Managing Severe Dermatitis Caused by Ileal Peristomal Leakage Using a Mushroom-type (de Pezzer) Catheter in Infants: A Case Series
Abstract
Skin damage secondary to peristomal leakage is a fairly common complication of ileostomies in infants. Traditional conservative measures, including skin barriers, ointments, and agents to reduce bowel movements, initially may be helpful but not in all patients. The purpose of this case series was to describe a new and relatively simple procedure to temporarily manage severe peristomal dermatitis caused by ileal peristomal leakage in infants.
After obtaining informed consent from the parents, a mushroom-type (de Pezzer) catheter was inserted into the ileostomy of 11 1- to 4-month-old infants (seven males, four females) with severe peristomal dermatitis. Eight had total aganglionic colon (TAC), two had meconium ileus (cystic fibrosis), and one had meconium peritonitis due to bowel perforation proximal to ileal atresia. The severity of the peristomal dermatitis improved remarkably in all patients after 2 to 3 days. In eight patients, minimal (if any) dermatitis was noted within 5 to 7 days after tube insertion. Six patients who initially had poor weight gain (mean 345 g/month) developed acceptable weight gain (mean 648 g/month) (P <0.03) within 2 to 4 months. In seven patients with TAC, the tube was maintained for 2 to 4 months until definitive pull-through procedure; in four other patients, the tube remained in place for 3 to 7 days as a step for preoperative build-up. None of the patients developed any complications. The procedure requires the presence of a pediatric or trained surgeon, and care must be taken to prevent iatrogenic damage. In this case series, an appropriate-size, mushroom-type (de Pezzer) catheter placed within the ileostomy was a practical mode for temporary control of ileal peristomal leakage that causes severe peristomal dermatitis in infants, particularly in those not responding to medical therapy. Larger studies are needed to develop evidence-based protocols of care for the prevention and management of ileostoma complications in infants.
Potential Conflicts of Interest: none disclosed
Introduction
Ileostomy surgery in infants is a life-saving procedure in many situations, including Hirschsprung’s disease with total aganglionic colon (TAC) (dysmotile spastic colon due to congenital absence of ganglion cells in the rectum and colon), complex meconium ileus (cystic fibrosis), necrotizing enterocolitis, gastroschisis with ileal atresia, and in the presence of meconium or fecal peritonitis due to ileal perforation.1 Despite its vital advantages in the latter situations, an ileostomy in this population is associated with a variety of management problems1; chemical, mechanical, and allergic dermatitis or skin excoriation around the stoma are the most frequent among its different complications.2-6 Although some patients may respond temporarily to ordinary conservative treatment, such as application of skin barriers and low-potency topical steroids in mild to moderate peristomal dermatitis for few days and administration of agents to reduce bowel movements, further aggressive management might be needed in other situations, particularly those requiring ileostomy for several months, such as TAC.
The main function of the colon is to conserve fluid and sodium.7 In ileostomy patients, such colonic function is lacking. Subsequently, owing to loose and high-output content of the ileostomy containing proteolytic enzymes, patients are prone not only to dehydration and hyponatremia, but also to irritant dermatitis.6,8 Various dermatological problems occur in children and some adults. Other than chemical injury, this situation also may be due to mechanical destruction, infections, immunological reactions, or disease-related conditions.3 According to Ratliff and Donovan’s prospective descriptive study,9 the frequency of peristomal complications is highest among patients with ileal conduits and ileostomies. Approximately one third of the patients in Robertson et al’s case series10 and 57% in Herlufsen et al’s series11 had compromised skin around the ileostomy, 77% of which could be related to contact with stoma effluent. In the Jemec and Nybaek series,12 more than one in three visits to ostomy nurses were due to peristomal skin problems. Prospective, descriptive studies6,13 have shown many patients (79%) with ileostomy, regardless of age and underlying cause of stoma, will develop mild to moderate dermatitis. Furthermore, retrospective studies14,15 have indicated severe episodes of peri-ileostomy dermatitis occur in 5% to 25% of patients.
 Regardless of its extent and patient age or size, peristomal dermatitis is managed mainly using a combination of skin barriers, different ointments, and most importantly, a pouching system (ie, a well-fitted ileostomy device) to prevent direct contact between the irritant bowel contents and the peristomal skin. However, in the authors’ experience, pouching systems for ileostomy in infants, in contrast to adults, are less efficient for fecal diversion. In other words, because of poor or partial appliance adherence in children, especially infants, ileal peristomal leakage occurs, and as expected the chance of problems around the ileostomy is higher as compared to adults. For the same reason, some infants may develop dermatitis extending to the unprotected ipsilateral groin (see Figure 1).
