Right Heart Catheterization: Right From the Anatomical Snuffbox
Key words: distal radial artery access, right heart catheterization
Distal radial artery access for left heart catheterization from the anatomical snuffbox has become more prevalent in clinical practice in the last few years due to its safety and multiple advantages to the patient, operator, and overall procedural ergonomics.1 If an associated right heart catheterization is to be performed from the same upper extremity, it is usually performed from a different anatomical location, ie, the antecubital area (antecubital or cephalic vein) or distal medial arm (basilic or brachial veins).2 This requires a dual procedural field preparation, which adds more time, patient inconvenience, and radiation exposure to the operator, and is not the most ergonomically friendly set-up (Figure 1).
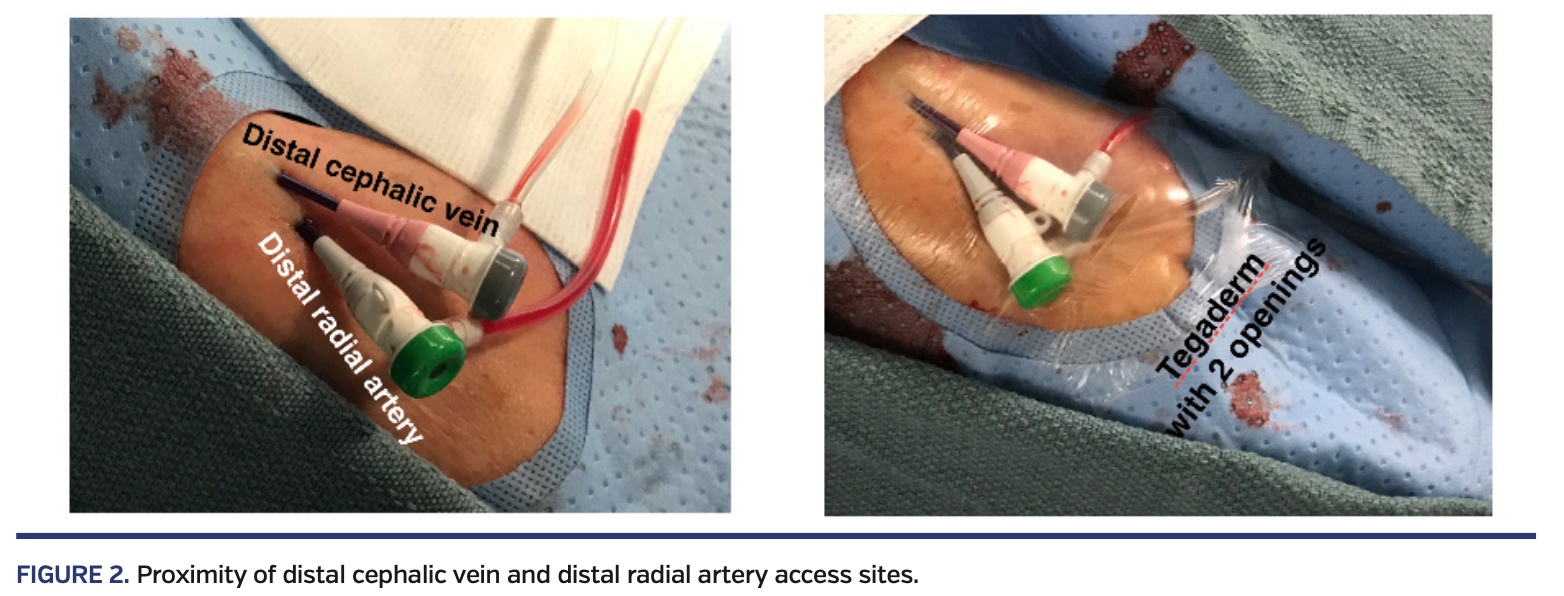
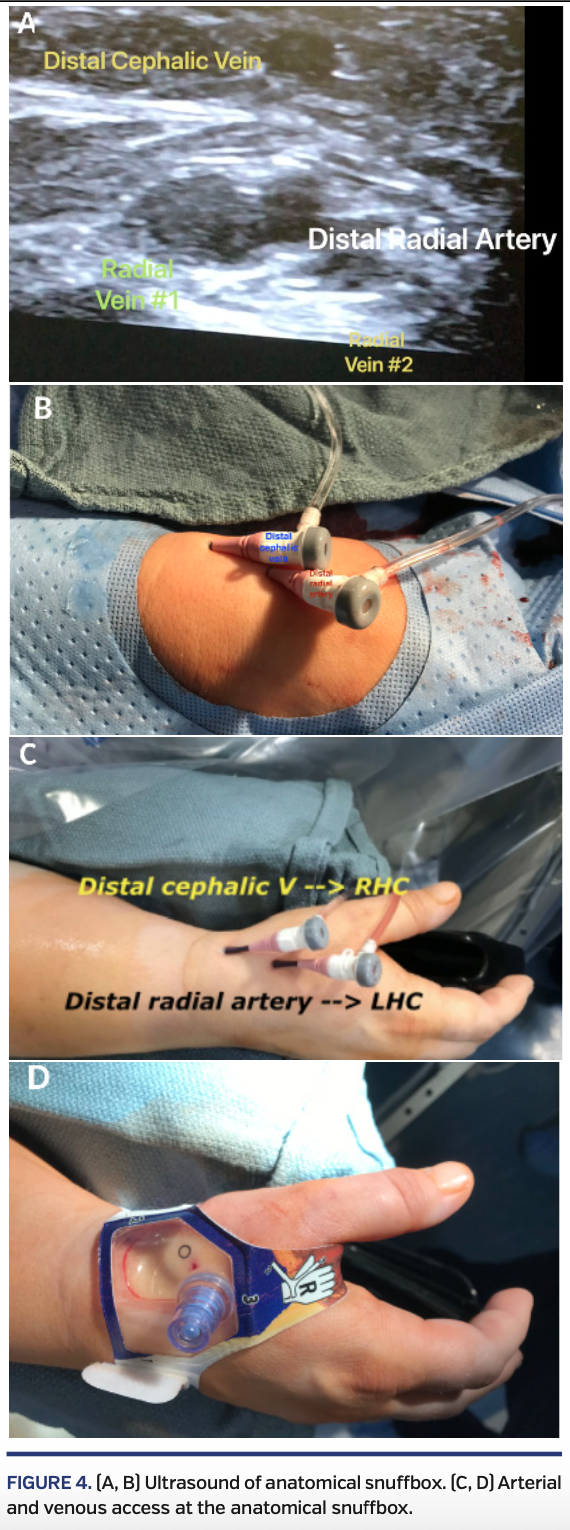
