A Cross-sectional Study of Chronic Wound-related Pain and Itching
Abstract
Persons with chronic wounds may experience wound-related itch (pruritus) and pain. A cross-sectional study was conducted to examine the occurrence of itch and pain in chronic wounds and the relationship of the intensity between these factors. Patients in an outpatient wound care center, 18 years and older with an open wound, were recruited consecutively over a 5-month period.
The 199 participants (112 [56%] men) had a mean age of 67 years (range 21–98 years); one wound per person was addressed and included venous (31), arterial (23), neuropathic (31), pressure-related (33), traumatic (37), and “other” (41) wounds. Wound-related pain and itch data were obtained using a modified Paul-Pieper Itching Questionnaire and Characteristics of Itch Questionnaire. Responses were hand-recorded and coded without personal identifiers and analyzed using descriptive statistics, and associations among data were assessed using Pearson chi-square, Mantel-Haenszel chi-square, and Cochran-Armitage trend tests. Wound-related itch was significantly associated with participant age (P = 0.011) and employment status (P = 0.003). Wound-related pain was significantly associated only with education level (P = 0.048). Persons with venous wounds had both the largest proportion with wound-related itch (45.2%) and the largest proportion with wound-related pain (61.2%) out of all of the wound types. Persons with diabetic neuropathy had both the smallest proportion with wound-related itch (16.1%) and the smallest proportion with wound-related pain (35.4%) among all of the wound types. Associations between wound type and wound-related itch or pain were not significant. When venous wounds were compared to all other wound types combined, wound-related itch was significantly associated (P = 0.021) with wound type — ie, venous wound type and itch was statistically significant when venous wounds were compared to a combination of all other wound types. Wound-related pain and itch occurred together in 35 participants (17.6%) across all wound types. Pain and itch on the wound were significantly associated (r = .36, P = 0.043), as were pain and itch around the wound (r = .43, P = 0.002). Because pain and itching can occur with chronic wounds and the presence of one factor can affect the other, clinicians need to assess and manage both symptoms in patients with wounds.
Potential Conflicts of Interest: The author received funding to conduct the study through a University Dissertation Fellowship from Wayne State University, Detroit, MI. This study is based on data collected from the same population of 200 persons described in the manuscript Paul J. Characteristics of chronic wounds that itch. Adv Skin Wound Care. 2013;26(7):320–332.
Introduction
According to a review by Hartoch et al,1 chronic wounds affect 0.78% of the population; most persons with chronic wounds are >60 years of age. It has been anecdotally noted that persons with chronic wounds can experience wound-related itching. Many patients with chronic wounds experience wound-related pain.2,3 Both pain and itch are negative wound-related sensations and clinical concerns.
Recent scientific advances have enabled a better understanding of itch physiology. Until 1997, the sensation of itch was thought to follow the same pathways as painful stimuli but with a less intense stimulus, eliciting itch rather than pain. Subsequently, itch-selective neurons were found in humans.4 Schmelz et al4 used microneurography on the peroneal nerves of 53 persons (38 men, ages 22 to 32 years, without signs of neurological or dermatological disease) and compared their ratings of ensuing itch sensations to 21 men (ages 21 to 31 years) regarding histamine-induced sensations. The researchers were able to identify a new class of nociceptors that represent the afferent units that mediate the itch sensation. Heymann5 noted these slow-conducting C-fibers (pruriceptors) that originate in the skin are similar to, but functionally distinct from, pain fibers.
Andrew and Craig6 studied recordings from the lumbosacral spinal cords of 33 anesthetized cats given histamine iontophoresis to offer evidence of histamine-selective spinothalamic tract neurons specific for itch sensation. These researchers also identified itch as a sensation distinct from pain.
Although pain and itch have many similarities, especially in intensity of the resulting distress, they are, in fact, separate phenomena. The purpose of this study was to examine the occurrence of pain and itch in chronic wounds and the relationship between the intensity of these factors. 
