The Roundabout Way to Save a Foot: Utilization of Pedal Access for Limb Salvage
Peripheral arterial disease (PAD) affects more than 12 million patients in the United States and more than 200 million patients worldwide.1 Current PAD management, including antiplatelet agents, statins, smoking cessation, and supervised exercise programs, aims to improve the patient’s quality of life and prevent the cardiovascular comorbidities associated with vascular disease.2 These therapies are reported to improve the maximum walking distance and to reduce limb loss, consequently resulting in better quality of life.3-7 Percutaneous vascular interventions (PVIs), on the other hand, are often needed in patients whose symptoms are refractory to conservative management or in those who develop critical limb ischemia and have the goal of limb salvage, potentially obviating the need for amputation. However, in the face of severe peripheral vascular disease and chronic total occlusions, crossing infragenicular lesions via the standard antegrade approach alone may prove exceptionally difficult. More than 2 decades ago, the inability to cross below-knee lesions in an antegrade fashion was considered as a failure of percutaneous intervention, indicating the need for a surgical approach. Iyer et al reported their first cases about the utilization of a retrograde pedal/tibial approach when the traditional antegrade method had failed in crossing the tibial lesions.8
In our case, we highlight the importance of combining the antegrade and retrograde approaches in order to achieve optimal revascularization in this form of severe infragenicular arterial disease.
Case Presentation
A 62-year-old woman with a history of hypertension, diabetes mellitus, chronic kidney disease, and non-ischemic cardiomyopathy with an ejection fraction status of 15% to 20% after automatic implantable cardioverter-defibrillator (AICD) placement was admitted to our center for management of right fifth digit gangrene. The patient also had severe peripheral arterial disease. The patient was evaluated by our interventional cardiology team, in conjunction with the podiatry and vascular surgery teams, who agreed that she might benefit from percutaneous vascular intervention to allow better tissue healing and possibly avoid the need for foot amputation. The patient had recently undergone percutaneous transluminal angioplasty (PTA) of the right posterior tibial artery, which was completely occluded proximally in the setting of a poorly healing heel ulcer.
Four weeks later, the patient returned for planned percutaneous transluminal angioplasty of the right anterior tibial artery (ATA).
Procedure Details
Left antegrade femoral arterial access was obtained. After performing angiography (Figure 1), a 0.018 gold-tip wire was advanced via antegrade approach to the proximal end of the occluded ATA (Figure 2). Multiple attempts were made at antegrade crossing, which led to subintimal crossing and inability to re-enter the true lumen. Subsequently, retrograde pedal access (via the dorsalis pedis artery) was obtained under fluoroscopic guidance (using roadmap technique) with placement of 4/5 FR Slender sheath (Figure 3). 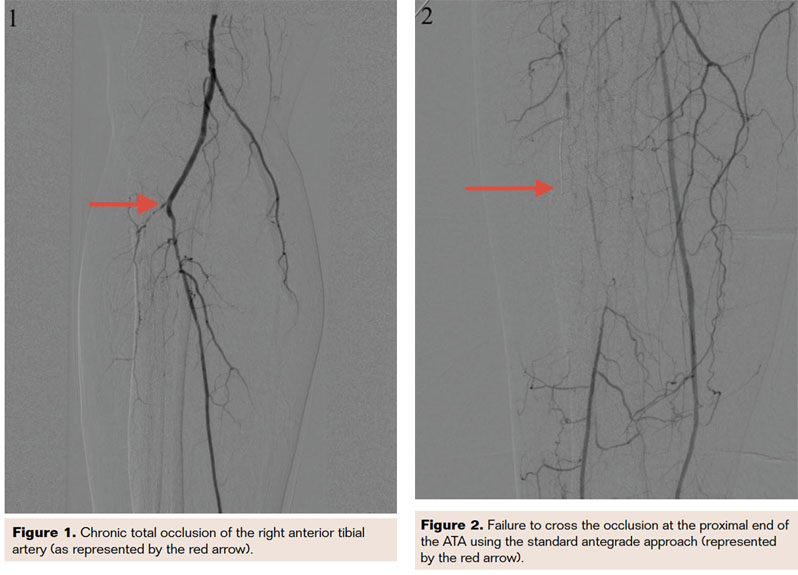

In a retrograde fashion, a 0.014-inch Runthrough wire was advanced in combination with a micro 14 support catheter, which was advanced to the proximal cap of the ATA occlusion and used as a reference (Figure 4). Under guidance of the retrograde wire, the antegrade wire was advanced in the appropriate direction, leading to intraluminal crossing (Figure 5), as confirmed by intravascular ultrasound (IVUS). Balloon angioplasty was then performed using a 2.0 × 150 mm NanoCross balloon with single inflation at 10 atm, followed by laser atherectomy and subsequent low-pressure inflation of the proximal ATA using the same balloon. Final angiograms revealed excellent antegrade flow through the tibioperoneal trunk, ATA, and PTA with 2.5 run-off to the foot (Figures 6 and 7).  The patient was discharged home the next morning on guideline-directed medical therapy for PAD in stable condition. The patient subsequently had the toe amputated; however, given her revascularization, the foot was salvaged and is currently doing well.