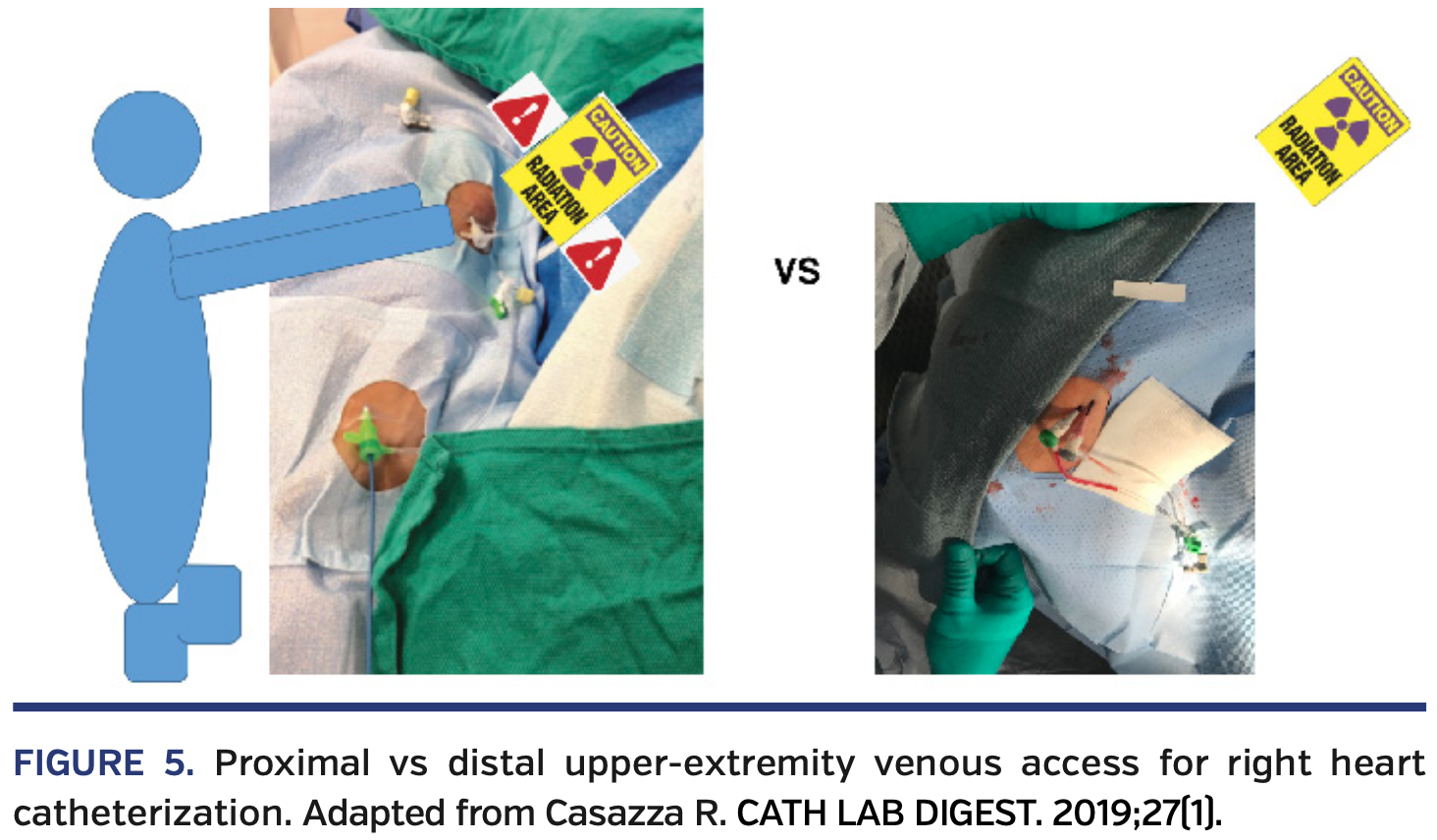
We hereby present the first reported cases of right heart catheterization from the distal cephalic vein in the anatomical snuffbox area (Figure 2). The distal cephalic vein originates from the dorsal metacarpal veins of the hand and courses through the anatomical snuffbox, in the superficial fascia overlying the distal radial artery (Figure 3).3 It often has a similar size as the distal radial artery and this can be significantly increased with a tourniquet placed under the drape at the distal forearm right before venous access (Figure 4; Video 1). The distal cephalic size can often handle 5 to 7 Fr sheaths due to the high venous wall compliance. This allows for convenient access in the same field as the distal radial artery while the patient’s hand is laying in a comfortable, neutral anatomical position right next to the ipsilateral thigh aligned with the body’s longitudinal axis. Even though the traditional distal arm or antecubital venous access allow for positioning of the arm in a similar position after venous access, the operator’s hand, while advancing the right heart catheter, is closer to the radiation source and fluoroscopy field (Figure 5). With this distal venous access technique, the operator’s hand stays farther away from radiation source.
This technique also allows for a more comfortable procedural set-up for the catheterization laboratory staff and a better ergonomic approach for the operator. Instead of reaching up to the venous sheath in the distal arm, which is hard to see while the arm is in a pronated position, a distal venous sheath at the anatomical snuffbox is easily accessible (right next to the arterial access), allows for better catheter handling/torque, and is more comfortable for both the patient and the operator while minimizing radiation exposure.