Pain and Itch Phenomena
In contrast to pain, which elicits a withdrawal response, itch causes a scratch response to attack and remove the offending irritant and protect the skin and integrity of the body.7 Itch can be inhibited by painful stimuli thermally (hot water), mechanically (scratching), or chemically (histamine). Analgesia actually may cause itch.8,9
Although pain and itch are distinct phenomena, they share similar cyclical responses. For example, aggravation of pain or itch potentiates more of the negative sensation. Wound-related pain is exacerbated by anxiety, initiating a vicious cycle of pain, anxiety, then worsening pain.10 In the itch-scratch cycle, the scratch response causes inflammation and further stimulation of nerve fibers, which results in the sensation of itch. The itch then prompts further scratching and rubbing.11,12
Two forms of central sensitization associated with itch are similar to pain sensitization: punctate hyperkinesis and allokinesis. Punctate hyperkinesis is an intense itch sensation that occurs when an area surrounding an itching site is pricked. Punctate hyperkinesis is similar to punctate hyperalgesia, an intensely painful sensation that occurs when an area immediately surrounding a painful site is pricked, as found with chronic pain conditions.13 Allokinesis is the induction of intense itching by touching or brushing an area around an itching site; it is similar to allodynia in which gentle contact with skin causes pain in chronic pain conditions.13
Phantom sensations of both itch and pain have been described and may have implications for wound-related itch and pain. Phantom pain is a well-recognized phenomenon, but phantom itch is not.14 In a case study, Jacome15 described a patient with bilateral below-knee amputations. The patient was able to relieve severe phantom itch in the area where his feet would have been by scratching in that area; scratching the stumps provided no relief.
Lierman16 interviewed 20 women in a Reach for Recovery program during their first year post-mastectomy to describe phantom sensations experienced and their responses to those sensations. Twelve (12, 60%) of the women had phantom sensations, and seven (35%) experienced phantom nipple sensations including itching (four, 20%), pain (one, 5%), squeezing pressure (one, 5%), and cold (one, 5%). Age and side of mastectomy were not significantly related to phantom sensations. Women with bilateral mastectomies and persons with implants did not experience phantom sensations. Researchers concluded that further studies over time were indicated among larger numbers of persons to increase understanding of the phantom phenomenon and to assist women to cope with the experience.
Wound-related Pain and Itch
Few studies address wound-related pain and itch together. Some studies involving venous wounds described both sensations. Duque et al17 surveyed 100 persons with chronic venous insufficiency about pain and itch (89% women, mean age of patients with itch 47 years). The most common condition was dry skin (74%), followed by itch. The prevalence of itch was 66%; the prevalence of pain was 62%. Co-occurring itch with burning was experienced by 47%; itch with pain was experienced by 44%. The mean duration of itch was 7.8 years, and the average duration of a bout of itching was 9 hours. Itch was most bothersome in the evening. Participants were able to distinguish among itch, burning, and pain. Itch negatively affected quality of life. The authors concluded itch, burning, and pain affected a large proportion of patients with venous disease. Clinicians need to ask patients with mild to moderate venous disease about wound itch and periwound sensations.
Hareendran et al18 used qualitative and quantitative methods to identify health-related quality-of-life issues in persons with venous ulcers (N = 38). The authors found that pain (80.5%) and itching (69.4%), as well as altered appearance (66.7%), loss of sleep (66.6%), functional limitations (58.3%), and disappointment with treatment (50%) were effects of ulceration. Pain, older age, and nonhealing ulcers negatively affected health-related quality of life (P <0.05). The authors concluded that patients’ perspectives should be considered when evaluating treatments for venous leg ulcers.
In a separate qualitative and quantitative three-phase study, Hareendran et al19 conducted indepth interviews and focus group discussions among 36 persons ages 46 to 91 years (24 women) who had venous leg ulcers, then administered a questionnaire to 124 patients with venous ulcers (phase 2), and finally 120 patients with venous ulcers to validate a quality-of-life questionnaire (phase 3). Ulcer duration ranged from 1.5 months to 50 years (M = 40.8 months, SD = 84.0). The researchers found that ulcer itches ranked fourth among 10 symptoms causing distress, following ulcer burns/stings, ulcer hurts, and skin irritated. Mild to moderate pain from the ulcer was reported by 75 (61%) of persons in phase 2 of the study and by 62 (60%) of persons in phase 3. The authors concluded the venous leg ulcer quality-of-life instrument was reliable, valid, sensitive to differences in clinical outcome, and responsive to clinical change.
