels.
 Serum albumin increases as inflammation subsides, regardless of how much protein is consumed. Because of its relationship to inflammation, serum albumin is no longer considered a good indicator of malnutrition or protein repletion.3-5 Ordering a nutritional or protein supplement due to low albumin is no longer automatic because it is now believed that albumin levels do not reflect nutritional status or refeeding with much accuracy. However, a decreased serum albumin is considered an indicator of morbidity and mortality and persons with low albumin levels are sometimes at nutritional risk for other reasons.3-5
Serum albumin increases as inflammation subsides, regardless of how much protein is consumed. Because of its relationship to inflammation, serum albumin is no longer considered a good indicator of malnutrition or protein repletion.3-5 Ordering a nutritional or protein supplement due to low albumin is no longer automatic because it is now believed that albumin levels do not reflect nutritional status or refeeding with much accuracy. However, a decreased serum albumin is considered an indicator of morbidity and mortality and persons with low albumin levels are sometimes at nutritional risk for other reasons.3-5
PAB, also known as transthyretin, is affected by many of the same inflammatory conditions as albumin. PAB may be more valuable than albumin as an indicator; because it has a shorter half-life, PAB can respond more quickly to increases in nutrient intake or improvements in inflammation. While some experts maintain their belief that prealbumin is a useful indicator of malnutrition, many do not because of prealbumin’s relationship to inflammation.3-7 Table 4 lists additional factors that affect the accuracy of prealbumin levels.
Transferrin is used to evaluate protein and iron status. Inflammation leads to a decrease in transferrin; iron deficiency causes it to increase.3 In patients with iron deficiency, transferrin’s use is limited. Like other negative acute-phase reactants, many underlying factors affect serum transferrin levels, putting its sensitivity as an indicator of nutrition depletion and response to depletion in question.6
Some medical professionals consider RBP a sensitive indicator of changes in nutritional status.5,6,8 RBP in the blood is decreased in uncomplicated protein-calorie malnutrition. Although a negative acute-phase reactant protein, RBP seems relatively unaffected by inflammation.8 However, RBP is decreased in renal failure, hepatic failure, stress, and zinc or vitamin A deficiency6 and is not a reliable indicator of protein status in persons with advanced liver disorders because it is synthesized in the liver.
CRP is a nonspecific marker of inflammation. An elevated CRP reflects any type of inflammation. Decreases in CRP may help predict when inflammation is waning and when intensive nutrition therapy would help.5 In that respect, CRP may serve as a useful indirect marker of undernutrition.6
TLC and other immune deficiency markers may help predict malnutrition. Protein-energy malnutrition is associated with impaired immunocompetence. However, TLC decreases in the presence of stress, tumors, sepsis, and steroid usage, independent of malnutrition.7 Unfortunately, no single marker for immunocompetence, including total lymphocyte count, is effective for measuring malnutrition.5
Total cholesterol is associated with malnutrition and high mortality rates. In elderly patients, a total cholesterol <160 mg/ dL is considered a reflection of low lipoproteins and subsequently low visceral protein status.6 However, low serum cholesterol levels also may indicate severe liver disease or malabsorption syndromes.8
Putting It All Together
Although laboratory values taken singly or together may provide some clues to nutritional status, they probably do not provide sufficient information to identify malnutrition or evaluate the success of nutrition interventions. Not surprisingly, according to ADA,2 a diagnosis of malnutrition is based on tried-and-true physical assessment rather than biochemical tests. Potential indicators of malnutrition include anthropometric measurements, such as a body mass index (BMI) <18.5, failure to thrive, significant weight loss, physical signs of malnutrition, poor meal intake resulting in decreased intake of nutrients, or client history of medical or socioeconomic conditions that could lead to malnutrition.2
Rather than relying on lab results, healthcare professionals must use their assessment expertise and critical thinking skills to diagnose malnutrition and develop an effective nutrition intervention plan. Lab results can provide overall trends but are only one piece of the puzzle. Additional data from the medical record, evaluation of meal consumption, physical exam, and a visit with the patient all will provide information about nutritional status. Thorough follow-up includes evaluating changes in weight, BMI, appearance, and physical condition to determine if nutrition interventions are having their intended effect or if modifications are needed.
Acknowledgment
The authors gratefully acknowledge the research support for this article provided by Alexandra Briceno, senior dietetics and nutrition student at Florida International University, Miami, FL.
Nancy Collins, PhD, RD, LD/N, FAPWCA, is founder and executive director of RD411.com and Wounds411.com. For the past 20 years, she has served as a consultant to healthcare institutions and as a medico-legal expert to law firms involved in healthcare litigation. Liz Friedrich, MPH, RD, LDN, is a registered dietitian in Salisbury, NC, whose specialty is long-term care. Correspondence may be sent to Dr. Collins at NCtheRD@aol.com.
This article was not subject to the Ostomy Wound Management peer-review process.
1. Niedert KC. American Dietetic Association. Position of the American Dietetic Association: liberalization of the diet prescription improves quality of life for older adults in long-term care. J Am Diet Assoc. 2005;105:1955–1965.
2. American Dietetic Association. Pocket Guide for International Dietetics and Nutrition Terminology (IDNT) Reference Manual: Standardized Language for the Nutrition Care Process. 2nd ed. Chicago, IL: American Dietetic Association;2009.
3. Banh L. Serum proteins as markers of nutrition: what are we treating? Pract Gastroenterol (serial online). 2006;October:46–64. Available at: www.healthsystem.virginia.edu/internet/digestive-health/nutritionarticles/banharticle.pdf. Accessed February 20, 2010.
4. Fuhrman MP, Charney P, Mueller CM. Hepatic proteins and nutrition assessment. J Am Diet Assoc. 2004;104:1258–1264.
5. Mahan LK, Escott-Stump S. Krause’s Food and Nutrition Therapy. 12th ed. St Louis, MO: Saunders/Elsevier; 2008.
6. Omran ML, Morley JE. Assessment of protein energy malnutrition in older persons, Part II: laboratory evaluation. Nutrition. 2000;16:131–140.
7. Sergi G, Coin A, Enzi G, et al. Role of visceral proteins in detecting malnutrition in the elderly. Eur J Clin Nutr. 2006;60:203–209.
8. Litchford MD. The Advanced Practitioner’s Guide to Nutrition and Wounds. Greensboro, NC: Case Software and Publishing;2006.