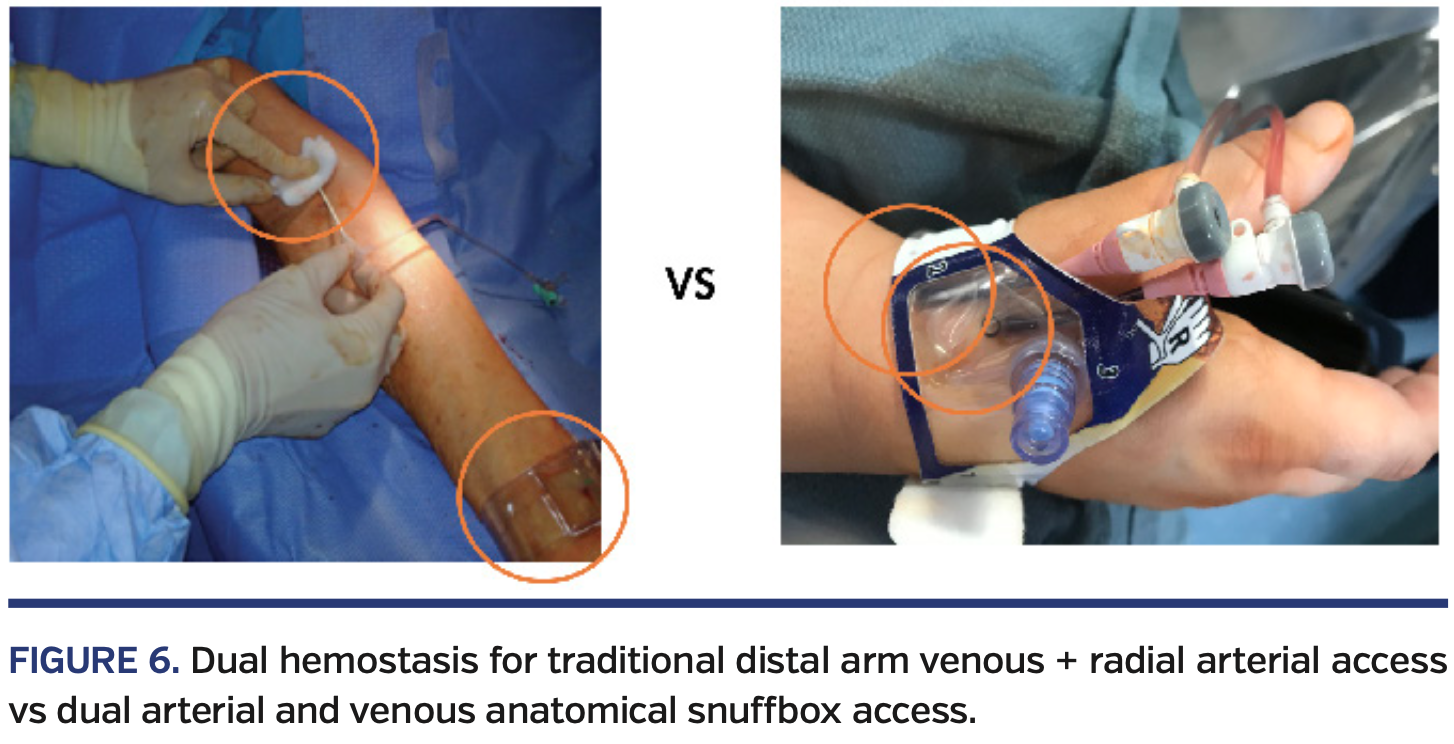
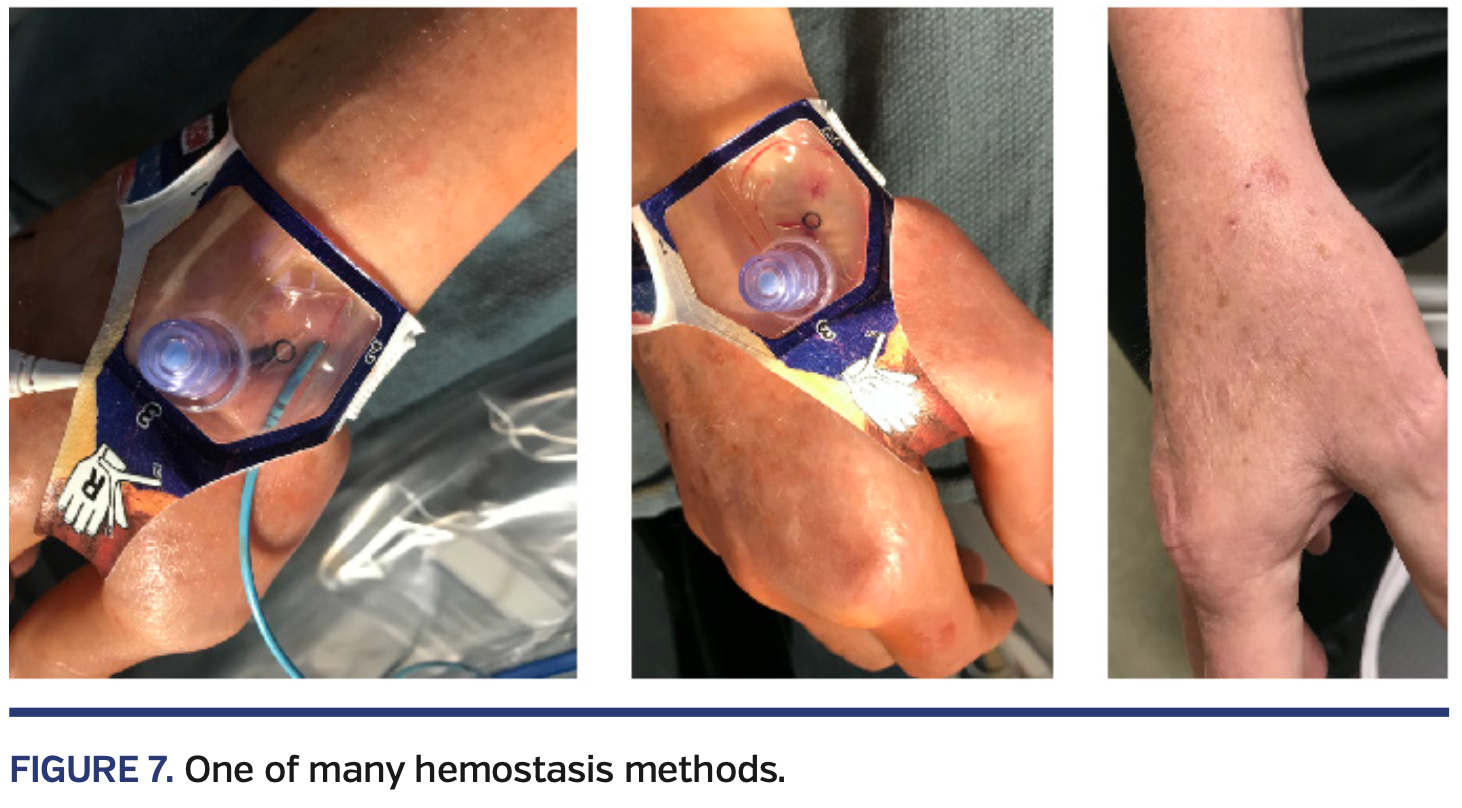
Additionally, it allows for simultaneous arterial and venous hemostasis through the same distal radial compression device since the access sites are so close to each other, hence saving time required for manual hold of the distal arm venous access site and improving patient throughput in the catheterization laboratory (Figures 6 and 7; Video 2).
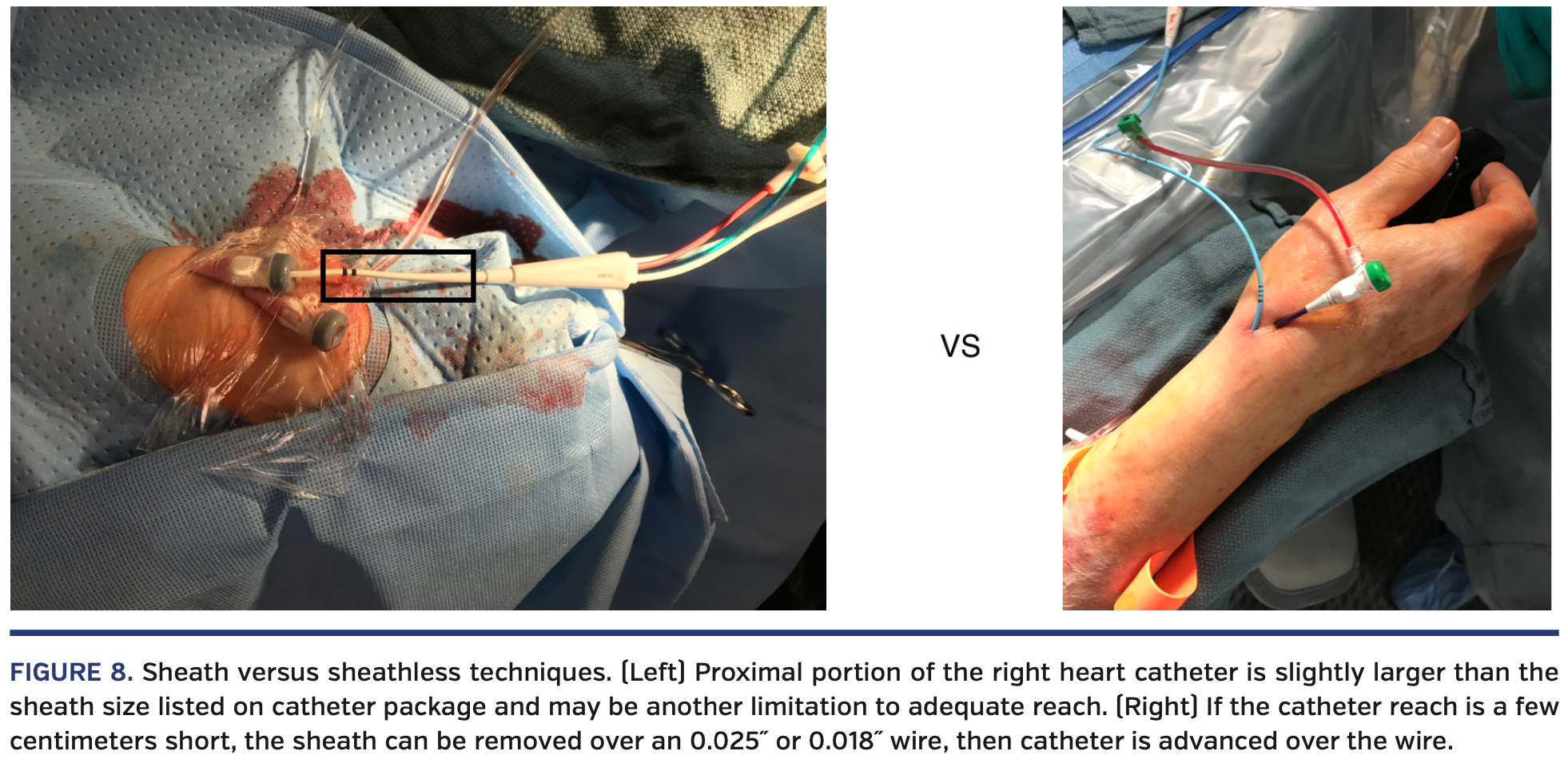
The major downside of this approach is the long distance to the right heart chambers and pulmonary capillary wedge position. As far as we know, there are no right heart catheters on the market longer than 110 cm; hence, most patients taller than 5’6” (168 cm) would not be good candidates for this