The Correlation Between Ostomy Knowledge and Self-Care Ability with Psychosocial Adjustment in Chinese Patients with a Permanent Colostomy: A Descriptive Study
Abstract
A colostomy can have a negative impact on patient quality of life. Research suggests that psychosocial adaptation is positively associated with quality of life, but few reports address this adaptation and its related factors in patients with a permanent colostomy.
A 4-month, descriptive study was conducted to assess the impact of ostomy knowledge and ability to self-care on the psychosocial adjustment of 54 Chinese outpatients (47 men, 14 participants 40 to 50 years old, 40 participants 50 to 70 years old) with a permanent colostomy to investigate the correlation between stoma knowledge, self-care ability, and psychosocial adjustment. Assessment instruments included a sociodemographic data questionnaire and a Chinese translation of the Ostomy Adjustment Inventory-23 that comprises 20 items in three domains (positive emotions, negative emotions, and social life). Participants rated statements on a scale from 0 (totally disagree) to 4 (totally agree); a score of 40 indicates a low level of psychosocial adjustment. Participants also completed the Stoma-related Knowledge Scale, comprising 14 5-point Likert scale questions where low scores indicate low knowledge, and they answered one question regarding self-care ability. Data were analyzed using statistical software for social science. The average stoma-related knowledge score suggested moderate levels of knowledge (45.112 ± 13.358). Twenty (20) participants managed all stoma care aspects independently, 30 required some assistance, and four (4) required care by someone else. The three domains of psychosocial adjustment scores (positive emotions, negative emotions, and social life) were 17.60 ± 4.093,12.92 ± 3.440, and 19.15 ± 6.316, respectively. Knowledge and the three domains of psychosocial adjustment were positively correlated with positive emotion (r = .610, P = 0.001), negative emotion (r = .696, P = 0.000), and social life adjustment (r = .617, P = 0.001). A significant difference in psychosocial adjustment scores was found between persons who did (57.37 ± 9.81) and those that did not (47.83 ± 8.18) independently care for their own stoma (P = 0.005). Persons with high levels of knowledge and independence had a high level of psychosocial adjustment. Providing knowledge and emphasizing/teaching self-care may help persons with a colostomy make the necessary daily and social life adaptations.
Potential Conflicts of Interest: none disclosed
Introduction
For most patients (especially those with a permanent colostomy), being discharged from the hospital is an important milestone in their recovery. They now will need to cope not only with surgical healing, but also with changes related to their stoma with regard to usual activities and lifestyle. A new stoma can be both physically and psychologically challenging. Colostomies are known to affect patient quality of life1-4; problems and concerns include inability to control gas, difficulties in activities of travel and leisure, self-abasement, and loneliness. Results of a descriptive study by Simmons et al5 showed patients who had a high level of psychosocial adjustment had high quality-of-life scores. However, studies regarding psychosocial adjustment of patients with permanent colostomy and its related factors are scant. The purpose of this prospective, descriptive study was to assess ostomy knowledge, self-care ability, and psychosocial adjustment in Chinese patients with a permanent colostomy and to investigate the correlation among these three characteristics. 
Methods
Setting. The study was conducted from January through April 2011. Data were collected from patients cared for in the intestinal surgery department of Jiang Su Cancer Hospital when they returned for follow-up.
Participants. A convenience sample of patients with a permanent colostomy was solicited. Inclusion criteria were 1) age between 18 and 75 years, 2) no acute or chronic disease that influences daily activities, and 3) no mental disorder. The study team comprised ostomy and enterostomal therapy (ET) nurses.
The descriptive, correlation study was approved by the nursing department and by the ethics committee at the hospital. The purpose of the study was explained to patients, and written informed consent was obtained. Respondents read and completed questionnaires.
Instruments.
Sociodemographic information. A sociodemographic data questionnaire was used to collect information about patients’ gender, age, marital status, education level, and caregiver.
Psychosocial adjustment scale. A psychosocial adjustment scale for persons with a stoma, developed by Simmons et al,6 was translated into Chinese by the study team for this endeavor. The Chinese version of the scale consisted of 20 items covering three domains: positive emotion, negative emotion, and social life adaptation. Participants responded to the statement in each item using a scale where 0 = totally disagree and 4 = totally agree. The higher the score, the better the psychosocial adjustment; a score of 60 to 80 indicated a high level of psychosocial adjustment, 40 to 59 indicated middle level of psychosocial adjustment, and a score <40 indicated low level of psychosocial adjustment. The internal consistency was previously shown to be .869, and the test-retest reliability over a 1-week period was .68.7
Stoma-related Knowledge Scale. The Stoma-related Knowledge Scale was derived from the Nursing Outcome Classification.8 The scale is comprised of 14 items that assess knowledge about colostomy care, colostomy products, colostomy irrigation, and other relevant factors. The response format for each item was a 5-point Likert-type scale with rating options from 1 (not at all known) to 5 (totally known). High scores represent higher level of knowledge. Scores of 41 to 60 indicate a high level stoma-related knowledge, 21 to 40 middle level of stoma-related knowledge, and <20 low level of stoma-related knowledge.
