One Last Inflation: A Difficult Case of a Patient With Symptomatic Carotid Artery Stenosis
Abstract
An 88-year-old woman presented with symptomatic right carotid artery disease. Due to significant atherosclerotic disease, we were unable to advance a self-expanding carotid stent past the lesion, even after multiple attempts of predilation with an appropriately sized balloon. Ultimately, only after predilation with an oversized balloon, we were able to pass and deploy the stent and perform successful postdilation. This case illustrates the potential for complications when facing severely fibrotic lesions in carotid catheterization as well as potential options for future operators.
VASCULAR DISEASE MANAGEMENT. 2022;19(8):E129-E130
Key words: angioplasty, calcification, carotid artery stenosis, stenting
Background
Carotid artery calcification is an inflammatory process associated with an increased risk of stroke proportional to the degree of stenosis.1 Carotid artery stenting has been demonstrated in multiple trials to possess noninferiority to carotid endarterectomy in both short- and long-term outcomes.2-4 However, severely calcified lesions that may be nondilatable present difficulties in obtaining carotid access. We present a case of predilating a large symptomatic carotid plaque using an oversized balloon to perform stenting with excellent patient outcomes.
Case Report
An 88-year-old woman was initially referred for significant aortic stenosis with a valve area under 1 cm2 with symptoms of dyspnea on exertion with maintained left ventricular function. Furthermore, she had presented with intermittent numbness of her left arm and leg over the previous month. A preprocedure heart catheterization and carotid angiogram delineated the significance of right internal carotid stenosis of 80%, the absence of significant coronary disease, and the presence of significant aortic stenosis.
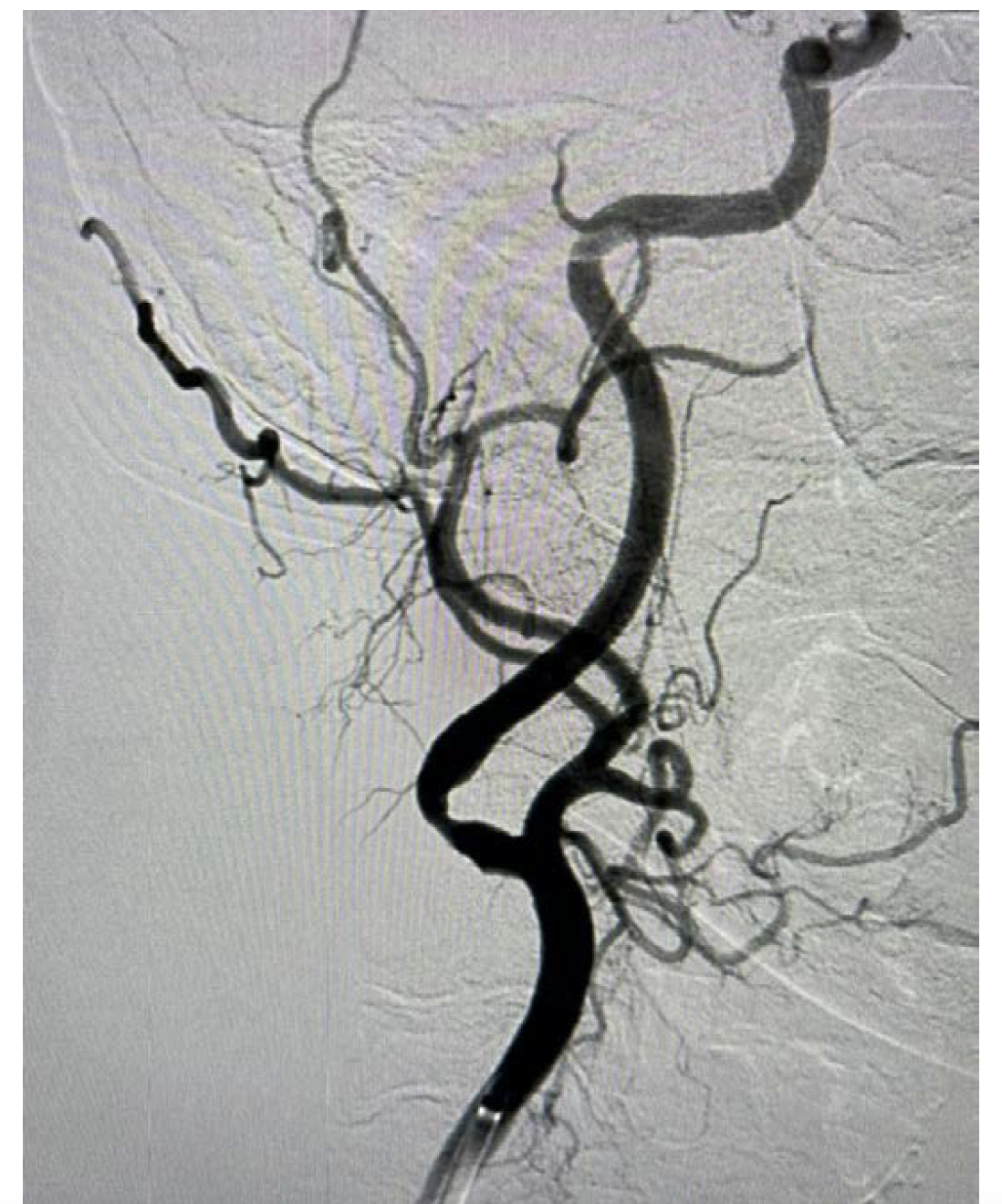

The patient underwent elective carotid stenting as a staged procedure prior to transcatheter aortic valve replacement (TAVR). Her previous diagnostic study utilized right radial artery access but it was difficult to perform selective carotid angiography, specifically that of the left carotid artery.5 Consequently, this intervention was performed from the right groin. A VTK catheter (Cook Medical) was placed in the right common carotid artery, followed by a TAD guidewire (Abbott Vascular) and then a Flexor Shuttle sheath (Cook Medical) with no difficulty. There was no difficulty deploying a large filter wire (NAV RX 7.2 mm, Abbott Vascular), and we were able to dilate with a 4-mm x 15-mm balloon (Abbott Vascular). However, we could not pass a 6/8 self-expanding stent (Abbott) (Figure 1). We performed further predilation with a 6-mm x 15-mm balloon, but we were still not able to pass the 6/8 stent. Because we had already performed adequate predilation, we attempted to pass a 2-cm self-expanding stent (Abbott Vascular) but were still unable to cross the lesion. Finally, we performed predilation balloon angioplasty with a 7-mm x 15-mm balloon (Abbott Vascular), which ultimately allowed us to pass the 6/8 self-expanding stent. After deployment, we removed the filter and a subsequent arteriogram confirmed that the lesion had completely resolved (Figure 2). The patient had no hypotension or bradycardia during the procedure and was discharged the following day. She will undergo TAVR at a later date. This case exemplifies using stepwise predilation of a severely calcified carotid lesion, demonstrating an option for operators.
Discussion
