Clinical Impact of Medical Therapy Versus Revascularization in Patients With Chronic Coronary Total Occlusions
Abstract
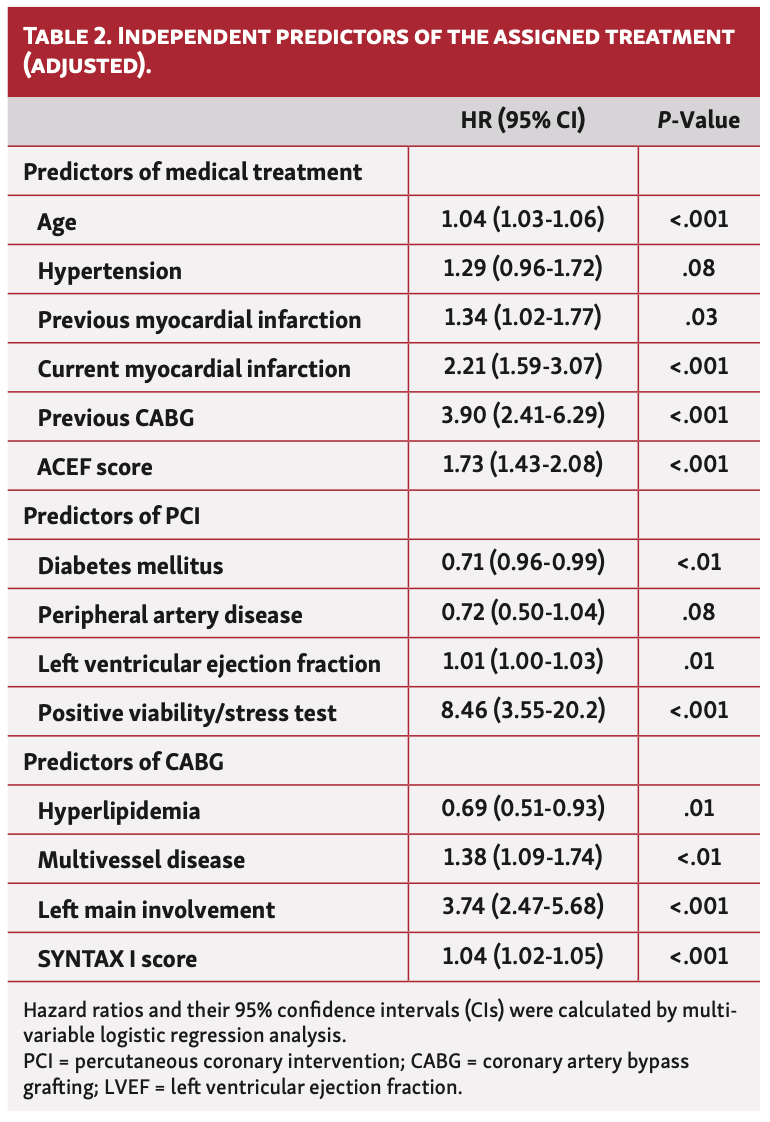
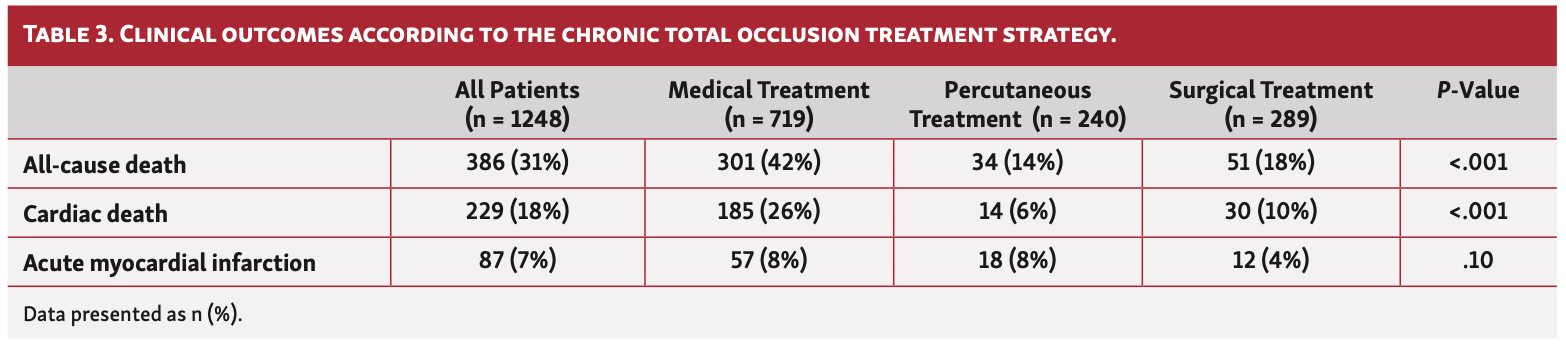
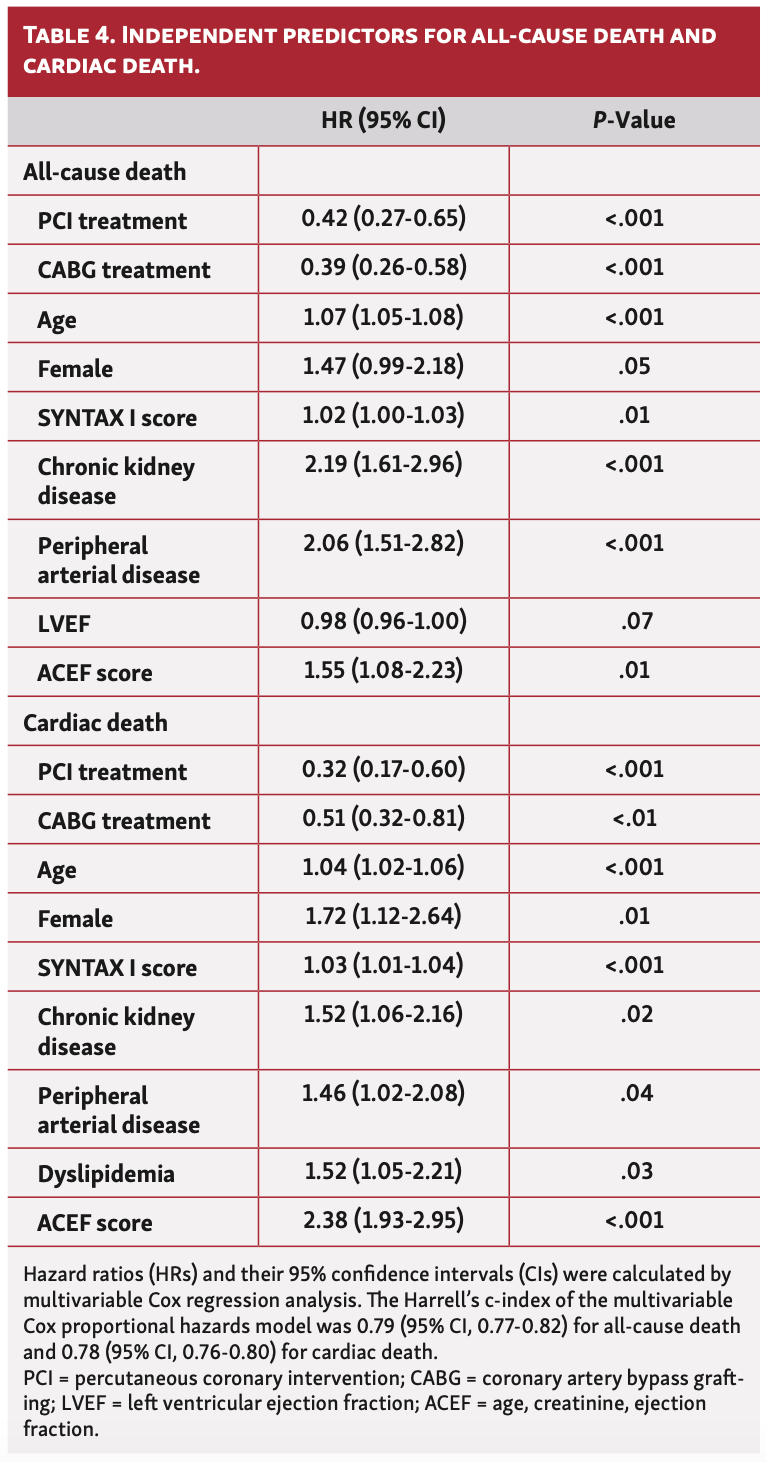
Background. Chronic total occlusions (CTOs) are prevalent angiographic findings in patients with suspected coronary artery disease. Conflicting results of randomized controlled trials and registries have not clarified the therapeutic approach for patients with CTO in clinical practice. Therefore, we sought to analyze variables influencing the decision-making process and their relationship with clinical outcomes according to the type of selected therapy. Methods. A total of 1248 consecutive patients with at least 1 CTO were identified between 2010 and 2014 at our institution. Clinical and angiographic variables were collected to allow the calculation of several predictive scores. Primary outcome was all-cause death at the longest follow-up available. Other endpoints of interest included cardiac mortality and myocardial infarction. Medical therapy (MT) alone was indicated in 719 patients (58%), whereas percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) were used in 240 (19%) and 298 (24%), respectively. Age, acute myocardial infarction, previous