The Effect of Pycnogenol on Wound Healing in Diabetic Rats
Abstract
Pycnogenol (PYC), an extract of pine bark, is known to have photoprotective, antimicrobial, antioxidant, and anti-inflammatory properties. An in vivo study was conducted to evaluate the effects of PYC treatment on wound healing in 48 adult male Sprague-Dawley rats, of which 24 were injected with a single dose of alloxan to induce diabetes.Three (3) excisional skin wounds (1.3 cm x 1.3 cm x 2 mm) were created in each healthy and diabetic animal. One (1) wound in each animal was left untreated, 1 was treated daily with a cleanser (ethacridine lactate) and covered with silver sulfadiazine (SSD), and 1 was treated with PYC powder (30 mg). After measuring wound size, 6 animals from both groups were sacrificed on days 3, 7, 14, and 21 and tissue samples were taken for histopathological evaluation of acute and chronic inflammation, granulation tissue, fibroblast maturation, collagen deposition, epithelialization, and neovascularization using a scoring system of 0 = none, 1 = mild, 2 = moderate, and 3 = abundant. Because the wounds created were not uniform in size within and among the animals, healing was expressed as a percentage of the initial wound size for each animal. Data were compared using 2-way analysis of variance; histopathological lesion scores were reported in median values in univariate analysis, with P <.05 denoting statistical significance. The mean initial wound surface area was 1.69 ± 0.44 cm2. On day 21, the average reduction in wound size was lower in diabetic than in healthy rats (47.42% versus 50.91%, P <.0001) and, in both groups combined, the average reduction was 45.73% in untreated, 48.73% in cleanser/SSD-treated, and 58.03% in PYC-treated wounds (P <.0001). Wound size reduction was also significantly different between PYC and the cleanser/SSD treatment depending on the rats’ health status (P <.0001): 49.68% and 47.84% using cleanser/SSD and 56.17% and 49.84% using PYC in healthy and diabetic rats, respectively. After 3 weeks, wound size for the healthy rats had decreased more than in the diabetic rats (mean 50.91% versus 47.42%). Although reepithelialization was complete in both groups by day 21, complete neovascularization was evident in the healthy rats but not in the diabetic rats. Overall, compared to the untreated control wounds, treatments with cleanser/SSD and PYC were equally effective in lowering acute and chronic inflammation scores on days 7 and 21. In diabetic rat wounds, collagen deposition and neovascularization scores were higher in wounds treated with PYC than cleanser/SSD-treated wounds (1.5 versus 1.0 and 2.0 versus 1.5, respectively). PYC appears to be a viable option to accelerate wound healing. Further in vivo and human research is warranted.
Introduction
Wound healing is a complex process that includes clotting, inflammation, granulation tissue formation, epithelialization, collagen synthesis, and tissue remodeling.1 According to an in vivo murine study,2 diabetes mellitus is associated with a variety of connective tissue abnormalities. Inhibition of the inflammatory response, angiogenesis, fibroplasia, and defects in collagen, as well as differentiation of the extracellular matrix, interfere with the wound healing process in diabetes.2,3
In several experimental studies,4-6 the therapeutic efficacies of many plants have been reported in ethno- and modern medicine. Pycnogenol® (PYC, the trademarked name of the extract of the French maritime pine tree) contains proanthocyanidins (antioxidants); it has been shown in experimental and in vitro studies to exert photoprotective, antimicrobial, antioxidant,7 anti-inflammatory,8 and anticarcinogenic9 effects. Proanthocyanidins have a high affinity to collagen and elastin and inhibit enzymatic hydrolysis via matrix metalloproteinases in vitro.10In vivo studies8,11,12 have shown these beneficial effects can aid the wound healing process.
