ADVERTISEMENT
Orthoses For Plantar Fasciitis: What The Evidence Reveals
 Do orthoses have an impact for plantar fasciitis? With this question and others in mind, this author offers a primer on the pathomechanics of heel pain, pertinent insights on the biomechanical effects of orthoses and candid assessments on custom versus prefabricated orthoses based on the literature.
Do orthoses have an impact for plantar fasciitis? With this question and others in mind, this author offers a primer on the pathomechanics of heel pain, pertinent insights on the biomechanical effects of orthoses and candid assessments on custom versus prefabricated orthoses based on the literature.
Plantar heel pain represents the most common musculoskeletal condition we treat in podiatric practice.1 Podiatric physicians are not the only caregivers for this problem as over 1 million people with plantar heel pain visit primary care providers and orthopedic surgeons each year.2 The direct cost of treating this disorder ranges from an estimated $192 million to $376 million annually.3 More importantly, researchers have documented the effects of plantar heel pain on quality of life and productivity, which justifies the need for prompt and effective treatment.4,5
The American College of Foot and Ankle Surgeons (ACFAS) has developed and published clinical practice guidelines for treating plantar heel pain.6 Initial treatments include mechanical interventions such as plantar arch strapping, over-the-counter arch supports and heel cups. Only when treatment has failed over the first six weeks do the guidelines recommend custom functional foot orthoses.
The treatments recommended by the ACFAS guidelines for plantar heel pain are based upon the strength of scientific evidence published in the medical literature and the evaluation of outcomes from randomized controlled clinical trials. While many podiatric physicians might be surprised to see such low priority for using custom foot orthoses in treating plantar heel pain from a panel of experts in our own profession, the truth of the matter is that there is very weak, if not conflicting, evidence about the benefit of using any type of orthotic device in the treatment of this common disorder.
Accordingly, let us take a closer look at the published evidence for treating plantar heel pain with foot orthoses and answer the following questions.
 1. Is there evidence that any type of shoe insert (i.e. an orthosis) can be of benefit in treating plantar heel pain?
1. Is there evidence that any type of shoe insert (i.e. an orthosis) can be of benefit in treating plantar heel pain?
2. Is there any evidence showing the superiority of custom versus prefabricated orthotic devices in treating plantar heel pain?
3. Regardless of custom or prefabricated, what are the design characteristics for an orthosis that seem to favor a better outcome when treating plantar heel pain?
How Do The Pathomechanics Of Plantar Heel Pain Relate To Foot Orthotic Therapy?
Researchers have attributed plantar heel pain to a number of clinical conditions including plantar fasciitis, subcalcaneal bursitis, neuritis, medial arch pain, subcalcaneal pain, stone bruise, calcaneal periostitis, subcalcaneal spur and calcaneodynia.6,7 However, it is well accepted that the majority of patients exhibiting plantar heel pain have pathology related to injury of the plantar fascia. Accordingly, clinicians commonly interchange the term plantar fasciitis with plantar heel pain.8,9
There are many proposed risk factors for plantar heel pain, including increased body mass index (BMI), limited ankle joint dorsiflexion, calcaneal spur, leg length discrepancy, diminished heel pad thickness, pes planus, pes cavus, excess pronation and limited range of motion of the first metatarsophalangeal joint (MPJ).6-10 However, a systematic review of the literature found that increased BMI in the non-athletic population and the presence of a calcaneal spur were the only risk factors that had strong evidence for association with plantar heel pain.11 More importantly, the evidence for abnormal foot posture and abnormal foot motion being causative factors for plantar heel pain was inconclusive.
Wearing and colleagues underscored this lack of correlation with foot type and the development of plantar heel pain, finding no correlation between dynamic arch mechanics in runners with and without plantar fasciitis.12 Taunton found that only 30 of 159 runners with plantar fasciitis had an abnormal arch structure, either high or low.13 Simply looking at arch height will not predict a risk of or the presence of plantar heel pain.
