Will Renal Denervation Have an Important Role in the Treatment of Hypertension?
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Vascular Disease Management or HMP Global, their employees, and affiliates.

Piedmont Heart Institute, Atlanta, Georgia
David E. Kandzari, MD, FACC, MSCAI, chief of Piedmont Heart Institute and Cardiovascular Services, director of interventional cardiology at the Piedmont Heart Institute, and chief scientific officer of the Piedmont Heart Institute, gave a presentation on Monday morning at ISET 2025, where he examined renal denervation (RDN) as a potential new standard in hypertension treatment. The talk covered the evolution of antihypertensive therapies, clinical evidence supporting RDN, and future considerations for integrating this technology into patient care.
Dr. Kandzari began his presentation reviewing the current landscape of hypertension treatment, noting that nearly half of U.S. adults (119.9 million) have hypertension, but only 22.5% have controlled blood pressure (BP) (<130/80 mmHg). Medication adherence remains a significant challenge, leading to suboptimal long-term BP control despite pharmacologic therapy. Recent trials suggest that drug-based hypertension management has limitations, with a mean systolic BP reduction of only 5.1 mmHg over time.
RDN is a catheter-based procedure that disrupts renal sympathetic nerves, reducing BP by limiting sympathetic outflow. Multiple sham-controlled randomized trials (RCTs) have confirmed the effectiveness of RDN, both with and without antihypertensive medications. RDN provides continuous BP reduction, avoiding issues of patient non-compliance with medications.
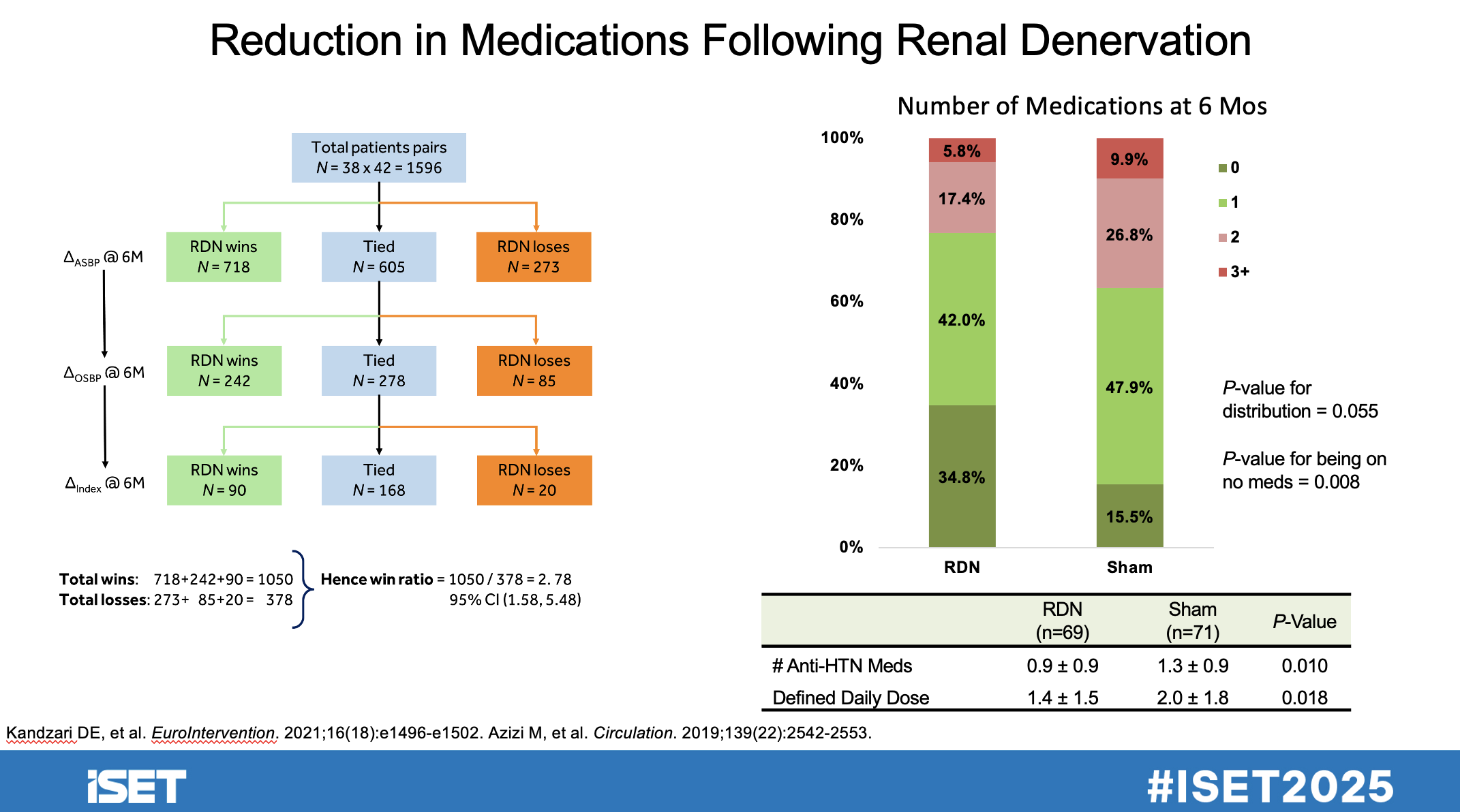
Key findings from RCTs and meta-analyses include sustained BP reduction over time, including long-term follow-up studies spanning more than 3 years. A reduction in medication burden was seen; patients required fewer antihypertensive drugs post-RDN. No evidence of significant rebound hypertension post-procedure.
Dr Kandzari emphasized that RDN has shown excellent safety profiles across multiple studies including a significant decline in renal function (eGFR remained stable) and very low rates of renal artery reintervention (0.20% per year). Cost-effectiveness modeling suggests RDN is a high-value treatment and is projected to reduce the risk of stroke (20%), myocardial infarction (12%), and heart failure (28%) over 10 years. RDN added 0.36 quality-adjusted life years (QALYs) with an incremental cost-effectiveness ratio (ICER) of $15,923 per QALY gained, which is well below standard cost-effectiveness thresholds.
The presentation concluded with a review of the key challenges for widespread adoption: a need for greater physician education and training in RDN procedures, reimbursement and cost considerations compared to standard antihypertensive medications, and the need for expanded patient selection criteria to maximize benefit. Future research areas include identifying which patient subgroups benefit most from RDN, exploring new anatomical targets for sympathetic denervation, and further integrating RDN into hypertension guidelines. RDN is a promising alternative to medication for long-term hypertension control, particularly in patients with poor medication adherence.













