Infection of a Common Iliac Artery Covered Stent, Implanted for an Ureteroiliac Artery Fistula
A rare but nonetheless important cause of recurrent gross hematuria is an ureteroarterial fistula.1 The diagnosis requires a high index of suspicion and, for this reason, management can easily be delayed, which can endanger a patient’s life.2 Since first reported in 1996, stent graft placement for these fistulas has become popular, with no deaths reported in a recent review of 32 cases.2,3
We present the clinical course of a patient with an ureteroiliac artery fistula who had been managed by iliac stenting for 2 years prior to presentation. The patient presented with stent thrombosis, infection, and refistulization as late complications.
Clinical Presentation
A 63-year-old man was sent to our department in August 2015 for evaluation of short-distance intermittent claudication of his left leg of several weeks duration. Physical examination results showed an ischemic left lower extremity with absent femoral, popliteal, and distal pulses. The patient’s right lower extremity had a good quality femoral pulse without popliteal and distal pulses.
Past surgical history included bladder cancer with cystoprostatectomy and Bricker operation in December 2009. Several months later, the patient had bilateral ureteral stenosis that could not resolve endourologically. An unsuccessful open bilateral ureter reimplantation was done in October 2010. As a result, the patient had a right percutaneous nephrostomy and a left ureteral catheter.
In July 2013, during a routine ureteral catheter replacement, the patient presented with an exsanguinating ureteral hemorrhage, and ureteroiliac fistula was diagnosed. He was treated via percutaneous insertion of a covered common iliac stent. Recovery was uneventful, and the patient was discharged without any additional complications.
Two years later, the patient underwent computed tomography (CT) to evaluate his ischemic left leg and to facilitate definitive operative planning. CT results revealed thrombosis of his common iliac stent, with an air bubble inside, and a perivascular hematoma involving the left common iliac artery and left ureter. 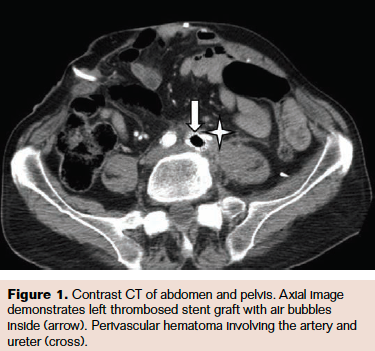
While preparations were underway for surgical intervention for stent explantation, the patient was scheduled for another routine ureteral catheter exchange. At that time, a several-day history of intermittent hematuria from his indwelling left ureteral catheter was documented. For this reason, the patient was transferred to our vascular surgery service. On arrival, he was greatly debilitated and afebrile, with dehydration and mild tachycardia. He was anemic, with hemoglobin of 6.9 g/dL, necessitating transfusion of 2 units of blood. Our infectious disease service initiated broad-spectrum antibiotic therapy with ertapenem. A new CT scan was ordered but did not show significant changes from the previous scan.
The patient was taken to the operating room. With the patient in the supine position, the right common femoral artery was punctured, and a guidewire was inserted via a 6F introducer sheath in order to have distal aortic control in the event a surgical accident occurred. A left retroperitoneal incision was performed to gain aortic and iliac axis control. The artery had a large orifice through which the covered stent was clearly visible. It was explanted without any difficulty, and the common iliac artery stump was sutured with 4/0 Prolene. We performed an angiogram via the right femoral artery sheath to confirm the correct sealing of the suture. A moderate right common iliac artery stenosis was observed, and simple angioplasty was performed, with satisfactory result.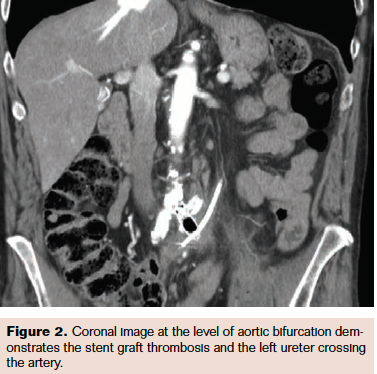
Following treatment, the patient´s hematuria ceased, the incision healed without complication, and his hemoglobin stabilized to around 10 g/dL (reference range, 12-15 g/dL) without need for any further transfusion. Serum creatinine trended down to baseline over the following week. During the postoperative course there was a urinary infection that was treated with carbapenem for 7 days, as well as a prosthesis infection by Pseudomonas that was treated with carbapenem and piperacillin/tazobactam. After consultation with the infectious diseases service, the decision was made to continue intravenous antibiotics for a total treatment duration of 3 weeks. Upon completion of the antibiotics course, the patient’s white blood cell count normalized.
The patient has since returned to interventional radiology for bimonthly percutaneous nephrostomy tube exchanges, and he denies any hematuria recurrence. His left-leg claudication has stabilized, and we have decided to pursue conservative treatment before a crossover femorofemoral bypass is performed.
Discussion
Ureteroarterial fistula is an infrequent cause of potentially life-threatening hematuria. The occurrence of this pathologic entity is unknown, but just over 100 cases have been reported to date.4 Before 1980, the mortality for ureteroarterial fistula was 60%, but it fell to 7.1% thereafter1 and has been attributed to a delay in diagnosis and treatment.5 Ureteroarterial fistula predominantly affect women (72%), with a wide time range between the initial operative insult to the ureter and fistulization, ranging from 2 to 25 years in several reports.6
Ureteroarterial fistula are the consequence of chronic inflammatory events that create a fibrous and poorly vascularized uretero-vascular adhesion.5 They can be classified according to cause: iatrogenic, primary, and pregnancy-related. Iatrogenic causes account for 85% of all ureteroarterial fistulas and are related to radiotherapy, pelvic surgery for malignancy, and vascular surgery with grafting.