approach with balloon-tipped catheters. Alternative approaches are: (1) the sheathless technique over 0.018˝ or 0.025˝ wires to gain 5-7 cm of right heart catheter length in the body since this proximal portion of the catheter is slightly larger than the listed sheath size on the catheter package (Figure 8); or (2) 150 cm non-balloon-tipped, flexible, angled catheters with a Tuohy valve over an 0.014˝ wire (eg, 4 Fr angled Navicross catheter; Terumo) just for pressure assessment and estimation of cardiac output by the Fick method without the ability to measure cardiac output by the thermodilution method. However, if the interventional community shows interest in this technique, the industry is likely to respond with the manufacture of longer, balloon-tipped thermodilution catheters (optimally up to 170 cm).
Another disadvantage is the size of the distal cephalic vein at this level, which is significantly smaller than the distal arm basilic or brachial veins and smaller than the mid cephalic or antecubital veins. Ultrasound examination of the distal cephalic vein size and course before preparation and draping of the patient (while a tourniquet is placed around the distal forearm) is definitely recommended prior to the procedure. There are also some situations where the satellite radial veins are larger than the distal cephalic vein and can be accessed instead (Figure 3). Care must be taken to avoid multiple venous punctures, since veins in this location quickly spasm and become inappropriate for further access attempts.