CABG, and age, creatinine, ejection fraction (ACEF) score were independently associated with the decision for MT alone. Conversely, the presence of multivessel disease, left main coronary artery involvement, and high SYNTAX score favored the decision for CABG. At a median follow-up of 4.3 years, revascularization strategies were independently associated with all-cause mortality and cardiac mortality (hazard ratio [HR], 0.42; 95% confidence interval [CI] 0.27-0.65; P<.001 and HR, 0.32; 95% CI, 0.17-0.60; P<.001, respectively) for PCI and (HR, 0.39; 95% CI, 0.26-0.58 and HR, 0.51; 95% CI, 0.32-0.81; P<.01, respectively) for CABG. Conclusion. Several clinical and angiographic parameters influence the decision-making process of patients with CTO. CTO revascularization with either PCI or CABG appeared to be associated with improved clinical outcomes at long-term follow-up as compared with MT alone.
J INVASIVE CARDIOL 2021;33(1):E2-E8. doi:10.25270/jic/20.00299
Key words: chronic total occlusion, clinical outcomes, revascularization
Although the evidence of a positive impact on clinical outcomes associated with chronic total occlusion (CTO) revascularization is growing, the best therapeutic approach for a CTO is still controversial. Indeed, data comparing the different treatment approaches (conservative or invasive) and their benefits in terms of long-term survival remain limited.1-3
In the “real world,” the success rate of percutaneous coronary intervention (PCI) of CTO is typically lower than observed in randomized clinical trials, in which CTO-PCI was performed by specialized operators at high-volume centers. Recently, the outcomes observed in randomized clinical trials have not favored CTO-PCI in terms of hard clinical endpoints, such as mortality, when compared with optimal medical therapy (MT) alone.4,5 On the other hand (and from the surgical point of view), CTOs are frequently not bypassed in clinical practice. This finding is directly related to completeness of revascularization and has prognostic implications in contemporary trials.6-8
The factors influencing the management of patients with CTO are poorly described, and conservative management is a common approach. To the best of our knowledge, there has not been a study that evaluated the influence of clinical, anatomical, and associated factors on the selection of the treatment strategy in patients with CTO.9,10
Therefore, we sought to analyze variables influencing the decision-making process and their relationship with clinical outcomes between the type of selected therapy (MT or revascularization) in patients with at least 1 CTO.