Regardless of its extent and patient age or size, peristomal dermatitis is managed mainly using a combination of skin barriers, different ointments, and most importantly, a pouching system (ie, a well-fitted ileostomy device) to prevent direct contact between the irritant bowel contents and the peristomal skin. However, in the authors’ experience, pouching systems for ileostomy in infants, in contrast to adults, are less efficient for fecal diversion. In other words, because of poor or partial appliance adherence in children, especially infants, ileal peristomal leakage occurs, and as expected the chance of problems around the ileostomy is higher as compared to adults. For the same reason, some infants may develop dermatitis extending to the unprotected ipsilateral groin (see Figure 1).
Furthermore, there is always a chance of superimposed fungal infection or candidiasis accompanying severe peristomal dermatitis or excoriation of skin at any age (including infants), aggravating the problem.1,2,4,6,9,16 In addition, because of the physiologic cotransport phenomenon of sodium glucose, in the presence of hyponatremia, glucose cannot be absorbed normally. As a result, glucose concentration of the bowel content will increase, which subsequently gives rise to more frequent small bowel movements or osmotic diarrhea.8 The latter problem cannot be overcome unless the low serum sodium concentration is corrected. Therefore, for a variety of reasons, these patients usually have frequent small bowel movements associated with poor feeding. Consequently, the patients are not only irritable and restless, but they also may develop dehydration, acid base imbalances, hyponatremia, and poor weight gain if not properly managed.
Despite the availability of different kinds of appliances, pouching systems, and skin barriers, stoma-related skin lesions are not uncommon.1,2,5,16 Moreover, management of severe dermatitis around an ileostomy, especially when it is not responding to conservative therapy, remains a challenge. The purpose of this case series is to describe a new and relatively simple procedure to temporarily manage severe peristomal dermatitis caused by ileal peristomal leakage in infants. 
Catheter Insertion Technique
An appropriately sized, mushroom-type (de Pezzer) catheter is selected, usually No. 22 or 24 for early infancy (up to 6 months of life). For better drainage, the nipple of the catheter is partially cut and, if necessary, its side holes are enlarged. The infant is sedated (the authors use hydroxyzine syrup 0.5 mL/kg 10 minutes before the procedure) in the operating theater or alternatively in the emergency room. Before insertion of the catheter by the pediatric or trained surgeon, the direction of the ileum for a few centimeters proximal to the stoma must be determined by a smooth-curved clamp to prevent iatrogenic bowel perforation. The widest part of the catheter then is folded on its longitudinal axis and clamped. The tube, while stretched to reduce its tip diameter, is held by the third to fifth fingers (usually the right hand). Once inserted for 3 to 4 cm, the tube is released and then de-clamped. To prevent catheter removal during withdrawal of the clamp, the catheter is held with a smooth forceps (in the left hand) introduced through the stoma. Owing to the self-holding nature of the catheter, suturing is not necessary. To prevent the chance of bowel obstruction, the tube (40 cm in length) is shortened to 12 to 15 cm to reduce resistance to outflow of bowel contents, after which it is connected either to an ostomy bag or a cost-effective ordinary plastic bag. Antifungal- and zinc oxide-containing ointment also is applied three to four times per day for another 5 to 6 days along with Vaseline® (EX-DOPAR, Sina Darou Lab Co, Iran) or vitamin A ointment twice daily for at least 1 week. To prevent detachment of the ileostomy, the catheter should not be inserted earlier than 3 weeks after construction of the ileostomy.
Other Interventions
As part of post-ileostomy medical management, to compensate for sodium loss and prevent metabolic acidosis, sodium bicarbonate (2 to 2.5 meq/kg/day in three to four divided doses) mixed with milk is given to all patients, regardless of peristomal condition, until the time of ileostomy closure. If necessary, a short course (5 to 7 days) of parasympatholytic agent (such as dicyclomine and, less frequently, belladona) for reduction of bowel movement (>2/hour) also is administered. An infant ileostomy bag is not used in any patient because of availability problems, cost, or lack of appropriate size and secure fit. 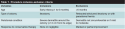
Methods
Patients. From April 2003 through March 2012, outpatient infants (1 to 6 months old) with an ileostomy who exhibited signs of severe dermatitis unresponsive to conservative therapy were considered for the procedure. Complete inclusion/exclusion criteria are detailed in Table 1.
Procedure. A mushroom-type (de Pezzer) catheter was inserted by the senior author into the ileostomy (with dermatitis around) and care procedures described instituted.
