Utility of Radiopaque Bypass Graft Markers During Coronary Angiography Following Coronary Artery Bypass Graft Surgery
Abstract: Background. Radiopaque bypass graft markers allow easy visualization of the location of the graft and can minimize contrast use and radiation exposure during follow-up coronary angiography. Methods. This retrospective study analyzed coronary artery bypass graft patients who underwent subsequent coronary angiography in the John Cochrane Veterans Affairs Medical Center from January 2009 until September 2017. Results. Patients who underwent diagnostic coronary angiography with proximal graft markers required less contrast use (P<.02) and less fluoroscopy time (P<.01). The presence or absence of proximal graft markers had no significant difference on the rise of creatinine following coronary angiography (P=.28). Conclusion. Bypass graft markers reduce contrast and radiation use in follow-up coronary angiography and reduce incidence of contrast-induced acute kidney injury.
Key words: cardiac imaging, contrast usage, coronary artery disease, radiation dose
Coronary artery disease is a leading cause of mortality and morbidity in the United States and worldwide. It is estimated that 16.5 million Americans have coronary artery disease.1 Coronary artery bypass graft (CABG) surgery has demonstrated significant improvement in mortality when compared with percutaneous coronary intervention (PCI) in patients with multivessel disease.2 Saphenous vein grafts remain essential bypass conduits in CABG surgery. The rate of saphenous graft patency is 50% at 10 years, and a significant number of CABG patients will require percutaneous coronary revascularization. Due to complex graft anatomies, CABG patients are often exposed to greater contrast volume and radiation dose with the associated increased risk of contrast-induced acute kidney injury (CI-AKI). Radiopaque bypass graft markers inserted at the origin of the bypass graft on the ascending aorta allow easy visualization of the location of the graft and can minimize contrast use and radiation exposure during follow-up coronary angiography. The use of bypass graft markers has been shown to reduce catheterization time and the use of contrast agents.3 However, there have been few studies directly comparing the incidence of CI-AKI in patients with graft markers.
The present study sought to evaluate the association of bypass graft markers with the incidence of AKI following diagnostic coronary angiography in CABG patients. The objective of this study was to compare the effect of graft markers on contrast exposure during coronary angiogram and renal function post angiography. The primary hypothesis was that proximal radiopaque graft markers would be associated with decreased contrast medium use and lower incidence of AKI.
Methods
This retrospective study analyzed CABG patients who underwent subsequent coronary angiography at the John Cochrane Veterans Affairs Medical Center from January 2009 until September 2017. Patients who underwent diagnostic coronary angiography without PCI were included. Patients who underwent subsequent peripheral angiography or PCI were excluded because these patients required additional contrast. Health data, including radiation time, amount of contrast used, and creatinine post angiography (at 48 hours to 3 months), were collected.
Statistical analysis. Patients were stratified into two cohorts: patients with proximal graft markers and patients without proximal graft markers. Statistical analysis for comparison of contrast volume, fluoroscopy time, and rise in creatinine was undertaken using paired t-tests to calculate P-values for statistical significance, defined as P<.05.
Results
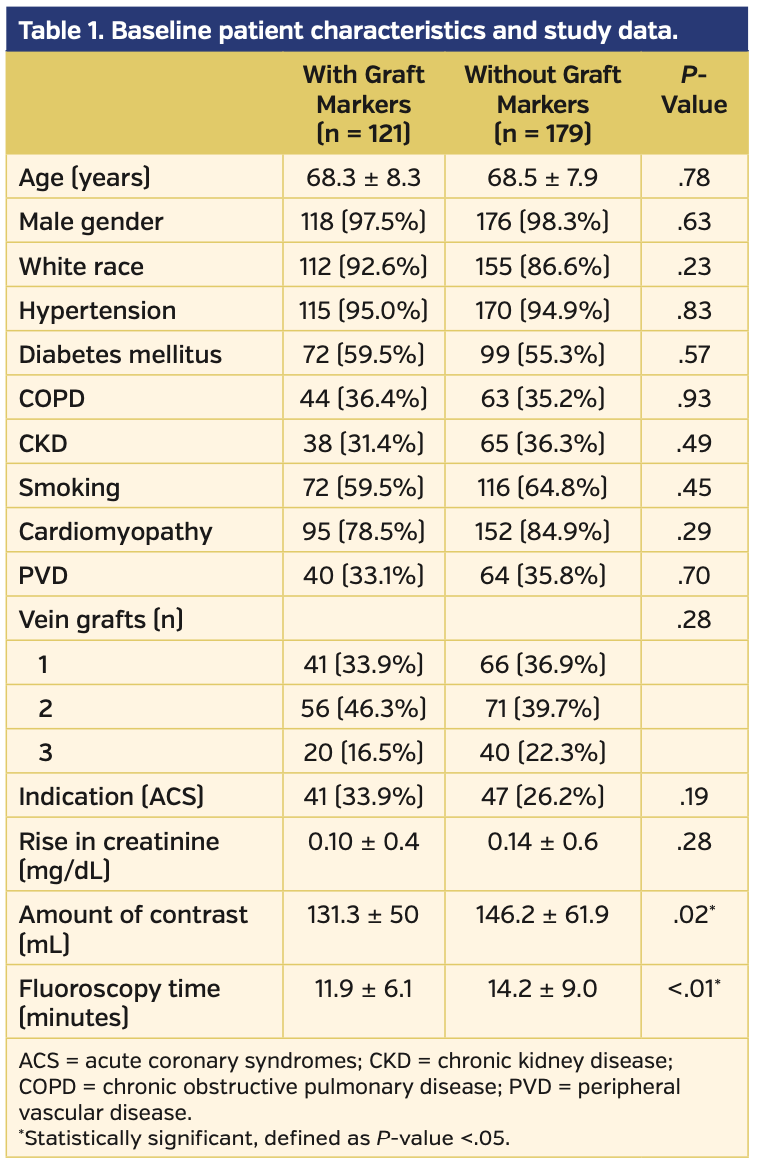
A total of 300 patients were included in the study (121 with graft markers and 179 without graft markers). The majority of the study population were white males suffering from hypertension and underlying cardiomyopathy. Significant comorbidities included diabetes mellitus, chronic obstructive pulmonary disease, chronic kidney disease, peripheral vascular disease, and tobacco abuse. The number of vein grafts ranged from 1-3. Table 1 includes the baseline patient characteristics and study data findings.