Other studies describe wound-related pain but not itch. Walshe20 conducted a qualitative study to describe the experience of living with venous leg ulceration. Thirteen (13) elderly persons (12 female, half of them >85 years) with venous ulcers were randomly selected to participate. Symptoms, especially pain, caused restrictions in people’s lives, especially in the ability to walk and to be out. Symptom control was recognized as the priority for persons with venous ulcers.
Price et al2 conducted a cross-sectional, descriptive study among 2,018 patients (57% female; mean age 68.6 years) with a variety of chronic wounds, including 20% diabetic or pressure-related; 7% surgical, traumatic, or burn wounds; and 66% leg ulcers of unknown etiology and found that wound-related pain was reported by 32.2% as never or rarely, 31.1% as quite often, and 36.6% as most or all of the time. Pain with dressing change was considered the worst part of living with a wound by 790 (40.3%) of the participants.
Shukla et al3 conducted a 1-day descriptive study of 50 patients at a wound clinic (26 with acute wounds and 24 with chronic wounds; mean age 40 years). Wound types included traumatic (33, 66%), pressure-related (six, 12%), diabetic (five, 10%), varicose (four, 8%), and idiopathic (two, 4%). Pain was experienced by 46 (92%) of the patients. Of the 50 participants, 31 (63%) rated their pain from 3 to 5 on a 10-mm visual analog scale.
In summary, pain and itch can occur in patients with chronic wounds.
Pain and itch are stressors to the person with a chronic wound and may, in turn, have a negative effect on wound healing.10
The purpose of this study was to examine the occurrence of itch and pain in chronic wounds and the relationship of the intensity between them. The research questions were: 1) What is the frequency of pain and itch related to chronic wounds? 2) How do ratings of wound-related pain compare to ratings of wound-related itch?
Methods
Design and participants. The study was conducted from the end of December 2010 to the end of May 2011 at an outpatient wound care center affiliated with a large teaching hospital in the midwestern United States. The wound care center is staffed with surgeons specializing in plastic, peripheral-vascular, or general surgery; podiatrists; a nurse practitioner; and staff nurses. The primary types of wounds followed at this clinic include vascular (arterial and venous), neuropathic, pressure-related, and traumatic, among others. Consecutive sampling methods were used to recruit participants attending the outpatient center for wound care. Inclusion criteria were: 1) presence of an open wound, 2) age 18 years or older, and 3) able to understand and speak English. Exclusion criteria included: 1) pregnancy, 2) closed surgical wound, 3) a rash in the area of the wound, and 4) a pruritic skin condition involving more than 20% of the body. Use of antipruritic medication did not exclude participants. The study was approved by the Commission of Nursing Scholarship and Research and the Human Investigation Committee (HIC) of the hospital and the HIC of the affiliated university. All participants received an informational letter about the study.
Instruments.
Itch and pain. The Paul-Pieper Itching Questionnaire (PPIQ) is a compilation of questions based on the itch literature and clinical observations. The 15-question instrument included rating scales, yes/no, and multiple choice items. Items addressed presence of wound itch, amount of itch on the wound, amount of itch around the wound, timing of wound itch, and treatments used for wound itch. Similar to the itch questions, three additional questions for this study addressed presence of wound pain, amount of pain on the wound, and amount of pain around the wound using a 0 to 10 scale where 0 was rated as none and 10, unbearable. Items were individually tallied in analysis. A yes response to itch in or around the wound was tallied (combined) for a wound-related itch total, and a yes response to pain in or around the wound was tallied for a wound-related pain total. Reliability of this instrument could not be calculated because it is a survey versus a summative rating scale.