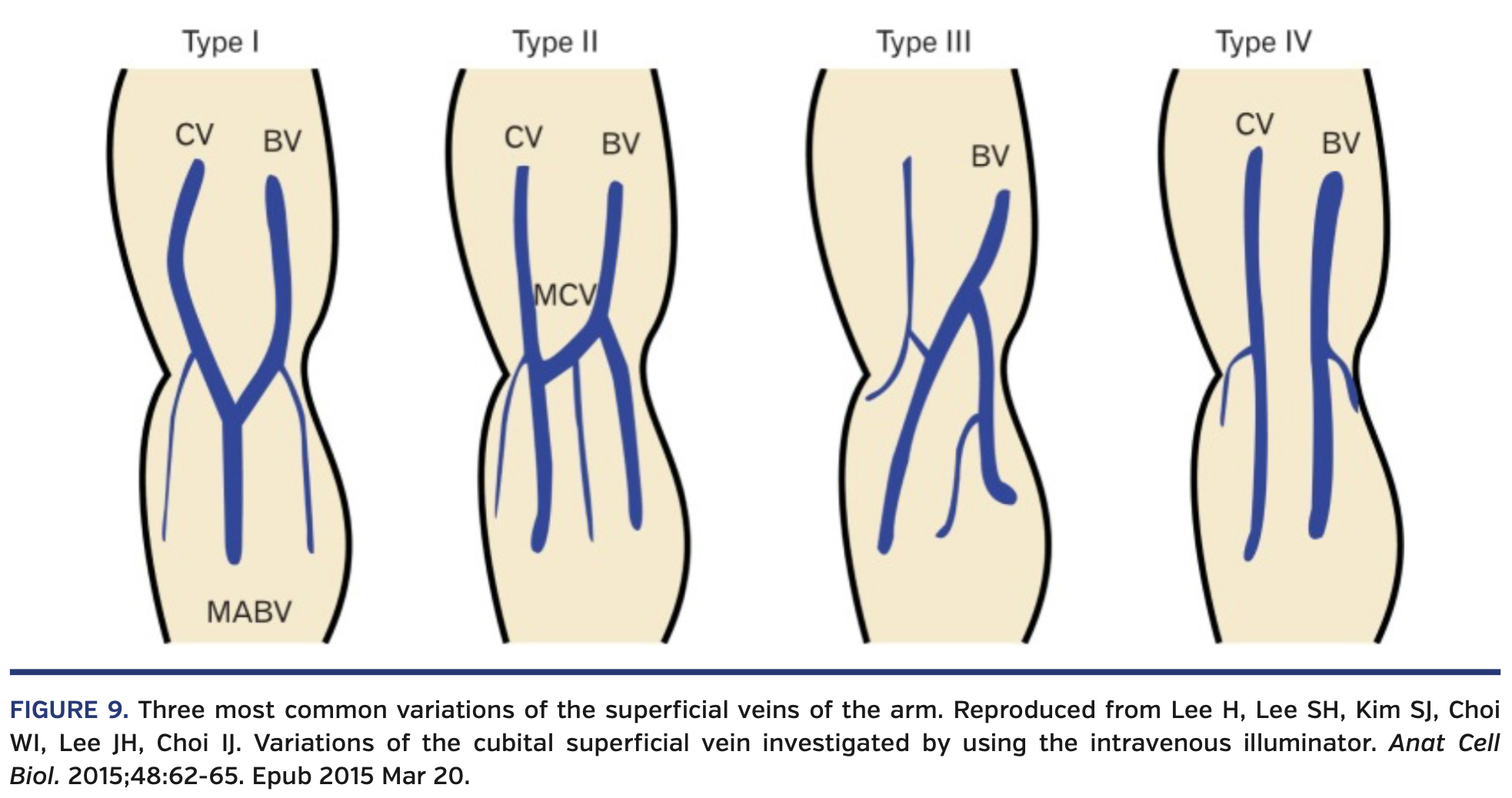
Finally, the sharp angle of the cephalic vein relative to the axillary vein and often the presence of a valve at that transition may require an 0.025˝ or 0.018˝ wire for crossing. However, there are 4 types of anatomical connection between the cephalic and basilic veins (Figure 9),4 which allow for more straightforward routes to the heart. A cephalic venogram with “roadmapping” can be performed from the access sheath with 7-8 mL of contrast if difficulties are encountered during the advancement of the catheter through the arm (Videos 3 and 4).
