Nutrition 411: Obesity, Bariatric Surgery, and Wound Healing
Obesity rates are rising at an alarming rate and pose a major public health concern in the US and worldwide. The Centers for Disease Control and Prevention1 estimate that 34% of the American population is obese, numbers that have trended upward dramatically since 1980. Even more alarming is the increase in childhood obesity. Obesity in children 2 through 19 years of age has steadily grown; currently, more than 17% of American children are obese.2
Obesity is defined by body mass index (BMI) ≥30, calculated by dividing weight in kilograms by height in meters squared. Morbid obesity is defined as having a BMI ≥40. Obesity is a refractory and multifactorial disease associated with many comorbid conditions that affect all organ systems (see Table 1). If comorbid conditions associated with obesity are taken into account, obesity contributes to an estimated 300,000 deaths per year.3 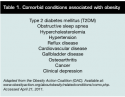
Conventional forms of obesity treatment include a combination of diet therapy, physical activity, pharmacotherapy, and behavior modification; the surgical approach (ie, bariatric surgery) is considered an effective long-term treatment.4 Because bariatric surgery successfully resolves certain comorbid conditions such as diabetes, hypertension, and obstructive sleep apnea, bariatric surgery is recognized as a metabolic surgery.5
Nutritional Concerns With Bariatric Surgery
Bariatric surgical techniques have evolved since the first surgical procedure (the jejunoileal bypass [JI]) was performed in the mid-1950s. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK),6 the most common bariatric procedure performed in the US is the Roux-en-Y gastric bypass (RNYGBP), followed by the adjustable gastric band (AGB), vertical sleeve gastrectomy (VSG), and the biliopancreatic diversion with duodenal switch (BPD/DS). All bariatric procedures restrict stomach capacity, so the patient is unable to eat large portions of food, leading to weight loss because of reduced caloric intake. Some surgical procedures are also malabsorptive, so calorie and nutrient absorption is reduced, which also facilitates the weight loss process.
Thus, bariatric surgery poses challenges and opportunities for nutrition and healthcare professionals. The type of bariatric procedure has a bearing on the type of nutritional side effects or potential deficiencies that may develop. Currently, no single, standardized bariatric diet is available, and many recommendations are based on experiential data with limited evidence-based research. Most dietary recommendations for postbariatric surgical patients are supported by evidence for similar gastrointestinal surgeries or recommendations for very low-calorie diets (VLCD). However, the American Society for Metabolic and Bariatric Surgery (ASMBS)7 recently published specific guidelines for the perioperative and postoperative care of the bariatric patient. In addition, the American Association of Clinical Endocrinologists, the Obesity Society, and the ASMBS have published a joint clinical practice guideline.8
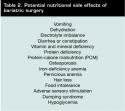 Bariatric surgery is considered a safe procedure for the long-term resolution of obesity; however, nutrition deficiencies, dumping syndrome (ie, gastric emptying where undigested stomach contents are “dumped” too rapidly into the small intestine), and food intolerances have been reported, especially in patients who do not follow guidelines.9 Potential nutritional side effects after bariatric surgery, which may be exacerbated by surgical type, are listed in Table 2.
Bariatric surgery is considered a safe procedure for the long-term resolution of obesity; however, nutrition deficiencies, dumping syndrome (ie, gastric emptying where undigested stomach contents are “dumped” too rapidly into the small intestine), and food intolerances have been reported, especially in patients who do not follow guidelines.9 Potential nutritional side effects after bariatric surgery, which may be exacerbated by surgical type, are listed in Table 2.
General nutrition recommendations for bariatric surgery focus on eating pattern, mechanics of eating and drinking, food tolerance, diet progression, adequate intake of fluids and macronutrients (especially high-quality protein), and daily adherence to vitamin and mineral intake recommendations. Table 3 lists general bariatric nutrition recommendations; however, healthcare providers should consider individual, patient-focused nutrition counseling based on the type of surgical procedure, presence of nutrition complication, socioeconomic and psychosocial factors, level of education, and patient readiness for the lifestyle changes associated with this surgery. Table 4 lists recommended vitamin and mineral intake based on surgical procedure.
In addition, it has been shown that patient outcomes in safety, weight loss, and dietary compliance are enhanced when a multidisciplinary team approach to care is implemented.10
Wound Healing in the Bariatric Surgical Patient
Most bariatric surgery is laparoscopic, but some patients may require “open” surgery or a laparotomy. These patients will have a larger incision that may take longer to heal. Infections can occur up to 3 weeks after surgery and patients must be educated on how to care for the surgical wounds and monitor for signs of infection or wound dehiscence. A recent study11 that examined the information received by patients undergoing bariatric surgery found that study participants received very little information about incision care. Lack of information about incision care was associated with greater fear of having the surgery. A questionnaire included as part of the study revealed patients are most concerned about pain, complications, and activity — issues that could easily be addressed with proper education and instruction. The Midwest Bariatric Institute at Saint Margaret Mercy Hospital in Indiana12 posts wound care instructions on its website as part of the educational process. This one-page document explains what to expect and how to change the wound dressings, shower with the incision, and monitor for any complications.
According to Virji and Murr,13 wound infection and incisional hernias are seen less in laparoscopic surgical procedures than in conventional surgeries. McGlinch et al14 have found that wound infection is seen in <3% of the population with laparoscopic bariatric surgery; however, in open bariatric surgery, as high as 20% of patients may present with wound infection with symptoms of pain, fever, erythema, and purulence around the surgical site. Obese patients have a higher risk of skin wound infection because of the presence of large subcutaneous spaces with poor blood supply. A large percentage of patients undergoing bariatric surgery also presents with several comorbid conditions such as diabetes mellitus, which increases risk of poor wound healing. Wound infections may present several weeks postsurgery and may lead to weakened surgical incision sites. Wound infections pose a challenge and are associated with increased morbidity because of prolonged healing time and increased risk of incisional hernias.