The peristomal skin was photographed every 2 to 3 days during the first 10 days until alleviation or substantial improvement of the dermatitis (dry pink skin in the absence of gross inflammation). Monthly body weights were recorded for comparison of before and after the tube insertion weight. Serum sodium and potassium concentrations also were measured at the time of referral before the tube insertion, corrected if needed, and checked once more 3 to 4 weeks after the procedure. Measurement of ileostomy fluid loss was not performed quantitatively. However, patients’ parents were asked to report estimated frequency of small bowel movements (ie, defecations via ileostomy) during 24 hours for 2 to 3 days both before and after catheter insertion.
The procedure was approved by the ethics committee of Shiraz University of Medical Sciences. Before the procedure, parents were informed of its benefits and potential problems, after which written parental consent was obtained.
Data collection and analysis. Wilcoxon signed-ranks test was used for statistical analysis of the weight gain. A P value <0.05 was considered statistically significant. Descriptive statistics of extent and severity of dermatitis was performed by gross appearance (inspection) of skin before and after catheter insertion. 
Results
Eleven 1- to 4-month-old infants (seven males, four females) with an end or loop ileostomy and severe dermatitis (ie, circumferential, ≥1.5 cm from the edge of the stoma, inflamed, wet, and deeply red skin) underwent the procedure (see Table 2). Five patients had dermatitis extending up to near the ipsilateral groin (see Figure 1a). Ileostomy had been performed for the following reasons: TAC (eight patients, six distal ileostomy and two mid-ileostomy), complex meconium ileus (two, due to cystic fibrosis), and meconium peritonitis due to bowel perforation proximal to ileal atresia (one patient) (see Table 2).  The severity of the peristomal dermatitis improved in all patients 2 to 3 days after the catheter was inserted. In eight patients, minimal if any dermatitis (ie, the skin appeared dry, non-inflamed, with almost normal skin color at the periphery of the stoma) was noted 5 to 7 days after insertion of the catheter (see Figures 1b, 2b, 3b). In addition, patients who had dermatitis near the ipsilateral groin showed marked improvement similar to healing of the peristomal skin lesion (see Figure 1). No relation was found between the initial extent of dermatitis and duration of time necessary for notable response to the procedure. There also was marked reduction in the number of defecations via ileostomy after tube insertion from 55 to 70 times/day before to 15 to 25 times/day following the procedure. Six patients with TAC who had poor weight gain (mean 345 [± 41] g/month, range 300 to 420 g/month) gained a significant amount of weight (mean 648 [± 57] g/month, range 600–750 g/month) thereafter (P <0.03).
The severity of the peristomal dermatitis improved in all patients 2 to 3 days after the catheter was inserted. In eight patients, minimal if any dermatitis (ie, the skin appeared dry, non-inflamed, with almost normal skin color at the periphery of the stoma) was noted 5 to 7 days after insertion of the catheter (see Figures 1b, 2b, 3b). In addition, patients who had dermatitis near the ipsilateral groin showed marked improvement similar to healing of the peristomal skin lesion (see Figure 1). No relation was found between the initial extent of dermatitis and duration of time necessary for notable response to the procedure. There also was marked reduction in the number of defecations via ileostomy after tube insertion from 55 to 70 times/day before to 15 to 25 times/day following the procedure. Six patients with TAC who had poor weight gain (mean 345 [± 41] g/month, range 300 to 420 g/month) gained a significant amount of weight (mean 648 [± 57] g/month, range 600–750 g/month) thereafter (P <0.03).  Although the potassium concentration was within normal range in all patients, hyponatremia (Na+ <130 meq/L) was detected in three patients with TAC despite daily sodium bicarbonate (2–2.5 meq/kg) administration. However, once corrected, hyponatremia did not recur while receiving the same sodium bicarbonate dose until the time of closure of the ileostomy. Major complications, such as bowel erosion or detachment of the ileostomy, did not occur in any patients. In two restless patients with TAC, the tube was extruded two times (1 to 2 weeks after insertion) without evidence of obstruction. Reinsertion was performed with a larger size catheter and no additional extrusions occurred. To prevent recurrence of the dermatitis, in seven patients with TAC who were not yet ready for a pull-through operation, the catheters were maintained for 2 to 4 months until the time of definitive procedure, usually at the age of 4 to 6 months. In five of the latter group, the tubes were renewed every 4 to 6 weeks because of partial tube decay. The tubes in four other patients were in place for only 3 to 7 days as a step for preoperative build-up (see Table 2). Final procedures included a Martin/Duhamel pull-through or a total colectomy and partial proctectomy followed by ileomidrectal anastomosis with or without posterior anorectal myectomy. None of the patients developed wound infection at the site of ileostomy following its closure.