The Characteristics of Itch Questionnaire was developed by Yosipovitch and colleagues based on the Eppendorf Itch Questionnaire.21 The Eppendorf Itch Questionnaire was derived from the short form of the McGill Pain Questionnaire.22 The Characteristics of Itch Questionnaire includes 10 multiple-choice and short-answer demographic and health history items, six yes/no and multiple choice items regarding itch history, 45 itch descriptors, one multiple response item regarding timing of itch, one item to rate itch intensity, and one item to rate scratching. Study participants who reported the presence of wound-related pain or itch were asked to rate their pain or itch on ordinal 0-to-10 scales (10 indicating highest possible level of pain or itch). The Characteristics of Itch Questionnaire has demonstrated a Cronbach alpha coefficient of 0.9 with test-retest reliability of 0.8.21 The McGill Pain Questionnaire has been well tested and has strong reliability and validity.23
Medical record data collection tool. A medical record data collection tool with face validity was used to record wound type/diagnosis, wound age, dermatologic diagnoses, medical history, current medications, and allergies from participant’s medical records.
Procedure. Interviews were conducted in private rooms during a routine visit, with confidentiality of response maintained. The primary investigator read the questionnaires to the participants during face-to-face interviews and hand-recorded the responses on data sheets that were coded and did not include any personal identifiers. Data sheets were kept in a locked file in the primary investigator’s office. The codebook was kept in a separate double-locked file in the primary investigator’s office. The medical record was reviewed for health information. Participants were compensated $10 in appreciation of their time and cooperation. Participation time, with clinic visit activities included, averaged 45 minutes (range 15 – 60 minutes).
Data analysis. Data were analyzed using Statistical Package for the Social Sciences version 19 (IBM Corporation, Chicago, IL), SAS version 9.3 for Windows (SAS Institute, Inc, Cary, NC), R version 2.15.1 for Windows (R Development Teams, available at www.r-project.org), and StatXact9 software (Cytel, Cambridge, MA). Descriptive statistics, including summary statistics for continuous variables and frequency tables for categorical variables, were used. Associations between variables were assessed using Pearson chi-square, Mantel-Haenszel chi-square, and Cochran-Armitage trend tests. Spearman correlation coefficients were calculated to answer the research question concerning the relationship between wound-related pain and itch.
Results
Sample characteristics. A total of 237 patients were asked to participate and/or screened. Thirty-seven (37) either refused to participate or did not meet inclusion criteria. The 199 participants included 112 men (56%), 170 Caucasians (84%), who ranged in age from 21 to 98 years (M = 67, SD = 14.06 years). Ninety-five (95) participants (48%) were married. The most frequent comorbidities were hypertension (124, 62.3%), diabetes mellitus (79, 39.7%), and arthritis (74, 37.2%). The 196 wounds assessed included venous (31), arterial (23), neuropathic (31), pressure-related (33), traumatic (37), and 41 some other type — ie, wounds of unknown or mixed etiology; data on wound type were missing for three participants. Data on wound itch were missing for one female participant.
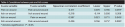
 Wound-related itch was significantly associated with participant age (P = 0.011) and employment status (P = 0.003). Wound-related pain was significantly associated only with education level (P = 0.048) (see Table 1).
Wound-related itch was significantly associated with participant age (P = 0.011) and employment status (P = 0.003). Wound-related pain was significantly associated only with education level (P = 0.048) (see Table 1).
 Persons with venous wounds had both the largest proportion with wound-related itch (45.2%) and the largest proportion with wound-related pain (61.2%) out of all of the wound types (see Table 2). Persons with diabetic neuropathy had both the smallest proportion with wound-related itch (16.1%) and the smallest proportion with wound-related pain (35.4%) among all of the wound types. The associations between wound type and wound-related itch or pain were both nonsignificant. When venous wounds were compared to all other wound types combined, wound-related itch was significantly associated (P = 0.021) with wound type.