Methods
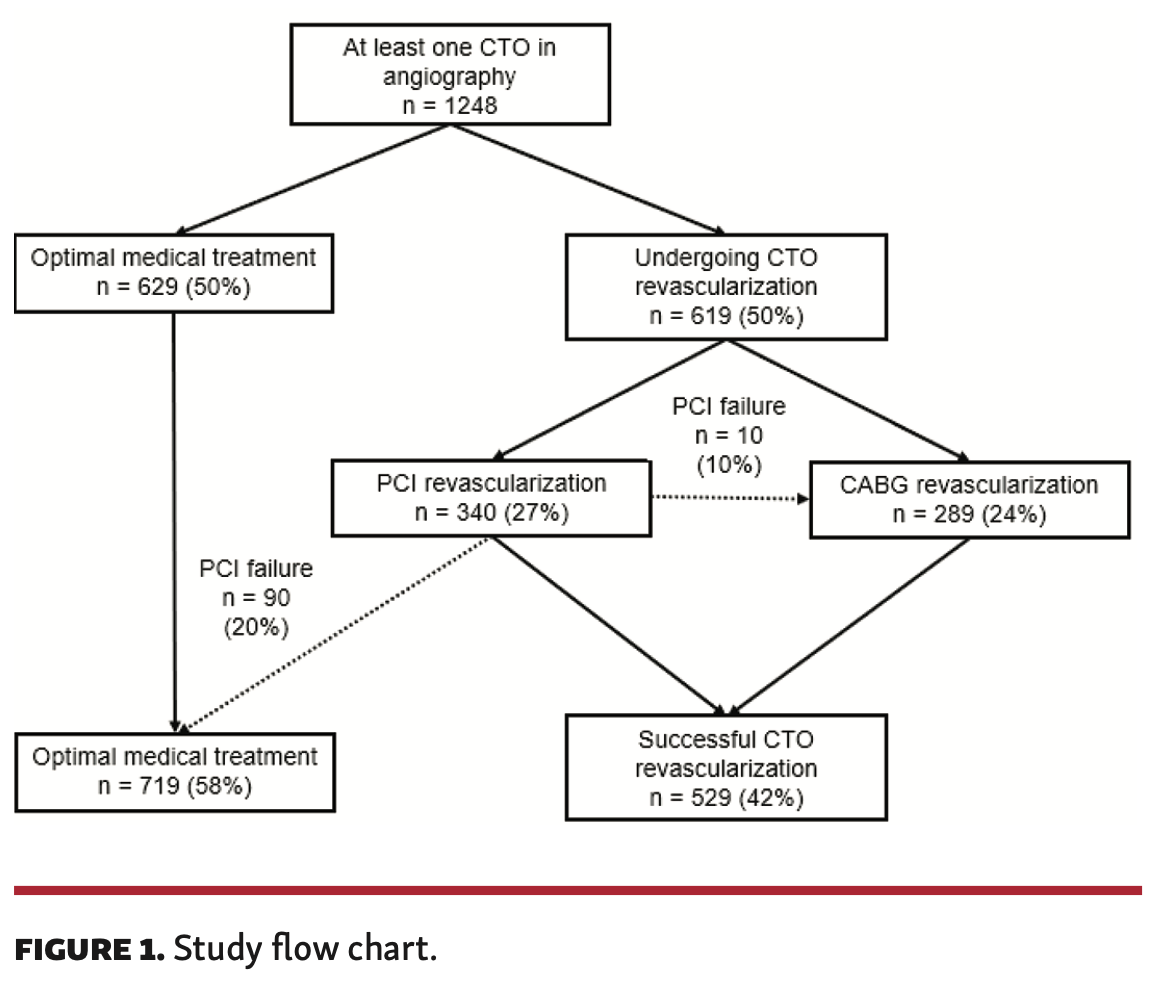
Design and study population. This single-center, observational, prospective study included all consecutive patients referred to our tertiary institution for a coronary angiogram between 2010 and 2014. The only inclusion criterion was the presence of at least 1 CTO; no exclusion criteria were considered. The choice of treatment was based on the criteria of a heart team, taking into account comorbidities and patient preference. Cardiovascular risk factors, previous ischemic cardiomyopathy, and several clinical- and angiography-related variables were recorded, including age; creatinine levels; left ventricular ejection fraction (LVEF); age, creatinine, ejection fraction (ACEF) score (age/LVEF + 1 if creatinine >2.0 mg/dL); and SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) I, II, and residual SYNTAX scores. The study flow chart is presented in Figure 1.
The follow-up protocol included a 30-day visit after hospital discharge and yearly thereafter, either on site, by review of medical records, or by telephone contact with the patient or the referring physician. The study was approved by the ethics committee at our center and complied with the principles of the Declaration of Helsinki. All patients signed informed consent for the procedures and for the research use of their anonymized data.
Study endpoints and definitions. A CTO was defined as angiographic evidence of Thrombolysis in Myocardial Infarction (TIMI) flow grade 0 within an occluded arterial segment for >3 months.11-13 In the absence of previous angiographic evidence, the duration of the occlusion was estimated clinically based on the onset of symptoms or timing of a myocardial infarction (MI) in the CTO-related artery.