Antiseptic agents are used in the treatment of some open wounds to kill or suppress microorganisms.13 Ethacridine lactate (EL), a commercially available antiseptic agent, is reported to stimulate release of an anti-inflammatory cytokine (ie, interleukin-10) during angiogenesis and formation of granulation tissue in vitro.14 Silver compounds are also antiseptic agents used in open wounds; in solution form, antiseptics often are used to irrigate or cleanse wounds.15-17 Ointments containing silver sulfadiazine (SSD) have been shown in murine, porcine,18 and rat model studies19 to improve the wound healing process by enhancing epithelialization. However, when used for an extended period of time, antiseptics increase the likelihood of tissue toxicity and delayed healing.15
Diabetes mellitus is associated with oxidative stress that slows the wound healing process.20,21 It was hypothesized that utilization of PYC would accelerate the wound healing process in the diabetic condition. The purpose of this in vivo experiment was to evaluate the effect of PYC on experimentally created excision wounds on the skin of healthy and diabetic rats in comparison with a cleanser containing EL and SSD ointment.
Methods
This experimental protocol was approved by the Ethics Committee for Animal Experimentation (#2013/63), Faculty of Veterinary Medicine, Atatürk University, Erzurum, Turkey. Adult male Sprague-Dawley rats (N = 48) weighing 350–400 g were fed pelleted feed and water ad libitum and housed at controlled ambient temperature (22.0˚ ± 1.0˚ C) under a 12-hour light/12-hour dark schedule. The rats were divided equally into 2 main groups: healthy and diabetic (induced).
Before the diabetes induction, the rats (n = 24) were fasted for 12 hours and then injected with a single dose of alloxan monohydrate (120 mg/kg body weight within 0.9% saline, intraperitoneal) (Sigma-Aldrich, St. Louis, MO). Three (3) days after alloxan injection, rats with a glucose level >250 mg/dL were considered diabetic.22
All animals were anesthetized using xylazine HCl and ketamine HCl before wounding. The rats were placed in the prone position, the hair on the dorsal side was shaved, and the skin was cleaned with 70% ethanol. Three (3) excision wounds were created on the midline by cutting out a 1.3 cm x 1.3 cm x 2 mm (length x width x depth) piece of skin.
Each of these 3 wounds in the healthy and diabetic rats was either untreated, treated topically with cleanser consisting of 0.1% EL (Rivanol, Şifa Kimya, Konya, Turkey) followed by SSD ointment (Silverdin 1%, Deva, İstanbul, Turkey), or treated with PYC powder (Pycnogenol®, 30 mg, Solgar Vitamin and Herb, Leonia, NJ). The wounds were covered with gauze (sterile gauze compress, PAK, Istanbul, Turkey) and adhesive tape (Cansın Plast, Kocaeli, Turkey). The wounds were treated once daily until the day of sacrifice.
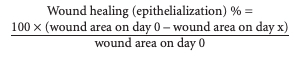
Wound area was measured on days 3, 7, 14, and 21 using a transparent paper and a permanent marker.23 Relative wound healing was reflected in reduction in wound size resulting from epithelialization and calculated using the following formula24:
On days 3, 7, 14, and 21, 6 rats in each group (healthy and diabetic) were euthanized under anesthesia. Their skin wound samples were removed and fixed in 10% buffered neutral formalin solution for 72 hours. Tissue samples were embedded in paraffin after xylene and ascendant ethanol series. The paraffin blocks were cut to 5-µm thickness using a Leica RM2125RT microtome and stained with Mallory’s triple stain.25 The stained specimens were examined under a light microscope. Photographic images were taken for scoring acute inflammation, chronic inflammation, granulation tissue, fibroblast maturation, collagen deposition, epithelialization, and neovascularization in 10 randomly selected areas using an approximately 4X objective lens; scores then were averaged. The scores were determined by a histologist blinded to the treatment groups as 0 = none, 1 = mild, 2 = moderate, and 3 = abundant, as described by Abramov et al.26
Data collection and analyses. Two-way analysis of variance (ANOVA) was used to test the effect of health status (healthy versus diabetic) and treatment (untreated versus cleanser versus PYC) as well as their interaction. The model also assessed the effect of time to elucidate alterations in response variables. The histopathological lesion scores were reported in median values in univariate analysis using SPSS version 16.0, (SPSS Inc, Chicago, IL). A P value <.05 was considered significant.