Although the potassium concentration was within normal range in all patients, hyponatremia (Na+ <130 meq/L) was detected in three patients with TAC despite daily sodium bicarbonate (2–2.5 meq/kg) administration. However, once corrected, hyponatremia did not recur while receiving the same sodium bicarbonate dose until the time of closure of the ileostomy. Major complications, such as bowel erosion or detachment of the ileostomy, did not occur in any patients. In two restless patients with TAC, the tube was extruded two times (1 to 2 weeks after insertion) without evidence of obstruction. Reinsertion was performed with a larger size catheter and no additional extrusions occurred. To prevent recurrence of the dermatitis, in seven patients with TAC who were not yet ready for a pull-through operation, the catheters were maintained for 2 to 4 months until the time of definitive procedure, usually at the age of 4 to 6 months. In five of the latter group, the tubes were renewed every 4 to 6 weeks because of partial tube decay. The tubes in four other patients were in place for only 3 to 7 days as a step for preoperative build-up (see Table 2). Final procedures included a Martin/Duhamel pull-through or a total colectomy and partial proctectomy followed by ileomidrectal anastomosis with or without posterior anorectal myectomy. None of the patients developed wound infection at the site of ileostomy following its closure.
Discussion
In general, three different categories of complications may occur after ileostomy: anatomical (eg, prolapse, parastomal hernia, stenosis, retraction), physiological (eg, dehydration, hyponatremia), and dermatitis or skin excoriation around the stoma, which is the most common.6,9-12 Dermatologic problems are far more similar among children and adults than the other two types of complications; as such, dermatologic-related information on ileostomy is not specific to infants/children. However, for a variety of reasons, such as irritant alkaline content of the ileal discharge,3,6 frequency of small bowel movements, texture of skin, and lack of snug fit of the ostomy device, dermatitis around the ileostomy is more common in infants than adults.
Severe peristomal dermatitis at any age may be accompanied by superimposed fungal infection, which in turn aggravates the problem.1,2,4,6,9,16 The main goal of the relatively simple procedure described in this study is to guide management of severe peristomal dermatitis in infants that has been shown to be unyielding to other modes of conservative therapy by preventing further direct contact of irritant small bowel contents to the skin around the ileostomy (see Figures 1b, 2b, 3b). In the authors’ experience, tube insertion into the ileostomy in the presence of severe dermatitis is highly effective, especially when infant pouching systems are not available or too costly. Regardless of the initial extent of severe dermatitis, the majority of the authors’ patients had remarkable improvement in a short period of time and almost complete healing occurred in approximately 1 week. In addition, some of the untoward side effects of the ileostomy, such as frequent defecations via ileostomy or poor weight gain, also improved.
Selecting an appropriate catheter size is crucial to achieving these goals. The mushroom-type (de Pezzer) catheter (original length = 40 cm) should not be too long to cause bowel obstruction, nor should it be too narrow to cause leakage around the tube or facilitate extrusion. In the authors’ experience, an appropriate tube length (approximately 12 to 15 cm) and size (usually No. 22 or 24 in early infancy) produces adequate resistance to outflow of the bowel contents without obstruction or significant leakage around the tube.
Although the number of small bowel movements before and after catheter insertion was estimated by the parents, the noted difference was substantial (55 to 70 per day versus 15 to 25 per day) and may be the result of partial stasis or slow transit time. Subsequently, there would be longer time for bowel contents to be absorbed. In other words, the outflow resistance created by the catheter causes delayed emptying and, at least to some extent, would lead to increased absorption and acceptable weight gain. However, the latter also may be partly related to healed dermatitis obviating irritability, restlessness, and to some extent, catabolic state. Therefore, a combination of factors — ie, the healing process and reduced loss of fluid and electrolytes presumably associated with improved absorption — may support an anabolic state and explain the statistically significant increase in weight gain (P <0.03). Although this procedure was performed in infants with positive response, owing to the loose and watery nature of ileal contents, it also might be useful in older children and even adults.
The need for daily replacement of sodium bicarbonate in infants with an ostomy (particularly an ileostomy) cannot be overemphasized. Patients with an ileostomy require 6 to 10 mmol/kg (equivalent to 6 to 10 meq/kg) of sodium per day.8 With ordinary feeds, infants receive 2 to 4 mmol/kg of sodium per day.8 Thus, the sodium deficit may be estimated at 4 to 6 mmol/kg. To prevent this complication, sodium bicarbonate 4 to 6 meq/kg/day, as suggested by Sacher et al,8 should be given daily in divided doses until the ileostomy is closed. Although the maintenance dose (2 to 2.5 meq/kg/day) of sodium given to the authors’ patients was about half of the recommended dose suggested by Sacher et al,8 none of their patients developed hyponatremia after its correction and ileostomy tube insertion. This also may have been due to outflow resistance created by the tube providing longer time for ileal contents, including sodium, to be absorbed.