CTO revascularization was performed by coronary artery bypass grafting (CABG) or by PCI. Successful CTO-PCI was defined as the recanalization of the lesion with residual stenosis levels <30% and a TIMI flow grade 3.11 CTO-PCI was performed using cutting-edge techniques such as bilateral injection, specialized hydrophilic wires, tapered tip, stiff wires, parallel wires, microcatheters, and retrograde approaches when feasible. Drug-eluting stents were implanted in all patients. Complete revascularization was defined by operators as successful treatment of all physiologically significant coronary stenosis.10,11 Following CTO-PCI, at least 12 months of clopidogrel and lifelong aspirin were prescribed to all patients. The study groups were divided according to the treatment strategy selected for the CTO: MT vs revascularization (PCI or CABG). Patients with failed PCI were reassigned to the MT group and outcomes were analyzed accordingly (Figure 1).
The primary endpoint was all-cause mortality at the longest follow-up available. Cardiac mortality was considered the main secondary endpoint. Cardiac mortality was defined according to the Academic Research Consortium-2 standards as any death due to proximate cardiac cause (MI, low-output failure, fatal arrhythmia), unwitnessed death, death of unknown cause, and all procedure-related deaths, including those related to concomitant treatment. MI was defined according to the Academic Research Consortium-2 standards for spontaneous MI, and MI related to complications of the study device (types 1, 2, 3, 4b, and 4c) proposed by the 2012 universal definition of MI.14
Statistical analysis. Continuous variables are presented as mean ± standard deviation, or as median with interquartile range (IQR). Categorical variables are presented as frequencies (percentages). The Kolmogorov-Smirnov test for a normal distribution was applied. Continuous variables were compared by the analysis of variance test and categorical variables with Pearson's Chi-squared test or Fisher's exact test, as appropriate.
We obtained hazard ratios (HRs) with associated 95% confidence intervals (CIs) from a multivariable Cox proportional hazard model developed to predict the outcomes of interest (ie, all-cause mortality and cardiac mortality). Follow-up was censored at the date of the last follow-up or at 5 years, whichever came first. Survival curves using all available follow-up data were constructed for time-to-event variables using the Kaplan-Meier methodology. All tests were 2-sided. P<.05 was considered statistically significant. Analyses were carried out using SPSS Statistics, version 19.0 (IBM).
Results
Baseline characteristics. During the study period, a total of 1248 patients (16% female) with at least 1 CTO were identified. Most patients had 1 CTO (79%), 242 patients had 2 CTOs (19%), and 15 patients had 3 CTOs (1%). CTO revascularization was initially indicated in 619 patients (50%). Failed PCI patients (n = 100) were finally treated with either CABG (n = 10) or MT (n = 90). As a result, 719 patients were finally treated with MT, 240 with PCI, and 289 with CABG. Baseline characteristics of the different study groups are presented in Table 1. The MT group was older, had a higher prevalence of hypertension and dyslipidemia, and a higher proportion of smokers. In addition, CTO was more often identified in the setting of acute coronary syndrome in the MT group vs the revascularized group (P<.05). In the revascularization group, patients in the CABG group had higher SYNTAX I score compared with the PCI-CTO group (P<.001). Also, the surgical group had higher rates of left main coronary artery disease and multivessel disease. Patients in the MT group had higher ACEF and SYNTAX II scores compared with the revascularization group.
In the revascularization group, the CTO-PCI group had higher rates of positive ischemia/viability test compared with the CABG and MT groups (51% vs 16% vs 26%, respectively; P<.001).
Predictors of the selection of therapeutic approach. Independent predictors of the therapeutic approach selected for CTO are presented in Table 2. The presence of viability/ischemia was the main independent predictor of CTO-PCI. In contrast, the presence of multivessel coronary artery disease, left main involvement, and the SYNTAX I score predicted the selection of CABG. Finally, age, ACEF score, and the history of previous CABG were independent predictors of MT.
Long-term clinical outcomes. At a median follow-up of up to 4.3 years (IQR, 2.6-4.8), patients undergoing MT had a higher rate of all-cause mortality (44% vs 18% vs 17%, respectively; P<.001) and cardiac mortality (27% vs 10% vs 10%, respectively; P<.001) compared with the PCI and CABG groups (Table 3; Figure 2).
On multivariate Cox regression analysis, CTO revascularization either by PCI or CABG was associated with lower all-cause and cardiac mortality. Other independent predictors for both cardiac and all-cause mortality in the multivariable Cox proportional hazard model included older age, SYNTAX II score, and ACEF score (Table 4).