Self -care ability. Participants were asked whether they care totally for themselves (ie, they can clean and change the ostomy pouch by themselves), partly care for themselves (ie, they can clean the ostomy pouch by themselves but cannot change the stoma appliance), or require care for all stoma care aspects from someone else (ie, they cannot clean and change the stoma pouch.)
Procedure. Patients returning to the hospital for follow-up were provided the questionnaire, which took approximately 15 minutes to complete.
Data collection. Researchers collected the questionnaires when they were completed. All data were entered without names into the Statistical Package for Social Science (SPSS, Chicago, IL).
Data analysis. Data were analyzed using SPSS software. Correlations between psychosocial adjustment and stoma-related knowledge were analyzed using person product moment correlations. One-way ANOVA analysis assessed the correlation between self-care ability and psychosocial adjustment. A P value <0.05 was used to indicate statistical significance.
Results
Demographics. During the study period, 62 patients were invited to participate. Six refused, and two did not complete the study because they were unable to read or write. Of the 54 participants, 47 were male. Most (40) respondents ranged in age from 50 to 70 years old; 14 patients were 40 to 50 years old. Forty-seven (47) patients had completed higher education, and seven (7) patients had completed primary education. Most (48) patients received care from their spouses.
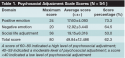
Psychosocial adjustment level. The mean total score of the psychosocial adjustment scale was 49.84 ± 12.486, which was in the middle level of psychosocial adjustment. Average scores from the three domains of psychosocial adjustment (positive emotion, negative emotion, and social life adaptation) were 17.60 ± 4.093, 12.92 ± 3.440, and 19.15 ± 6.316, respectively (see Table 1).
Stoma-related knowledge level. The mean total score of stoma-related knowledge was good (45.112 ± 13.358). Participants scored highest on understanding the need for sufficient daily water intake and how to change the ostomy pouch (see Table 2).
Self-care ability. Of the 54 respondents, 20 managed the stoma on their own, 30 patients managed with some help, and four received care from someone else.
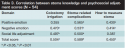
Correlation between knowledge and psychosocial adjustment. Significant positive correlations were found between knowledge and positive emotion scores (r = .610, P = 0.001), negative emotion (r = .696, P = 0.000), and social life adjustment (r = .617, P = 0.001) (see Table 3). Knowledge about colostomy irrigation was highly correlated with social life adjustment.

Correlation between self care ability and psychosocial adjustment. Of the 54 participants, 20 (37%) managed all aspects of stoma care by themselves, 30 (55%) indicated needing assistance with appliance changes only, and four (4, 8%) required care from someone else for all aspects of stoma care. Psychosocial adjustment scores were significantly higher (57.37 ± 9.81) among participants who managed all aspects of stoma care by themselves than among persons who required care from someone else for all aspects of stoma care (47.83 ± 8.18, P = 0.005).
Discussion
Psychosocial adjustment. Caring for patients with a permanent colostomy involves both physical and psychosocial rehabilitation. In a qualitative analysis by Krouse et al,9 quality of life among persons with a stoma was not high due to psychosocial adjustment issues, despite improvement in stoma care. Simmons et al5 showed psychosocial adjustment in patients with a permanent colostomy was positively related to quality of life; patients who had high psychosocial adjustment scores enjoyed high quality of life. In the current study, the psychosocial adjustment score was 49.84 ± 12.486, (about mid-level), with the lowest score in social life adjustment. These results indicate a colostomy negatively affects the patient’s social life, so healthcare providers should acknowledge and help address an ostomate’s potential social life concerns following discharge.
Knowledge. Patients with a permanent colostomy wear an appliance to collect feces for the rest of their lives. To return to their previous life activities, patients must acquire knowledge and skills — eg, the ability to perform normal stoma care, identify problems, care for peristomal skin, and understand how to prevent and treat potential complications.
This study showed patients have some but not a great deal of knowledge regarding their stoma; the lowest scores were in colostomy irrigation, stoma-related complications, and how to measure a stoma. China has few enterostomal therapists (ETs), and most of them work in big urban hospitals. In the authors experience, many patients come from rural areas; they had very little contact with an ET following discharge from the hospital. Thus, patients should be taught about knowledge of stoma caring as early as possible.
Colostomy irrigation involves irrigating the colon regularly to establish a regular bowel habit.10 Controlled studies11,12 found that colostomy irrigation can help improve patient quality of life.
In this study, knowledge about colostomy irrigation received the lowest knowledge score. As observed in the authors’ clinic, most patients prefer to not irrigate (in part because of economic and living conditions), show no interest in learning about irrigation, and choose not perform this task. A mixed method quantitative and qualitative study about nurses’ perceptions of ostomy patients by Carlsson et al13 found that almost all patients who use colostomy irrigation associated it with the positive aspects of feeling secure and having an empty pouch. The stoma nurse should introduce more information about colostomy irrigation for patients to potentially help address concern about this management option.