We present 2 cases (Videos 5 and 6) where a right heart catheterization was performed from the anatomical snuffbox through the distal cephalic vein along with a left heart catheterization from the distal radial artery. A quick right cephalic venogram was performed in both cases with 8 mL of contrast prior to catheter advancement, even though an alternative reasonable approach is to perform a venogram only when encountering difficulties.
View the Supplemental Video Series Here
15 Technical Tips
- High-quality ultrasound is needed with a high-frequency hockey stick probe.
- Check patient height and measure approximate length of the right heart catheter course.
- Ultrasound examination should be done on the table before patient preparation for planning of access sites and back-up plans.
- Place the wrist in an anatomically neutral position with slight adduction (ulnar deviation) on a rolled towel, supporting the medial aspect of the wrist joint to facilitate exposure of the vascular structures for access.
- Venous access should be done before arterial access (more technically difficult with arterial sheath in the way of ultrasound probe). Arterial access is easier and often more distal; in addition, the patient is not anticoagulated yet.
- Very gentle pressure should be applied by the ultrasound probe to minimize superficial venous collapse.
- Use a shallow angle for needle entry into the vein.
- Use slow, alternating movements of the needle tip while adjusting the ultrasound probe location and angle of examination.
- Do not pull the ultrasound probe off the skin before threading the access wire into the vein. The cephalic vein is so superficial that vein access is often lost when the probe is pulled off the skin. The access wire can be threaded without the need to hold the needle if the angle of needle entry is shallow; however, if slight resistance is encountered, an assistant can gently hold the needle hub and slightly change the angle of entry to allow for the wire to enter into the vein lumen.
- If the cephalic vein size allows, pick a sheath 1-2 Fr larger than the right heart catheter in order to reach the pulmonary capillary position. Swan-Ganz catheters are at least 1 Fr size larger on the proximal side, and one may not be able to introduce the most proximal 5-7 cm of the catheter into the sheath to reach the pulmonary capillary wedge position if the sheath size is equal to the catheter size.
- Braided, thin-walled sheaths are preferred.
- Do not aspirate from the venous sheath (the vein often collapses on the distal sheath tip).
- If the first attempt fails, try slightly more proximal after giving nitroglycerin subcutaneously at the new access site.
- If you can’t reach the pulmonary capillary wedge position, go sheathless by exchanging the catheter and sheath combination over a 0.025˝ or 0.018˝ wire for a catheter only OR use an angled, 150 cm, 4 Fr Navicross catheter through the sheath over an 0.014˝ wire and a Tuohy valve for continuous pressure assessment.
- Place the arterial hemostatic device as if the venous sheath is not there. Remove arterial sheath with the patent hemostasis technique, then remove the venous sheath. The pressure exerted by the device is often enough to result in effective venous hemostasis of the adjacent site. If oozing is seen, venous manual hold for a few minutes is recommended.
From Ascension Saint Thomas Heart, Murfreesboro and Nashville, Tennessee.
Disclosure: The author has completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. The author reports no conflicts of interest regarding the content herein.
Manuscript accepted April 21, 2020.
The author reports that patient consent was provided for publication of the images used herein.
Address for correspondence: Hady Lichaa, MD, FACC, FSCAI, FSVM, RPVI, Ascension Saint Thomas Heart, 1840 Medical Center Pkwy #201, Murfreesboro, TN 37129. Email: hady.lichaa@gmail.com or hady.lichaa@ascension.org
- Coomes EA, Haghbayan H, Cheema AN. Distal transradial access for cardiac catheterization: a systematic scoping review. Catheter Cardiovasc Interv. 2019 Nov 29 (Epub ahead of print).
- Seto A. Ultrasound guidance for upper extremity arterial and venous access. Cath Lab Digest. 2015;23(12).
- Standring S. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 41st ed. Elsevier Limited. 2016:862–894.
- Lee H, Lee SH, Kim SJ, Choi WI, Lee JH, Choi IJ. Variations of the cubital superficial vein investigated by using the intravenous illuminator. Anat Cell Biol. 2015;48:62-65. Epub 2015 Mar 20.