In addition to nursing and medical management of wounds, which includes drainage and broad-spectrum antibiotic therapy, increased protein and calories, 15 mg of zinc, 3,000 mcg biotin, and 250 to 500 mg of vitamin C may be recommended (see Table 4). For malabsorptive bariatric procedures, oral intake of modular proteins that contain all indispensable amino acids may be recommended. A protein intake of 1.5 to 2.0 g/kg of body weight may be appropriate to reduce the risk of hypoalbuminemia.
Chronic wounds. Some bariatric surgical patients may have chronic wounds such as nonhealing pressure ulcers. This may be a result of the greater adiposity, making it difficult to reposition, and multiple skin folds. Although evidence is scant with regard to bariatric surgical patients with chronic wounds, the most important macronutrient for both populations is protein. Protein is the sole macronutrient to provide nitrogen, which is essential to life. The patient with reduced stomach capacity should be instructed to consume the protein component of the meal first.
Because of compromised absorption of macro- and micronutrients, patients who have undergone gastric bypass or BPD/BS present the extra challenge of balancing weight loss with calorie and protein intake appropriate to facilitate chronic wound healing. The addition of L-arginine and L-glutamine may be useful in the wound healing process, although empirical evidence of efficacy and dosage of these products used in the bariatric population is limited. Medical nutrition therapy of bariatric patients with acute or chronic wounds requires individual detailed assessment of oral intake and tolerance. Correcting malnutrition by administering appropriate calories and adding nutraceuticals, modular proteins, separate amino acids, and extra vitamins and minerals are best recommended after careful assessment of lab work and interdisciplinary collaboration with the medical and nursing team.
Practice Points
Healthcare professionals should understand that bariatric patients have an altered anatomy that mandates specific nutrition requirements. Nutrition assessment should include collecting anthropometric and biochemical data along with a full assessment of dietary intake, eating patterns, adherence to diet regimen, current challenges, and any wounds that may be present before or after surgery. The patient’s physical activity progress and psychosocial support system also should be monitored. Bariatric patients should understand the surgery provides only a tool to help facilitate weight loss. The nutrition professional can assist the patient with dietary and lifestyle changes for life-long healthy success of obesity remission.
Coming next month: Best Practices for Nutrition
Nancy Collins, PhD, RD, LD/N, FAPWCA, is founder and executive director of RD411.com and Wounds411.com. For the past 20 years, she has served as a consultant to healthcare institutions and as a medico-legal expert to law firms involved in healthcare litigation. Lillian Craggs-Dino, MS, RD, LD/N, CLT, is a Bariatric Dietitian and Support Group Coordinator for the Bariatric and Metabolic Institute at Cleveland Clinic Florida. Correspondence may be sent to Dr. Collins at NCtheRD@aol.com. This article was not subject to the Ostomy Wound Management peer-review process.
1. CDC defining overweight and obesity. Available at: www.cdc.gov/obesity/defining.html. Accessed April 22, 2011.
2. CDC childhood overweight and obesity. Available at: www.cdc.gov/obesity/childhood/index.html. Accessed April 22, 2011.
3. Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;20;293(15):1861–1867.
4. Buchwald H. Consensus conference statement: bariatric surgery for morbid obesity: health implications for patients, health professionals, and third party payers. Surg Obesity Rel Dis. 2005;1:371–381.
5. American Society for Metabolic and Bariatric Surgery. Metabolic surgery expected to play a bigger role in treating type 2 diabetes and other metabolic diseases. Available at: www.asbs.org/Newsite07/resources/press_release_8202007.pdf. Accessed April 23, 2011.
6. Bariatric Surgery for Severe Obesity. Available at: http://win.niddk.nih.gov/publications/gastric.htm. Accessed May 18, 2011.
7. ASMBS Allied Health Nutritional Guidelines for the Surgical Weight Loss Patient. Available at: www.asmbs.org/Newsite07/resources/bgs_final.pdf. Accessed April 23, 2011.
8. American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic and Bariatric Surgery. Medical Guidelines for Clinical Practice for the Perioperative Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery Patient. Available at: www.asmbs.org/Newsite07/resources/aace-tos-asmbs.pdf. Accessed April 22, 2011.
9. McKee JS, Tassinari, S. Nutrition in bariatric surgery: the role of nursing in reducing liability. J Legal Nurs Consult. 2006;17:7–11.
10. Blackburn GL. The 2008 Edward E. Mason founders lecture: Interdisciplinary teams in the development of best practice obesity surgery. Surg Obesity Rel Dis. 2008;4:679–684.
11. Pieper B, Sieggreen M, Nordstrom C, Kulwicki P, Freeland B, Palleschi MT, et al. Bariatric Surgery: Patient Incision Care and Discharge Concerns. Available at: www.o-wm.com/article/5837?page=0,6. Accessed May 13, 2011.
12. Midwest Bariatric Institute, Saint Margaret Mercy Hospital. Wound care after gastric bypass surgery. Available at: http://smmhc.adam.com/content.aspx?productId=67&pid=67&gid=000047. Accessed May 13, 2011.
13. Virji A, Murr MM. Caring for patients after bariatric surgery. Am Fam Phys. 2006;73(8):1403–1408.
14. McGlinch BP, Que FG, Nelson JL, Wrobleski DM, Grant JE, Collazo-Clavell ML. Perioperative care of patients undergoing bariatric surgery. Mayo Clin Proc. 2006;81(10 suppl):S25–S33.