The patient was discharged home the next morning on guideline-directed medical therapy for PAD in stable condition. The patient subsequently had the toe amputated; however, given her revascularization, the foot was salvaged and is currently doing well.
Discussion
Critical limb ischemia (CLI) and chronic total occlusions (CTO) are associated with extensive morbidity and pose a significant challenge for interventionists, often leading to an excessive number of patients undergoing amputation. Consequently, techniques aimed at facilitating crossing of complex lesions that are not amenable to the standard antegrade approach, and thereby potentially impeding or altogether preventing the need for amputation, have piqued the interest of the medical community.

In a retrospective review of prospectively collected institutional data of 430 patients with CLI undergoing peripheral vascular intervention (PVI), patients treated with retrograde access were more likely to have a history of recent (< 5 years) coronary artery bypass graft, trended more towards advanced age, and were more likely to have had prior PVI.9 Interestingly, retrograde access was successful in 90.5% of cases, without any instances of perforation, distal embolization, or loss of distal target.8 In the group that received PVI via retrograde access, follow-up data revealed freedom from re-intervention (either by PVI or surgical bypass) was 68.6% at 6 months and 1 year.9 Moreover, freedom from amputation at 6 months and 1 year was 86.2% and 78.3%, respectively. This case, as supported by the literature, shows the importance of using the retrograde approach when possible, along with the antegrade approach, for patients with multiple comorbidities who are otherwise deemed as too high-risk to undergo surgical revascularization.
Conclusion
In this case, retrograde arterial access of the arteries of the lower extremities (popliteal, tibial, and pedal) enabled limb salvage in a complex lesion, thereby salvaging the foot and limiting the extent of amputation.
Disclosure: The authors have completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors report no conflicts of interest regarding the content herein.
Manuscript submitted August 11, 2017; final version accepted September 5, 2017.
Address for correspondence: Anwar Zaitoun, MD; Saint John Hospital and Medical Center, 22101 Moross, Detroit, MI, 48236. Email: anzaitoun@gmail.com
References
1. American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care 2003;26:3333–41.
2. Rooke TW, Hirsch AT, Misra S, et al. Management of Patients with Peripheral Artery Disease (Compilation of 2005 and 2011 ACCF/AHA Guideline Recommendations). A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(14):1555-1570.
3. Murphy TP, Cutlip DE, Regensteiner JG, et al. Supervised exercise versus primary stenting for claudication resulting from aortoiliac peripheral artery disease: six-month outcomes from the Claudication: Exercise Versus Endoluminal Revascularization (CLEVER) study. Circulation. 2012;125:130-139.
4. Nordanstig J, Taft C, Hensäter M, et al. Improved Quality of Life After One Year With an Invasive Versus a Non-Invasive Treatment Strategy in Claudicants: One Year Results of the IRONIC Trial. Circulation. 2014;CIRCULATIONAHA.114.009867
5. Safley DM, House JA, Laster SB, et al. Quantifying improvement in symptoms, functioning, and quality of life after peripheral endovascular revascularization. Circulation. 2007;115: 569-575.
6. Bradbury AW, Adam DJ, Bell J, et al. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: An intention-to-treat analysis of amputation-free and overall survival in patients randomized to a bypass surgery-first or a balloon angioplasty-first revascularization strategy. J Vasc Surg. 2010;51(5 Suppl):5S–17S.
7. Fakhry F, Spronk S, van der Laan L, et al. Endovascular revascularization and supervised exercise for peripheral artery disease and intermittent claudication: a randomized clinical trial. JAMA. 2015;314:1936-1944.
8. Iyer SS, Dorros G, Zaitoun R, Lewin RF. Retrograde recanalization of an occluded posterior tibial artery by using a posterior tibial cutdown: two case reports. Cathet Cardiovasc Diagn. 1990;20(4):251–253.
9. Cafasso D, Stern J, Connolly P, et al. Safety and Effectiveness of Retrograde Arterial Access for Endovascular Treatment of Critical Limb Ischemia (CLI). Annals of Vascular Surgery. 2017;41:18.