The risks of attempting carotid artery stenting in highly calcified lesions include balloon rupture during predilation. However, this has been demonstrated to be a rare as well as relatively benign event, although it carries the theoretical risk of causing cerebral embolism.6 More common is the possibility of causing intimal tears, although the data show the majority can be conservatively managed without significant consequences.7 As such, the risks must be balanced against the potential long-term sequelae of not performing the procedure.
Currently, there are several technologies available for the treatment of calcific carotid lesions, including focused balloons such as the AngioScore (Philips) as well as noncompliant balloons from Medtronic. Additional tools exist for coronary lesions including scoring balloons such as AngioSculpt (Philips) and lithotripsy systems such as intravascular lithotripsy (Shockwave). In this case, none of these options were available if the 7-mm balloon had not dilated the lesion enough to pass the stent, since these balloons do not come in larger sizes. Furthermore, not all cath labs may possess these technologies. By overdilating the stenosis with a balloon that appeared to be larger than the internal carotid, we were able to deploy the self-expanding stent with excellent clinical outcomes. If dilation with the 7-mm balloon was unsuccessful, we would have likely only performed balloon angioplasty without stenting, which we were unsure would be adequate given the patient’s significant aortic stenosis and upcoming TAVR.
Conclusion
Symptomatic carotid artery stenosis, especially in the setting of preexisting cardiac disease, should be adequately treated with carotid artery stenting as an excellent option. This case report demonstrates that when severely calcified carotid lesions prevent adequate initial predilation and stent passage, subsequent sequential predilation using sequentially larger balloons may allow for sufficient lumen opening, allowing for stent deployment.
Disclosure: The authors have completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors report no conflicts of interest regarding the content herein.
Manuscript accepted August 9, 2022.
Address for correspondence: Richard Heuser, MD, University of Arizona College of Medicine, Phoenix, AZ 85004. Email: heuser58@gmail.com
Related Articles
Transradial Carotid Artery Stenting Complicated With Neck Hematoma, Conservative Is a Valid Option!
Advances in Carotid Artery Imaging: Beyond Luminal Stenosis
An International Trial of Carotid Surgery Compared to Stenting: Interview With Jonathan D. Beard, MD
REFERENCES
1. Inzitari D, Eliasziw M, Gates P, et al. The causes and risk of stroke in patients with asymptomatic internal-carotid-artery stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 2000;342(23):1693-1700. doi:10.1056/nejm200006083422302
2. Brott TG, Hobson 2nd RW, Howard G, et al. Stenting versus
endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010;363(1):11-23. doi:10.1056/NEJMoa0912321
3. Gurm HS, Yadav JS, Fayad P, et al. Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med. 2008;358(15):1572-1579. doi:10.1056/NEJMoa0708028
4. Rosenfield K, Matsumura JS, Chaturvedi S, et al. Randomized trial of stent versus surgery for asymptomatic carotid stenosis. N Engl J Med. 2016;374(11):1011-1020. doi:10.1056/NEJMoa1515706
5. Heuser RR. Can radial access be a practical alternative to treat peripheral vascular disease (PVD)? A different (safer) approach
to treat PVD: experience with a radial sheathless guide. Cath
Lab Digest. May 2019;14-17.
6. Simpfendorfer CC, Dimas AP, Zaidi A, et al. Balloon rupture during coronary angioplasty. Angiology. 1986;37(11):828-831. doi:10.1177/000331978603701106
7. Rao AS, Makaroun MS, Marone LK, Cho JS, Rhee R, Chaer RA. Long-term outcomes of internal carotid artery dissection. J Vasc Surg. 2011;54(2):370-374; discussion 375. doi:10.1016/j.jvs.2011.02.059