Persons with venous wounds had both the largest proportion with wound-related itch (45.2%) and the largest proportion with wound-related pain (61.2%) out of all of the wound types (see Table 2). Persons with diabetic neuropathy had both the smallest proportion with wound-related itch (16.1%) and the smallest proportion with wound-related pain (35.4%) among all of the wound types. The associations between wound type and wound-related itch or pain were both nonsignificant. When venous wounds were compared to all other wound types combined, wound-related itch was significantly associated (P = 0.021) with wound type.
Frequency of wound-related pain and itch. Wound-related pain and wound-related itch were reported by 98 (49.2%) and 56 (28%) of the participants, respectively. Wound-related pain was significantly associated with wound-related itch (P = 0.027). Thirty-five (35, 17.6%) participants reported both pain and itch (see Table 3).
 Comparison of wound-related pain and itch. Assessments of the amount of pain and itch both on and around the wound were compared for the 35 persons who experienced both phenomena (see Table 4). Pain and itch around the wound were significantly correlated (r = .436, P = 0.002), as were amounts of pain and itch on the wound (r = .366, P = 0.043). Amount of wound-related pain correlated positively with wound-related itch (r = .17, P = 0.02).
Comparison of wound-related pain and itch. Assessments of the amount of pain and itch both on and around the wound were compared for the 35 persons who experienced both phenomena (see Table 4). Pain and itch around the wound were significantly correlated (r = .436, P = 0.002), as were amounts of pain and itch on the wound (r = .366, P = 0.043). Amount of wound-related pain correlated positively with wound-related itch (r = .17, P = 0.02).
Discussion
The purpose of this study was to examine the occurrence of itch and pain in chronic wounds and the relationship between intensity of wound-related pain and itch. Although wound-related pain was reported with greater frequency than wound-related itch (98 compared to 56 participants), both negative sensations were encountered by 35 (17.6%) participants.
Wound-related itch was significantly associated with participant age (P = 0.011) and employment status (P = 0.003), and wound-related pain was significantly associated with education level (P = 0.048). It is not surprising that wound-related itch was associated with participant age. Norman24 describes xerosis (dry, cracked skin) as characteristic of advanced age. The association of wound-related itch with employment status (greater itch with retirement) may represent pruritus with advanced age. No explanation can be given for the association of wound-related pain with educational level.
Most participants, regardless of wound type, did not experience wound-related itch, but persons with venous, traumatic, and pressure-related wounds had more wound-related pain. Although wound type was not significantly associated with wound-related pain or itch, it may have been difficult to discern related to the large number of wound type categories and few numbers of some wound types.
The ratings of amounts of pain and itch on 0 to 10 scales of pain on the wound (M = 2.59) were greater than the ratings of itch on the wound (M = 0.49). A total itch rating of 0.96 is high compared to the findings of Duque et al,17 who reported an itch intensity of 0.29 where intensity scores were measured along a 10-cm visual analog scale (with 10 being worst). The total pain rating of 2.47 is similar to the results of Goncalves et al’s25 descriptive, cross-sectional study to describe the characteristics of pain in persons with chronic leg ulcers; among 90 persons with chronic leg ulcers (81.1% venous), pain intensity was rated 3.1 out of 10. Nemeth et al26 conducted a descriptive, cross-sectional study of 255 persons with pure and mixed venous leg ulcer pain to determine point prevalence of venous leg ulcers over autumn, winter, and spring; mean pain severity scores were <3 (10-point scale). In Walshe’s study,20 persons with venous ulcers providing unstructured interviews described the leg ulceration experience to be overwhelmingly painful. Shukla et al3 studied pain as experienced by 50 persons with wounds and found 88% of the participants described mild to moderate pain that interfered with physical activity (40 participants, 87%) and social functioning (23 participants, 50%). Price et al2 administered a survey internationally to a total of 2,018 patients with various types of chronic wounds and found that patients (36.6%) reported wound-related pain most or all of the time.