Results
Wound size. The wounds were not created equal in size within and among animals. The initial mean wound surface area was 1.69 ± 0.44 cm2. As time progressed, wound size decreased, with the largest decrease observed within the first week in all wounds regardless of the rat’s health status. The mean percent reduction in wound size relative to initial wound area was 16.17% ± 0.21% (range 15.75%–16.60%), 38.60% ± 0.25% (range 38.11%–39.09%), 60.78% ± 0.30% (range 60.18%–61.38%), and 81.14% ± 0.43% (range 80.30%–81.98%) on days 3, 7, 14, and 21, respectively. Overall, within 3 weeks wound healing in diabetic rats was slower than in healthy rats, as reflected by lower reduction in wound size relative to the initial size (47.42% versus 50.91%, P <.0001) (see Table 1). In both groups combined, after 21 days, the average reduction was 45.73% in untreated wounds compared to 48.73% for wounds treated with the cleanser/SSD and 58.03% for wounds in the PYC group (P <.0001). The superior results achieved when using PYC versus the cleanser/SSD application were reflected by the wound size reduction in both healthy (56.17% versus 49.68%) and diabetic (49.84% versus 47.84%) rats, respectively (P <.0001).
Wound macroscopy.
Healthy rats. On day 3, mild erythema was noted on the wound edges in untreated rats and rats treated with cleanser/SSD (see Figure 1A). On day 7, it was observed that: 1) a thin new tissue layer had formed at the base of the wounded areas in untreated healthy rats, 2) a rash surrounded the wound that developed scar tissue that covered approximately 50% of the wounds treated with cleanser/SSD, and 3) a scar formed over the entire wound in healthy rats receiving PYC (see Figure 1A). Wound contraction was noted on day 14, the most in the PYC-treated wounds, followed by cleanser/SSD-treated and untreated wounds (see Figure 1A).
Diabetic rats. On day 3, wounds in untreated rats and diabetic rats in the cleanser/SSD group exhibited a lack of wound contraction and the formation of scar tissue (see Figure 1B). However, wound contraction with a mild erythema on the edges and a thin layer forming at the base of the wounds was noted in diabetic rat wounds treated with PYC (see Figure 1B). On day 7, a scar developed that covered half of the wound in untreated and diabetic rats that received PYC. Mild wound contraction in all diabetic rats and a greatly reduced erythema in PYC-treated wounds of diabetic rats also was noted (see Figure 1B). On day 14, none of the wounds in diabetic rats showed erythema; on day 21, mild contraction of the wounds was noted (see Figure 2B).
Histopathology.
Quantitative microscopy. Overall, acute inflammation, chronic inflammation, collagen deposition, and reepithelialization scores for wounds in healthy and diabetic rats were similar. Fibroblast maturation (2.00 versus 1.00) and neovascularization (2.00 versus 1.00) scores for wounds in healthy rats were statistically higher than those for diabetic rats (see Table 2; P <.0001). Acute inflammation scores were higher on day 3 in diabetic rats than healthy rats (3.00 versus 2.00); it diminished on day 14 in all wounds of both healthy and diabetic rats. Signs of chronic inflammation were not evident on day 21 in either healthy or diabetic rats. Despite no noticeable differences on day 3 in both groups, collagen deposition increased more in healthy rats than diabetic rats by the end of the study (3.00 versus 2.00). Granulation tissue was still present in the diabetic rats (median score of 2.00), but not in the healthy rats at the end of the experiment. Fibroblast maturation (median score of 1.00) and neovascularization (median score of 2.00) were evident on day 3 in healthy rats and on day 7 in diabetic rats, with a median score of 1 for both parameters. Reepithelialization was absent until day 14 in all rats. However, fibroblast maturation and reepithelialization were completed in both groups by the end of the experiment with median score of 3.00. Complete neovascularization was evident in healthy rats but not in diabetic rats on day 21 (3.00 versus 2.00) (see Figure 2A for healthy rats and 2B for diabetic rats).
Overall, compared to the untreated control wounds, treatments with cleanser/SSD and PYC were equally effective in altering histopathology indices in both diabetic and healthy animals (see Table 2). Both treatments resulted in lower scores for acute and chronic inflammation on days 7 and 21, respectively.