There is no gold standard for the management of ureteroarterial fistulas. Currently, the ideal treatment for ureteroarterial fistula is controversial and has changed with the advent of covered stents.7 Percutaneous endovascular stenting is a new and attractive treatment option that has the advantage of being a less invasive, more rapid, and simpler approach.
The main limitations to endovascular treatment are that the long-term patency of stents is unknown, and there is a possibility of graft infection.8 The case presented here illustrates these 2 issues, ie, stent thrombosis and a newly developed infectious ureteroarterial fistula after long-term stent implantation. Fox et al reported a success rate of 85% in the endovascular treatment of 14 patients,9 and van den Bergh et al reported no deaths after endovascular treatment in their systematic review of 32 cases.10 The median follow-up in these studies was only 4.5 months.
In a review by Krambeck et al, 2 of 3 patients required secondary treatment as a result of graft occlusion and continued hemorrhage, and one of the patients developed chronic lower limb edema and pain on the side of the occluded graft.11
The largest systematic review was published by Bergqvist et al and analyzed 80 patients in 77 reports that spanned 7 decades.1 Since most surgeons have treated isolated cases, treatment algorithms have not yet been defined. Okada et al, in the largest single-institution series published, evaluated the safety, efficacy, and long-term results of endovascular stent graft placement in 11 patients with ureteroarterial fistula with a mean follow-up of 548 days.3 Thirty-six percent of patients had recurrent hematuria, and 2 patients underwent additional treatment with secondary stent graft placement and surgical reconstruction. There were no stent-graft–related complications such as thrombosis, kinking, or migration, and all stent grafts were patent. However, the duration of the follow-up period may not be sufficient to detect this complication, as the most severe complications appear beyond the second year of implantation.
Our patient presented with a secondary ureteroarterial fistula and a thrombosed iliac covered stent 2 years after implantation. This long follow-up period provides important insights about this endovascular treatment and opportunity for treatment if stent graft infection, patency complications, or new fistulas appear.
Conclusion
Ureteroiliac fistulas are increasing in frequency due to the more liberal use of catheters for ureteral obstruction, extensive urologic surgery, and radiotherapy. An early diagnosis plays a crucial role in treatment. Endovascular treatment holds apparent advantages over open surgery in this emergent life-saving situation. Endovascular treatment occludes the fistula while maintaining blood flow in the affected vessels, does not put the ureter at any increased risk, and allows treatment to occur more expeditiously. As in other fields of vascular surgery that encounter potentially infected pathology (eg, aortoenteric fistulae, mycotic aneurysms, and others), endovascular stent-graft implantation should be contemplated as a possible bridge procedure. In this sense, long-term follow-up and a high index of suspicion are essential to address severe complications as soon as they appear. In these cases, open surgery with explantation of all prosthetic material is mandatory, with or without revascularization via alternative fields, depending on the patient’s condition.
Disclosure: The authors have completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors report no conflicts of interest regarding the content herein.
Manuscript submitted August 8, 2017; accepted October 16, 2017.
Sandra Vicente, M.D, PhD; Department of Angiology, Vascular and Endovascular Surgery, Alcorcon Fundation Hospital, 1 Budapest Street, Alcorcón, Madrid, Spain 28922. Email: sandravj1984@gmail.com
References
1. Bergqvist D; Pärsson H; Sherif A. Arterio-ureteral fistula — a systematic review. Eur J Vasc Endovasc Surg. 2001;22(3):191-196.
2. Muradi A, Yamaguchi M, Idoguchi K, et al. Lessons learned from endovascular management of ureteroarterial fistula. Vasc and Endovasc Surg. 2014;48(2):159-161.
3. Okada T, Yamaguchi M, Muradi A, et al. Long-term results of endovascular stent graft placement of ureteroarterial fistula. Cardiovasc Intervent Radiol. 2013;36(4):950-956.
4. Tselikas L, Pellerin O, Di Primio M, et al. Uretero-iliac fistula: modern treatment via endovascular route. Diagn Interv Imaging. 2013;94(3):311-318.
5. Yamasaki K, Omori K, Takaoka E, et al. Successful management by provocative angiography and endovascular stent of ureteroarterial fistula in a patient with a long-term indwelling ureteral stent. Jpn J Clin Oncol. 2010;40(3):267-270.
6. Malgor R, Oderich G, Andrews J, et al. Evolution from open surgical to endovascular treatment of ureteral-iliac artery fistula. J Vasc Surg. 2012;55(4):1072-1080.
7. Darcy M. Uretero-arterial fistulas. Tech Vasc Interv Radiol. 2009;12(3):216-221.
8. Copelan A, Chehab M, Cash C, Korman H, Dixit P. Endovascular management of ureteroarterial fistula: a rare potentially life threatening cause of hematuria. J Radiol Case Rep. 2014;8(7):37-45.
9. Fox JA, Krambeck A, McPhail EF, Lightner D. Ureteroarterial fistula treatment with open surgery versus endovascular management: long-term outcomes. J Urol. 2011;185(3):945-950.
10. Van der Bergh RC, Moll FL, de Vries JP, Lock TM. Arterioureteral fistulas: unusual suspects—systematic review of 139 cases. Urology. 2009;74(2):251-255.
11. Krambeck A, Dimarco D, Gettman M, Segura J. Ureteroiliac artery fistula: diagnosis and treatment algorithm. Urology. 2005;66(5):990-994.