Discussion
The main findings of our study are as follows: (1) overall, CTO patients had a poor cardiovascular profile; (2) in our cohort, only half of patients with at least 1 CTO have been revascularized; (3) stratification through different risk scores were determinant in the decision-making process of patients with CTOs; and (4) CTO revascularization was positively associated with all-cause mortality and cardiac mortality, independent of the revascularization strategy.
CTO revascularization remains a controversial topic, as randomized clinical trials are scarce and have not clarified the indication for revascularization. To date, CTO revascularization is indicated in symptomatic patients resistant to optimal MT or with a large area of documented ischemia in the territory of the CTO (class IIB).15-17 Observational studies have shown that MT is the preferred treatment for patients with at least 1 CTO, and only a minority receive CTO revascularization either by PCI or CABG. The general preference for MT over revascularization in patients with a CTO originates from concern regarding the clinical and prognostic benefits for the patient associated with CTO revascularization, a complex PCI with historically low technical success and high complication rates, and doubts about the presence of ischemia or viability in the myocardial territory subtended by the occluded artery.6-8 Older age and multiple comorbidities, such as peripheral artery disease, hypertension, dyslipidemia, chronic renal disease, and diabetes, have made the decision of CTO revascularization a real challenge. However, current techniques and new materials for CTO-PCI have significantly increased the success rate and safety of this procedure.17 Even though advanced age seems to be a limitation for any revascularization strategy, there is recent evidence demonstrating that coronary revascularization (when appropriate) compared with MT alone in patients >75 years old predicted a lower risk of all-cause mortality.10
Stratification strategies based on different risk scores could help in the decision-making process in patients with CTO lesions. In our study, the stratification through clinically and anatomically based scores identified patients in whom a conservative treatment was preferred. Also, in our cohort, higher ACEF, SYNTAX I, and SYNTAX II scores were found to be independent predictors of cardiac mortality. The ACEF score was the strongest factor associated with this outcome. Di Serafino et al11 demonstrated the ACEF score as a simple bedside tool to predict clinical outcomes in patients treated with CTO-PCI. The SYNTAX score has also been related to clinical outcomes in a CTO population. Nagashima et al demonstrated that SYNTAX score >22 predicted lower procedural success compared with patients with a SYNTAX score <22 and was an independent predictor of 30-day major adverse cardiovascular events in patients with at least 1 CTO. Shiba et al evaluated the SYNTAX II score in the revascularization selection of CTO patients with special focus on all-cause mortality and demonstrated its utility to identify patients who were treated with PCI and had a higher risk of mortality, but as in our study, the effect on long-term mortality of PCI was attenuated by comorbidities.13
We have observed that CTO-PCI was preferred in cases of a low coronary artery disease burden, where the CTO was the major determinant in the SYNTAX score calculation. Conversely, CABG was chosen in cases with extensive coronary artery disease where the CTO alone accounted for just a fraction of the overall SYNTAX score. This finding may imply that future CTO trials should not only include the angiographic evaluation of the CTO, but also a complete SYNTAX evaluation as a validated angiographic tool that is the cornerstone of decision making in the revascularization process of patients with multivessel disease.
The current evidence for CTO revascularization is controversial. Recently, 4 randomized controlled trials have evaluated the indication of PCI in CTO patients. The EXPLORE (Evaluating Xience and Left Ventricular Function in Percutaneous Coronary Intervention on Occlusions After ST-Elevation Myocardial Infarction) trial evaluated whether patients with STEMI and concurrent CTO in a non-infarct related artery benefit from additional CTO-PCI shortly after primary PCI.22 Although the trial failed to demonstrate a clear benefit of CTO-PCI with no differences in LVEF, there was a reduction in terms of angina at 12-month follow-up. The limitations on this trial included a low success rate of CTO-PCI (73%) and high crossover rate from MT to PCI (23%). The REVASC (Recovery of Left Ventricular Function in Coronary Chronic Total Occlusion) trial did not appear to improve regional or global left ventricular function in the CTO-PCI group versus the non-CTO PCI group.23 DECISION-CTO (Optimal Medical Therapy With or Without Stenting for Coronary Chronic Total Occlusion) was also a negative trial.24 This trial presented critical flaws in its design, with extremely low enrollment and a high crossover rate (19.6%) from the MT arm to the revascularization arm. In the EUROCTO trial, patients randomized to CTO-PCI (86% rate of successful PCI) had an improvement in the frequency of angina at 12 months (P<.01) and quality of life (P<.01) as assessed by the Seattle Angina Questionnaire, with no difference in the incidence of major adverse cardiovascular and cerebrovascular events.15 To date, CTO indication is limited to symptom improvement. The ongoing NOBLE-CTO trial (Nordic-Baltic Randomized Registry Study for Evaluation of PCI in Chronic Total Coronary Occlusion; NCT 03392415) and the ISCHEMIA-CTO trial (Nordic and Spanish Randomized Trial on the Effect of Revascularization or Optimal Medical Therapy of Chronic Total Coronary Occlusions with Myocardial Ischemia; NCT 03563417) will help answer this question, but are estimated to be completed in 2023 and 2028, respectively.