Health status by treatment interaction showed that both cleanser/SSD and PYC applications improved wound healing process, more notable in healthy rats than in diabetic rats (see Table 2).
Discussion
In this study, diabetes was induced to compare the efficicacy of PYC and EL plus SSD in the wound healing process.27 The wound was created in the diabetes model because hyperglycemia was reported to interfere with tissue regeneration, probably due to increased oxidative stress in diabetic subjects.20,21 EL solution, an aromatic organic compound, is primarily used as an antiseptic for wounds.28 A pilot study using a pig model29 investigating the effects of silver-containing dressings on infected resection wounds reported use of SSD led to early wound granulation compared with hydrocolloid wound dressing treatment; histologically, fewer inflammatory cells and increased reepithelialization were noted.
Various natural substances have been widely used for wound healing since ancient times.30 Among such substances, polyphenol compounds are known to be strong antioxidants.31 PYC, primarily composed of procyanidins and phenolic acids, has been used worldwide as a herbal remedy for wound healing.32 Clinical studies have shown it accelerates wound healing processes11,33 owing to its anti-inflammatory and wound healing effects.8,11 In this study, macroscopically, the reduction in wound size resulting from reepithelialization was considered a clinical healing parameter; overall average wound size decreased approximately 50% within 21 days (see Table 1). Neither healthy nor diabetic rats achieved 100% skin coverage in the wounded area; the average was 81% on day 21. Regardless of health status, wounds managed with PYC exhibited a greater percent reduction in wound size compared to the cleanser/SSD and untreated control wounds, but it failed to exert more positive effects in diabetic rats. According to the study by Jeong et al,12 wound size decreased from day 1 to day 7 and wound area decreased significantly in the PYC-treated group on day 7. Similar to the results of the current study, Latif et al34 reported topical application of PYC to skin excision wounds in diabetic and healthy rats increased the rate of wound repair.
Wound contraction is considered an important factor in evaluating healing in large open wounds.35 In this study, in both healthy and diabetic animals, a significant difference was noted in the contraction rate of wounds treated with PYC compared to those treated with the cleanser and SSD. According to Jeong et al,12 wound contraction and collagen deposit time were higher in the PYC-treated group than the untreated control group on day 7. Jeong et al12 also stated epithelial cell movement is observed at day 5 in the PYC group. In the current study, histopathology parameters partially explain the reductions in wound area observed. A high acute inflammation score following wounding could indicate successful wound induction, and having no chronic inflammation by the end of the study could suggest 3 weeks is a sufficient follow-up period to determine remission. Clinically, estimating scar condition 21 days after skin damage may be limited in its significance. However, it must be considered that the wound healing process in animals such as rats is accelerated and consequently days ahead of human wounds at the same points in time.36
During this study, increased collagen deposition, formation of granulation tissue, fibroblast maturation, reepithelialization, and neovascularization scores in response to treatment were evident for wound healing, which was slower in diabetic rats than in healthy rats, suggesting interference of oxidative stress at cellular and tissue levels due to metabolic stress. However, the differences in wound healing rates between PYC and the cleanser/SSD treatment were not statistically significant in diabetic rats. In their clinical study, Grimm et al36 reported PYC promotes inflammatory responses in healthy subjects. In the current study, inflammation was still present on day 21 in the untreated control group regardless of health status.
Limitations
This experiment dealt only with macroscopical and histopathological changes. Further studies should correlate macroscopical and microscopical changes with blood inflammatory markers.
Conclusion
Clinical and histological evaluation of wound area and wounded tissue in response to PYC application in healthy and diabetic rats was compared to untreated control wounds and wounds treated with a wound cleanser and SSD. In the combined group, the percent reduction in wound size was statistically significantly different between healthy and diabetic rats (50.91% versus 47.42%). The greatest wound size reduction was achieved by the group treated with PYC (53.03%), followed by wounds treated with cleanser/SSD (48.76%) and untreated wounds (45.73%), both in healthy and diabetic rats. Histopathological changes such as inflammation reduction, granulation tissue formation, collagen deposition, fibroblast maturation, reepithelialization, and neovascularization scores were similar in response to PYC and cleanser/SSD treatment regardless of the health status of the rats. To further examine the potential effect of PYC on the wound healing process in healthy and diabetic animals, future research should consider blood chemistry variables to correlate alterations with the degree of hyperglycemia that interfere with oxidative status and tissue regeneration ability.