The presence or absence of proximal graft markers had no statistically significant difference on the rise of creatinine post coronary angiography (P=.28) (Figure 1). However, patients who underwent diagnostic coronary angiography with proximal graft markers required less contrast use (P<.02) and less fluoroscopy time (P<.01). In patients with multiple vein grafts, the presence of proximal graft markers decreased contrast use and fluoroscopy time (Figures 2 and 3).
Discussion
CABG is a crucial intervention in the treatment of coronary artery disease, and coronary angiography is an important diagnostic tool to evaluate follow-up bypass graft patency. The complexity of graft anatomy in CABG patients increases volume of contrast and subsequent contrast-associated complications, primarily CI-AKI. The use of proximal radiopaque graft markers is often operator and institution dependent. There is also concern of the graft marker affecting long-term bypass patency. A retrospective study by Olenchock et al4 that compared approximately 2000 patients with saphenous vein graft bypass markers with controls found no difference in graft patency at 12-18 months following bypass surgery.
Our analysis showed an absolute decrease in the volume of contrast and a non-statistically significant reduced risk of AKI following coronary angiography compared with patients without graft markers. This study also demonstrated a reduction in radiation exposure during the angiographic procedure. Nephrotoxicity is a well-studied complication in the use of iodinated contrast.5 Patient with acute coronary syndrome undergoing PCI are at especially high risk for CI-AKI, which is likely due to hemodynamic instability and larger volume of contrast used during PCI. CI-AKI is an independent predictor of mortality. A study by Wi et al6 found that patients with CI-AKI have greater in-hospital and 2-year mortality when compared with patients without CI-AKI in a cohort undergoing PCI for acute coronary syndrome.
Multiple studies have consistently illustrated the advantages of proximal radiopaque graft markers in reducing the volume of contrast used.7 The results of the present study supplement previous studies, while also providing objective evidence of the beneficial effect of radiopaque bypass graft markers in preventing subsequent CI-AKI and mortality.
Study limitations. This study may exhibit limited external validity, as the patients included were predominantly white males and included only a patient population receiving care under a Veterans Affairs Medical Center in the United States. In addition, this study was conducted at a single institution and was retrospective in design. Creatinine data post angiography were collected from 48 hours to 3 months, which may have led to confounding or bias in the data. Future prospective studies including larger, randomized patient populations are needed.
Conclusion
This study objectively demonstrates a significant reduction in CI-AKI at follow-up coronary angiography in CABG patients. Radiopaque bypass graft markers reduce subsequent iodinated contrast use and radiation exposure in CABG patients, thereby reducing the risk of CI-AKI and CI-AKI associated mortality. The marking of proximal anastomoses during CABG surgery is a safe and simple procedure that does not affect long-term graft patency while reducing the risk of CI-AKI following angiography.
From the 1Department of Cardiology and 2Department of Internal Medicine, St. Louis University School of Medicine, St Louis, Missouri; and 3Department of Cardiology, John Cochrane Veterans Affairs Medical Center, St. Louis, Missouri.
Disclosure: The authors have completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors report no conflicts of interest regarding the content herein.
Manuscript submitted December 22, 2019, final version accepted December 31, 2019.
Address for correspondence: Julien Feghaly, MD, Saint Louis University, Internal Medicine, 3635 Vista Avenue, St. Louis, MO 63110. Email: julien.feghaly@health.slu.edu
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics — 2018 update: a report From the American Heart Association. Circulation. 2018;137:e67.
- Head SJ, Milojevic M, Daemen J, et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet. 2018;391:939.
- Eisenhauer MD, Collier E 3rd, Eisenhauer TL, Cambier PA. Beneficial impact of aorto-coronary graft markers on post-operative angiography. Cathet Cardiovasc Diagn. 1997;40:249-253.
- Olenchock AS Jr, Karmpaliotis D, Gibson WJ, et al. Impact of saphenous vein graft radiographic markers on clinical events and angiographic parameters. Ann Thorac Surg. 2008;85:520-524.
- Weisbord SD. Iodinated contrast media and the kidney. Rev Cardiovasc Med. 2008;9:14-23.
- Wi J, Ko Y, Kim J, et al. Impact of contrast-induced acute kidney injury with transient or persistent renal dysfunction on long-term outcomes of patients with acute myocardial infarction undergoing percutaneous coronary intervention. Heart. 2011;97:1753-1757.
- Pingpoh C, Siepe M, Burger K, et al. Impact of proximal radiopaque graft markers on post-bypass surgery coronary angiography. J Thorac Cardiovasc Surg. 2018;155:1565-1572.