Participants in the current study were able to distinguish between the two sensations, both in terms of sensation location and ratings. It is interesting to note that pain on the wound was rated proportionally higher than pain around the wound, while itch around the wound was rated higher than itch on the wound. This finding may have implications for interventions, especially for topical therapy. Wound-related pain might be treated with systemic analgesics, while wound-related itch might be treated with application of products around the open wound.
The significant associations between wound-related itch and pain indicate that painful wounds also should be assessed for itchiness. More accurately, the absence of one of the two sensations in the presence of a wound is likely to indicate the absence of the other sensation, as evidenced by the low incidence itch and pain with neuropathic wounds (see Table 2). These findings demonstrate the close physiological interaction between itch and pain. Itch sensitization in the periphery and in the central nervous system has many similarities to pain sensitization.27 Pain inhibits itch, while itch can be induced by exogenous opiates.7 This supports the sensitivity and selectivity theories of itch.27 The specificity theory suggests sensory neurons that are specific to itch stimuli. The selectivity theory suggests that itch neurons also can be excited by painful stimuli. Both theories have been supported by physiological findings.28 The fact that pain and itch activate the same areas of the brain implies a different pattern of activation for the two stimuli.27
Limitations
Pain and itch are subjective phenomena; the ability to describe them is dependent on self-report and recall. Inconsistencies were found in responses about the presence of wound-related pain and itch and amounts of pain and itch in and around the wound. Participants, especially the very elderly, had difficulty assigning numeric values to the sensations. The interviews were lengthy when both wound-related pain and itch were experienced, possibly resulting in inconsistencies. Bias may have been introduced related to answering the same questions about pain and itch. Interpretation of the sensations was likely altered by the wound care visit process, which was taking place simultaneously with the interview, including anesthetic gel application and wound debridement. The sample size, as well as the fact that the majority of patients were Caucasian, limits validity and generalizability of the findings.
Conclusion
This study explored wound itch and pain and compared the two sensations. Occurrence of pain and itch related to chronic wounds occurred with venous, arterial, traumatic, pressure-related, and other wound types. Pain and itch scores on and around the wound were significantly related (r = .36, P = 0.043 and r = .43, P = 0.002, respectively). This study is intended to advance awareness and understanding of itch and pain related to chronic wounds so both might be assessed and managed to promote healing and quality of life. Further studies with larger and different populations to ensure validity and allow generalization of the findings are warranted.
Acknowledgment
The author gratefully acknowledges the assistance of Barbara Pieper, PhD, RN, ACNS-BC, CWOCN, FAAN, and Charity Chen, MS.
Dr. Paul is a Plastic Surgery Nurse Practitioner, William Beaumont Hospital, Royal Oak, MI. Please address correspondence to: Julia Paul, PhD, RN, ACNS-BC, CCRN, CWS, NP, William Beaumont Hospital, 3601 West Thirteen Mile Road, Royal Oak, MI 48073; email: jpaul@beaumont.edu.
1. Hartoch RS, McManus JG, Knapp S, Buettner MF. Emergency management of chronic wounds. Emergency Med Clin North Am. 2007;25(1):203–221.
2. Price PE, Fagervik-Morton H, Mudge EJ, Beele H, Ruiz JC, Nysrom TH, et al. Dressing-related pain in patients with chronic wounds: an international perspective. Int Wound J. 2008;5(2):159–171.
3. Shukla D, Tripathi AK, Agrawal S, Ansari MA, Rastogi A, Shukla VK. Pain in acute and chronic wounds: a descriptive study. Ostomy Wound Manage. 2005;51(11):47–51.
4. Schmelz M, Schmidt, R, Bickel A, Handwerker, HO,Torebjork HE. Specific C-receptors for itch in human skin. J Neurosci. 1997;17(20):8003–8008.
5. Heymann WR. Itch. J Am Acad Dermatol. 2006;54(4):705–706.
6. Andrew D, Craig AD. Spinothalamic lamina I neurons selectively sensitive to histamine: a central neural pathway for itch. Nature Neurosci. 2001;4(1):72–77.