In our study, CTO revascularization was associated with a lower rate of all-cause mortality, irrespective of whether surgical or percutaneous coronary revascularization (PCI) was performed. In the Italian Registry of CTO, CTO-PCI was associated with lower rates of cardiac death, acute MI, and rehospitalization in comparison with MT at 1-year follow-up. On the other hand, Kim et al4 demonstrated that CABG in CTO was associated with lower rates of major adverse cardiovascular and cerebrovascular events when compared with PCI. Our findings are in keeping with those of a recent meta-analysis.26 In this pooled analysis, Christien et al observed that patients with CTO treated with MT had higher risk of all-cause mortality (relative risk, 1.99; 95% CI, 1.38-2.86; P<.001) and cardiac mortality (relative risk, 2.36; 95% CI, 1.97-2.87; P<.001) when compared with PCI.26
As previously stated, the immediate and long-term outcomes of CTO revascularization depend on a case by case scenario, where PCI or CABG should be selected using a heart team approach. Selection should be made based on the clinical background, the angiographical CTO characteristics, the expertise of the interventional team in CTO-PCI, and the evaluation of the viability of the territory subtended by the CTO. Eventually, a hybrid approach may be indicated in order to guarantee complete anatomical and functional revascularization.
Study limitations. The main limitation of this study is its observational design, which comes with an inherent selection bias. Although we observed that successful CTO revascularization was a predictor of survival in our cohort, our findings are based on registry data and the bias in treatment choice (less invasive approaches preferred in the sickest subjects) could have affected our results. Moreover, it is doubtful that a registry could capture all potential confounders, let alone control for them. Therefore, our results should be considered hypothesis generating. As a single-center study, the sample size may lack sufficient power to detect statistical differences in outcomes between PCI and CABG. The second limitation is that viability/ischemia testing was not performed in all patients. This limitation has been noted in previous reports, but it is a reflection of what occurs in the real-world clinical scenario, where the great majority of patients are referred to the catheterization laboratory without viability data available.
Conclusion
Several clinical and angiographic parameters influence the decision-making process of patients with CTO. CTO revascularization either with PCI or CABG appeared to be associated with improved clinical outcomes at long-term follow-up as compared with MT alone.
*Joint first authors.
From the 1Cardiology Department, Clinic Cardiovascular Institute, Hospital Clínic, IDIBAPS, Barcelona, Spain; 2Cardiology Department, Vall d'hebron Hospital, Barcelona, and CIBER de
Epidemiología y Salud Pública (CIBERESP), Spain; and 3Service de Cardiologie, Centre Hospital-ier de Saintonge, Saintes, France.
Disclosure: The authors have completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Sabate reports consultant fees from Abbott Vascular and IVascular.
The remaining authors report no conflicts of interest regarding the content herein.
Final version accepted May 18, 2020.
Address for correspondence: Manel Sabaté, MD, PhD, Hospital Clínic; C/Villarroel, 170, Cardiology Department, 08036 Barcelona, Spain. Email: masabate@clinic.cat
- Galassi A, Wener G, Boukhris M, et al. Percutaneous recanalization of chronic total occlusions: 2019 consensus document from the EuroCTO Club. EuroIntervention. 2019;15:198-208.
- Ladwiniec A, Allgar V, Thackray S, Alamgir F, Hoye A. Medical therapy, percutaneous coronary intervention and prognosis in patients with chronic total occlusions. Heart. 2015;101:1907-1914.
- Tomasello SD, Bourkhirs M, Giubilato S, et al. Management strategies in patients affected by chronic total occlusions: results from the Italian Registry of Chronic Total Occlusions. Eur Heart J. 2015;36:3189-3198.