References
1. Li PN, Li H, Zhong LX, et al. Molecular events underlying maggot extract promoted rat in vivo and human in vitro skin wound healing. Wound Repair Regen. 2015;23(1):65–73.
2. Chithra P, Sajithlal GB, Chandrakasan G. Influence of aloe vera on the healing of dermal wounds in diabetic rats. J Ethnopharmacol. 1998;59(3):195–201.
3. Cordeiro JV, Jacinto A. The role of transcription-independent damage signals in the initiation of epithelial wound healing. Nat Rev Mol Cell Biol. 2013;14(4):249–262.
4. Natarajan V, Venugopal PV, Menon T. Effect of Azadarichta indica (neem) on the growth pattern of dermatophtyes. Indian J Med Microbiol. 2003;21(2):98–101.
5. Singh A, Singh DK. Molluscicidal activity of Lawsonia inermis and its binary and tertiary combinations with other plant derived molluscicides. Indian J Exp Biol. 2001;39(3):263–268.
6. Khadeer BMA, Gowdru HB, Rajashekarappa S, Malleshappa KSH, Krishna V. Molecular docking of glycogen synthase kinase3-β inhibitor oleanolic acid and its wound-healing activity in rats. Med Chem Res. 2013;22(1):156–164.
7. Blazsó G, Rohdewald P, Sibbel R, Gábor M. Anti-inflammatory activities of procyanidin-containing extracts from Pinus pinaster sol. In: Antus S, Gabor M, Vetschera K (eds). Flavonoids and Bioflavonoids. Budapest, Hungary: Akademiai Kiado;1995:231–238.
8. Blazsó G, Gábor M, Rohdewald P. Antiinflammatory activities of procyanidin-containing extracts from Pinus pinaster Ait. after oral and cutaneous application. Pharmazie. 1997;52(5):380–382.
9. Saha R. Cosmeceuticals and herbal drugs: Practical uses. IJPSR. 2012;3(1):59–65.
10. Grimm T, Schäfer A, Högger P. Antioxidant activity and inhibition of matrix metalloproteinases by metabolites of maritime pine bark extract (pycnogenol®). Free Radic Biol Med. 2004;36(6):811–822.
11. Blazsó G, Gábor M, Schönlau F, Rohdewald P. Pycnogenol accelerates wound healing and reduces scar formation. Phytother Res. 2004;18(7):579–581.
12. Jeong MJ, Jeong SJ, Lee SH, et al. Effect of pycnogenol on skin wound healing. Appl Microsc. 2013;43(4):133–139.
13. Lipsky BA, Hoey C. Topical antimicrobial therapy for treating chronic wounds. Clin Infect Dis. 2009;49(10):154–159.
14. Reinhardt CS, Geske T, Schmolz M. A topical wound disinfectant (Ethacridine lactate) differentially affects the production of immunoregulatory cytokines in human whole-blood cultures. Wounds. 2005;17(8):213–221.
15. White RJ, Cutting K, Kingsley A. Topical antimicrobials in the control of wound bioburden. Ostomy Wound Manage. 2006;52(8):26–58.
16. Fonder MA, Lazarus GS, Cowan DA, et al. Treating the chronic wound: a practical approach to the care of nonhealing wounds and wound care dressings. J Am Acad Dermatol. 2008;58(2):185–206.
17. Castellano JJ, Shafii SM, Ko F, et al. Comparative evaluation of silver-containing antimicrobial dressings and drugs. Int Wound J. 2007;4(2):114–122.
18. Kjolseth D, Frank JM, Barker JH et al. Comparison of the effects of commonly used wound agents on epithelialization and neovascularization. J Am Coll Surg. 1994;179(3):305–312.