Limitations
An important limitation of the procedure is that, due to potential complications such as iatrogenic bowel perforation, catheter insertion should be performed by an expert or trained surgeon. To prevent detachment of the ileal stoma, the procedure should not be performed earlier than 3 weeks after construction of the ileostomy. In the presence of failure to thrive or poor weight gain, because of poor wound healing, the surgeon should be very cautious during tube insertion. The results reported here only describe a small sample of patients; more extensive research to help standardize care is needed.
Conclusion
In this case series, inserting an appropriate-size, mushroom-type (de Pezzer) catheter inside the ileostomy as a temporary measure for fecal diversion and control of ileal peristomal leakage in infants was found to be a practical method to manage severe peristomal dermatitis. Following the procedure, the dermatitis resolved. In addition, weight gain and hyponatremia were observed to improve in patients not responding to conservative therapy. This procedure may be considered for infants with ileostomies and skin problems, especially in settings where an alternative pouching system is not readily available. Further studies on the safety, effectiveness, and efficacy of this method are warranted.
Acknowledgment
The authors are most grateful to Dr. Hassanzadeh for his statistical analysis.
Dr. SA Banani is a Professor of Pediatric Surgery and Academic Member, Shiraz University of Medical Sciences (SUMS), Department of Pediatric Surgery, Shiraz, Iran. Dr. SJ Banani is a General Practitioner and Clinical Research Assistant at University of British Columbia, Vancouver, BC, Canada. Please address correspondence to: Seyed Javad Banani, MD, 2306-918 Cooperage Way, Vancouver, BC, Canada V6B 0A7; email: sjavadbanani@alumni.ubc.ca.
1. Gauderer MWL. Stomas of the small and large intestine. In: Coran AG (ed). Pediatric Surgery, 7th ed. Philadelphia, PA: Elsevier; 2012:1235–1245.
2. Burch J. Caring for peristomal skin: what every nurse should know. Br J Nurs. 2010;19(3):166–170.
3. Nybaek H, Jemec GB. Skin problems in stoma patients. J Eur Acad Dermatol Venereol. 2010;24(3):249–257.
4. Ratliff CR. Early peristomal skin complications reported by WOC nurses. J Wound Ostomy Continence Nurs. 2010;37(5):505–510.
5. Burch J. Peristomal skin care and the use of accessories to promote skin health. Br J Nurs. 2011;20(7 suppl):S4–S8.
6. Hellman J, Lago CP. Dermatologic complications in colostomy and ileostomy patients. Int J Dermatol. 1990;29(2):129–133.
7. Sandle GI. Salt and water absorption in the human colon: a modern appraisal. Gut. 1998;43(2):294–299.
8. Sacher P, Hirsig J, Gresser J, Spitz L. The importance of oral sodium replacement in ileostomy patients. Prog Pediatr Surg. 1989;24:226–231.
9. Ratliff CR, Donovan AM. Frequency of peristomal complications. Ostomy Wound Manage. 2001;47(8):26–29.
10. Robertson I, Leung E, Hughes D, Spiers M, Donnelly L, Mackenzie I, et al. Prospective analysis of stoma-related complications. Colorectal Dis. 2005;7(3):279–285.
11. Herlufsen P, Oslen AG, Carlsen B, Nybaek H, Karlsmark T, Laursen TN, et al. Study of peristomal skin disorders in patients with permanent stomas. Br J Nurs. 2006;15(16):854–862.
12. Jemec GB, Nybaek H. Peristomal skin problems account for more than one in three visits to ostomy nurses. Br J Dermatol. 2008;159(5):1211–1212.
13. Moon CM, Meffert JJ. Periostomy dermatitis: a novel therapeutic approach. Skinmed. 2002;1(1):60–61.
14. Shellito PC. Complications of abdominal stomal surgery. Dis Colon Rectum. 1998;1(12):1562–1572.
15. Husain SG, Cataldo TE. Late stomal complications. Clin Colon Rectal Surg. 2008;21(1):31–40. 16. Burch J, Sica J. Common peristomal skin problems and potential treatment options. Br J Nurs. 2008;17(17):S4–S8.