Correlation between knowledge and psychosocial adjustment. This study showed stoma knowledge was positively associated with psychosocial adjustment, inferring the greater the stoma-related knowledge, the better the patient’s adjustment to life with a stoma. This finding is similar to Hu et al’s14 descriptive study results, which found patients who were provided information before surgery adjusted better to their new situation than those who had not received relevant information. Stoma knowledge included diet, cleaning activities, and peristomal skin care — factors related to everyday life and that influence patients’ psychosocial adaptability. The current study indicated the stoma nurse should provide knowledge in different stages to help patients return to their normal life more expediently.
Correlation between self-care ability and psychosocial adjustment. Results of the current study also found that self-care ability was an important factor in psychosocial adjustment. Patients who can totally care for themselves had higher levels of psychosocial adjustment. The study by Metcalf15 found patients who master self-care skills make better social adjustments. Hu et al16 also observed that ability to self-care was correlated positively with level of psychosocial adjustment. The results of these studies all suggest that facilitating patient ability to manage all aspects of stoma care by themselves should be a priority, preferably before hospital discharge.
Limitations
This study only addressed the correlation between knowledge and self-care ability and psychosocial adjustment. The small sample size and the acknowledgment that other factors may be associated with psychosocial adjustment limit the extent of the conclusions drawn and underscore the need for further investigation of what clinicians can do to help patients cope with their ostomies.
Conclusion
In this study, patients with higher levels of knowledge about stoma care and those who can manage all aspects of care independently were more psychosocially adjusted to their stomas than persons with less knowledge and more dependence on others for care. The results of this and other studies suggest providing knowledge and emphasizing/teaching self-care before hospital discharge may optimize quality of life for persons with a colostomy.
Acknowledgment
The authors are sincerely grateful to all patients who participated in the study.
Dr. Cheng is an ostomy nurse, Ms. Meng is head nurse, and Ms. Yang and Ms. Zhang are enterostomal therapy nurses, Jiang Su Cancer Hospital, Nanjing, PR China, Please address correspondence to: Ai-Feng Meng, Surgery Department, Jiang Su Cancer Hospital, 42 Baiziting Street, 210009 Nanjing, PR China; email: 313913065@qq.com.
1. Charúa-Guindic L, Benavides-León CJ, Villanueva-Herrero JA, Jimnez-Bobadilla B, Abdo-Francis JM, Hernanez-Labra E. Quality of life in ostomized patients. Cir Cir. 2011;79(2):149–55.
2. Dabirian A, Yaghmaei F, Rassouli M, Tafreshi MZ. Quality of life in ostomy patients: a qualitative study. Patient Prefer Adherence. 2010;5:1–5.
3. Cakmak A, Aylaz G, Kuzu MA. Permanent stoma not only affects patients’ quality of life but also that of their spouses. World J Surg. 2010;34(12):2872–2876.
4. Pomazkin VI. Assessment of the quality of life in patients with intestinal stomas. Vopr Onkol. 2010;56(2):182–184.
5. Simmons KL, Smith JA, Bobb KA, Liles LL. Adjustment to colostomy: stoma acceptance, stoma care self-efficacy and interpersonal relationships. J Adv Nurs. 2007;60(6):627–635.
6. Simmons KL, Smith JA, Maekawa A. Development and psychometric evaluation of the Ostomy Adjustment Inventory-23. J Wound Ostomy Continence Nurs. 2009;36(1):69–76.
7. Xu Q, Cheng F, Dai XD. The test of reliability and validity of Chinese version of psychosocial adjustment scale. J JiangSu Med. 2010;14:1647–1649.
8. Donahue MP, Brighton V. Nursing outcome classification: development and implementation. J Nurs Care Qual. 1998;12(5):588–594.
9. Krouse RS, Grant M, Rawl SM, Mohler MJ, Baldwin CM, Coons SJ, et al. Coping and acceptance: the greatest challenge for veterans with intestinal stomas. J Psychosom Res. 2009;66(3):227–233.
10. Varma S. Issues in irrigation for people with permanent colostomy: a review. Br J Nurs. 2009;18(suppl 4):S15–S18.
11. Cesaretti IU, Santos VL, Vianna LA. Quality of life of colostomized person with or without use of methods of bowel control. Rev Bras Enferm. 2010;63(1):16–21.
12. Karadag A, Mentes BB, Ayaz S. Colostomy irrigation: results of 25 cases with particular reference to quality of life. J Clin Nurs. 2005;14(4):479–485.
13. Carlsson E, Gylin M, Nilsson L, Svensson K, Alverslid I, Persson E. Positive and negative aspects of colostomy irrigation: a patient and WOC nurse perspective. J Wound Ostomy Continence Nurs. 2010;37(5):511–516.
14. Hu A, Zhang MF, Zhang JE. The status and related factors of adjustment in colostomy patients. Chinese J Nurs. 2010;45(2):109–111.
15. Metcalf C. Stoma care: empowering patients through teaching practical skills. Br J Nurs. 1999;8(9):593–570.
16. Hu A, Zhang MF, Chen MX, et al. Correlation between adjustment with self-care ability in patients with colostomy. Paper presented at the Wound Ostomy Continence Nurses Society meeting. June 2010.