19. Lansdown ABG, Sampson B, Laupattarakasem P Vuttıvırojana A. Silver aids healing in the sterile skin wound: experimental studies in the laboratory rat. Brit J Dermatol. 1997;137(5):728–735.
20. Esteves JC, Aranega AM, Borrasca AG, Fattah CM, Garcia-Junior IR. Repair process of surgical defects filled with autogenous bone grafts in tibiae of diabetic rats. J Appl Oral Sci. 2008;16(5):316–320.
21. Mariano R, Messora M, de Morais A, et al. Bone healing in critical-size defects treated with platelet-rich plasma: a histologic and histometric study in the calvaria of diabetic rat. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(1):72–78.
22. Jaouhari JT, Lazrek HB, Jana M. The hypoglycemic activity of Zygophyllum gaetulum extracts in alloxan-induced hyperglycemic rats. J Ethnopharmacol. 2000;69(1):17–20.
23. Mahmood AA, Mariod AA, Abdelwahab SI, Ismail S, Al-Bayaty F. Potential activity of ethanolic extract of Boesenbergia rotunda (L.) rhizomes extract in accelerating wound healing in rats. J Med Plants Res. 2010;4(15):1570–1576.
24. Kahkeshani N, Farahanikia B, Mahdaviani P, et al. Antioxidant and burn healing potential of Galium odoratum extracts. Res Pharm Sci. 2013;8(3):197–203.
25. Lemo N, Marignac G, Reyes-Gomez E, et al. Cutaneous reepithelialization and wound contraction after cutaneous reepithelialization and wound contraction after skin biopsies in rabbits: a mathematical model for healing and kin biopsies in rabbits: a mathematical model for healing and remodelling index. Vet Arhiv. 2010;80(5):637–652.
26. Abramov Y, Golden B, Sullivan M, et al. Histologic characterization of vaginal vs. abdominal surgical wound healing in a rabbit model. Wound Repair Regen. 2007;15(1):80–86.
27. Altman M, Suleskey C, Delisle R, DeVelasco M. Silver sulfadiazine and hydrocortisone cream 1% in the management of phenol matricectomy. J Am Padiatric Med Assoc. 1990;80(10):545–547.
28. Chen W, Xu K, Zhang H, Shang Y, Hao P. A comparative study on effect of bacterial load in diabetic foot ulcers dealing with iodophor and rivanol respectively. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008;22(5):567–570.
29. Konrad D, Tsunoda M, Weber K, Corney SJ, Ullmann L. Effects of a topical silver sulfadiazine polyurethane dressing (Mikacure) on wound healing in experimentally infected wounds in the pig. A pilot study. J Exp Anima Sci. 2001;42(1):31–43.
30. Kim YS, Cho IH, Jeong MJ, et al. Therapeutic effect of total ginseng saponin on skin wound healing. J Ginseng Res. 2011;35(3):360–367.
31. Hsu S. Green tea and the skin. J Am Acad Dermatol. 2005;52(6):1049–1059.
32. Packer L, Rimbach G, Virgili F. Antioxidant activity and biologic properties of a procyanidin-rich extract from pine (Pinus maritima) bark, pycnogenol. Free Radic Biol Med. 1999;27(5-6):704–724.
33. Peng QL, Buz’Zard AR, Lau B. Research report: pycnogenol protects neurones from amyloid β peptide-induced apoptosis. Brain Res Mol Brain Res. 2002;104(1):55–65.
34. Latif MA, Zaki MZM, Leng TM, et al. Alocasia denudata Engler treatment enhance open wound healing activities in Wistar rat’s skin. J Ethnopharmacol. 2015;176(6):258–267.
35. Cross SE, Naylor L, Coleman RA, Teo TC. An experimental model to investigate the dynamics of wound contraction. Brit J Plast Surg 1995;48(4):189–197.
36. Grimm T, Chovanová Z, Muchová J, et al. Inhibition of NF-kappaB activation and MMP-9 secretion by plasma of human volunteers after ingestion of maritime pine bark extract (Pycnogenol). J Inflamm (Lond). 2006;3(1):1–6.