7. Paus R, Schmelz M, Biro T, Steinhoff M. Frontiers in pruritus research: scratching the brain for more effective itch therapy. J Clin Invest. 2006;116(5):1174–1186.
8. Stander S, Schmelz M. Chronic itch and pain — similarities and differences. Eur J Pain. 2006;10(5):473–478.
9. Waxler B, Dadabhoy ZP, Stojiljkovic L, Rabito SF. Primer of postoperative pruritus for anesthesiologists. Anesthesiology. 2005;103(1):168–178.
10. Woo KY. Exploring the effects of pain and stress on wound healing. Adv Skin Wound Care. 2012; 25(1):38–44.
11. Stander S, Steinhoff M, Schmelz M, Weisshaar E, Metze D, Luger T. Neurophysiology of pruritus: cutaneous elicitation of itch. Arch Dermatol. 2003;139:1463–1470.
12. Yosipovitch G, Hundley JL. Practical guidelines for the relief of itch. Dermatol Nurs. 2004;16(4):325–329.
13. Yosipovitch G, Papoiu ADP. What causes itch in atopic dermatitis? Curr Allergy Asthma Rep. 2008;8:306–311.
14. Yosipovitch G, Goodkin R, Wingard EM, Bernhard JD. Neuropathic pruritus. In: Yosipovitch G, Greaves MW, Fleischer AB Jr, McGlone F, eds. Itch: Basic Mechanisms and Therapy. New York, NY: Marcel Dekker Inc;2004:1–4.
15. Jacome D. Phantom itch relieved by scratching phantom feet. JAMA. 1978;240(22):2432.
16. Lierman LM. Phantom breast experiences after mastectomy. Oncol Nurs Forum. 1988;15(1):41–44.
17. Duque MI, Yosipovitch G, Chan YH Smith R, Levy P. Itch, pain, and burning sensation are common symptoms in mild to moderate chronic venous insufficiency with an impact on quality of life. J Am Acad Dermatol. 2005;53(3):504–508.
18. Hareendran A, Bradbury A, Budd J, Geroulakos G, Hobbs R, Kenkre J, et al. Measuring the impact of venous leg ulcers on quality of life. J Wound Care. 2005;14(2):53–57.
19. Hareendran A, Doll H, Wild D J, Moffatt C J, Musgrove E, Wheatley C, et al. The Venous Leg Ulcer Quality of Life (VLU-QoL) questionnaire: development and psychometric validation. Wound Repair Regener. 2007;15(4):465–473.
20. Walshe C. Living with a venous leg ulcer: a descriptive study of patients’ experiences. J Adv Nurs. 1995;22(6):1092–1100.
21. Dawn AD, Papoiu A P, Chan YH, Rapp SR, Rassette N, Yosipovitch G. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. Br J Dermatol. 2008;160(3):642–644.
22. Darsow U, Scharein E, Simon D, Walter G, Bromm B, Ring J. New aspects of itch pathophysiology: component analysis of atopic itch using the Eppendorf Itch Questionnaire. Int Arch Allergy Immunol. 2001;124(1–3):326–331.
23. Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1(3):277–299.
24. Norman RA. Xerosis and pruritus in the elderly: recognition and management. Dermatol Ther. 2003;14(3)254–259.
25. Goncalves ML, de Gouveia Santos VLC, de Mattos Pimenta CA, Suzuki E, Komagae KM. Pain in chronic leg ulcers. J Wound Ostomy Continence Nurs. 2004;31(5):275–283.
26. Nemeth KA, Harrison MB, Graham ID, Burke S. Pain in pure and mixed aetiology venous leg ulcers: a three-phase point prevalence study. J Wound Care. 2003;12(9):336–340.
27. Schmelz M. Modulators of pruritus: peripheral and central sensitization. In: Misery L, Stander S, eds. Pruritus. London, UK: Springer-Verlag;2010:22–29.
28. Patel TS, Yosipovitch G. Central transmission: from skin to brain. In: Misery L, Stander S, eds. Pruritus. London, UK: Springer-Verlag;2010:23–26.