- Kim BS, Yang JH, Jang WJ, et al. Clinical outcomes of multiple chronic total occlusions in coronary arteries according to three therapeutic strategies: bypass surgery, percutaneous coronary intervention and medication. Int J Cardiol. 2015;197:2-7.
- Holmes DR Jr, Barsness GW. Percutaneous coronary intervention for chronic total occlusions. Circ Cardiovasc Interv. 2019;12:e008321.
- Farooq V, Serruys PW, García-Garcia HM, et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX trial. J Am Coll Cardiol. 2013;61:282-294.
- Généreux P, Palmerini T, Caixeta A, et al. Quantification and impact of untreated coronary artery disease after percutaneous coronary intervention: the residual SYNTAX (Synergy Between PCI with Taxus and Cardiac Surgery) score. J Am Coll Cardiol. 2012;59:2165-2174.
- Farooq V, Serruys PW, Bourantas CV, et al. Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation. 2013;128:141-151.
- Azzalini L, Jolicoeur M, Pighi M, et al. Epidemiology, management strategies, and outcomes of patients with chronic total coronary occlusion. Am J Cardiol. 2016;118:1128-1135.
- Flores-Umanzor EJ, Vazquez S, Cepas-Guillen P, et al. Impact of revascularization versus medial therapy alone for chronic total occlusion management in older patients. Catheter Cardiovasc Interv. 2019;94:527-535.
- Di Serafino L, Borgia F, Maeremans J, et al. The age, creatinine, and ejection fraction score to risk stratify patients who underwent percutaneous coronary intervention of coronary chronic total occlusion. Am J Cardiol. 2014:114:1158-1164.
- Nagashima Y, Lijima R, Nakamura M, Sugi K. Utility of the SYNTAX score in predicting outcomes after coronary intervention for chronic total occlusion. Herz. 2015;40:1090-1096.
- Shiba M, Minakawa M, Nakamura M. Syntax-score II based assessment of percutaneous coronary intervention for patients with chronic total occlusion. Circulation. 2017;136:A20204.
- Garcia-Garcia HM, McFadden EP, Farb A, et al. Standardized end point definitions for coronary intervention trials: the Academic Research Consortium-2 consensus document. Circulation. 2018;137:2635-2650.
- Werner GW, Martin-Yuste V, Hildick-Smith D, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 2018;39:2484-2493.
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165.
- Flores-Umanzor EJ, Cepas-Guillen PL, Vázquez S, et al. Survival benefit of revascularization versus optimal medical therapy alone for chronic total occlusion management in patients with diabetes. Catheter Cardiovasc Interv. Epub 2020 Feb 25.
- Carlino M, Magri CJ, Uretsky BF, et al. Treatment of the chronic total occlusion: a call to action for the interventional community. Catheter Cardiovasc Interv. 2015;85:771-778.
- Fefer P, Knudtson ML, Cheema AN, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012;59:991-997.
- Redfors B, Palmerini T, Caixeta A, et al. Impact of chronic total occlusions on revascularization scores and outcome prediction. J Invasive Cardiol. 2017;29:123-131.
- Tajti P, Burke MN, Karmpaliotis D, et al. Update in the percutaneous management of coronary chronic total occlusions. JACC Cardiovasc Interv. 2018;11:615-625.
- Henriques JP, Hombres LP, Ramunddal T, et al. Percutaneous intervention for concurrent chronic total occlusions in patients with STEMI: the EXPLORE trial. J Am Coll Cardiol. 2016;68:1622-1632.
- Mashayekhi K, Nührenberg TG, Toma A, et al. A randomized trial to assess regional left ventricular function after stent implantation in chronic total occlusion: the REVASC trial. JACC Cardiovasc Interv. 2018;11:1982-1991.
- Lee SW, Lee PH, Ahn JM, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion. Circulation. 2019;139:1674-1683.
- Marecharl P, Davin L, Gach O, et al. Coronary chronic total occlusion intervention: utility or futility. Expert Rev Cardiovasc Ther. 2018;16:361-367.
- Christien KH, Gabriel Wong KH, Gong M, et al. Percutaneous coronary intervention versus medical therapy for chronic total occlusion of coronary arteries: a systematic review and meta-analysis. Current Atheroscler Rep. 2019;21:42.