Notwithstanding, researchers had attributed mechanical overload as being the primary etiology of plantar fasciitis.14,15 Looking at the histopathlogy of the damaged plantar fascia in patients with plantar heel pain, Lemont and colleagues demonstrated evidence of tissue changes consistent with chronic degeneration: myxoid degeneration and fibroblast necrosis, chondroid metaplasia, angiofibroblastic proliferation, collagen degeneration, an altered ratio of Type III to Type I collagen, and an increased number of abnormal fibroblasts with mitochondrial defects.16
With the recognition that inflammation does not appear to be a dominant feature of plantar fasciitis, newer terminologies (such as “plantar fasciosis” or “plantar fasciopathy”) have emerged and are now in common use when referring to this condition.16,17 The absence of inflammation and the presence of degenerative changes have also been present with chronic tendon disorders.18 Authors have often attributed tendinopathy to tensile overload.19 Accordingly, podiatric physicians often attribute plantar “fasciopathy” to simple overload as well. This has led to a well-recognized mechanism in which failure of the medial arch of the foot or overload of the Achilles tendon will lead to increased tensile load on the plantar fascia.20
In an important paper, Wearing and coworkers present numerous challenges to the assumption that the histopathologic changes in plantar fasciopathy are the result of altered loading or increased tensile strain on the plantar aponeurosis due to abnormal arch mechanics.21 The authors show evidence that heel spurs may be the result of bending rather than traction loading of the insertion of the plantar aponeurosis on the calcaneus. These authors also note that with tendinosis, traction is not always a primary contributor as researchers have shown that other factors such as local ischemic changes as well as the formation of free radicals may cause degenerative changes. Wearing and colleagues demonstrate that gait studies of the kinetics and kinematics of patients with plantar fasciitis reveal conflicting and inconsistent results. Attributing plantar fasciopathy to a failure of arch mechanics leading to excessive traction may be overlooking other etiologic factors. They point out that one must also consider bending, compression and shear forces. This may be one explanation for the conflicting results of foot orthotic therapy in treating patients with plantar heel pain.
 More recent studies have shed further light onto the pathomechanics of plantar fasciitis and possible orthotic strategies to treat the condition. Sullivan and colleagues showed that patients with plantar fasciitis adopt a walking strategy to offload the heel and medial forefoot, presumably as a compensation to decrease pain.22 They speculate that in previous reports of successful treatment of heel pain with foot orthoses, authors may have achieved benefit by augmenting the protective mechanisms of the foot to prevent pain during walking.23-24
More recent studies have shed further light onto the pathomechanics of plantar fasciitis and possible orthotic strategies to treat the condition. Sullivan and colleagues showed that patients with plantar fasciitis adopt a walking strategy to offload the heel and medial forefoot, presumably as a compensation to decrease pain.22 They speculate that in previous reports of successful treatment of heel pain with foot orthoses, authors may have achieved benefit by augmenting the protective mechanisms of the foot to prevent pain during walking.23-24
Chang and coworkers recognized that previous gait studies of patients with plantar fasciitis did not validate the identification of abnormal rearfoot motion and abnormal arch mechanics as causative factors.25 However, they point out the shortcomings of using two-dimensional measurement and modeling the foot as a single rigid segment. Using a 3D multi-segment foot model, Chang and coworkers showed that patients with plantar heel pain had greater amounts of rearfoot pronation during gait than healthy individuals. They also measured greater peak first MPJ dorsiflexion motion during gait in patients with plantar heel pain. Based on this finding, the authors speculated that the first MPJ can place an excessive load on the medial band of the central plantar aponeurosis, which could explain why the medial calcaneal tubercle is the most frequent site of plantar heel pain. This is the first paper to verify previous hypotheses that excessive first MPJ dorsiflexion could actually be a contributing factor for plantar heel pain through excessive loading of the windlass mechanism.26 It would be interesting to see if future orthotic strategies might address this factor when treating plantar heel pain.
What Are The Potential Biomechanical Effects Of Foot Orthotics On The Plantar Fascia?
Although many studies have measured the effects of foot orthoses on rearfoot motion, none focused on arch mechanics and load on the plantar fascia.27-30 Williams and colleagues were among the first to suggest that important changes in midfoot and arch mechanics could occur with custom foot orthotics.31
Early investigators speculated that the plantar fascia, also known as the plantar aponeurosis, carries the bulk of load during standing and walking, maintaining the structural integrity of the arch of the foot.32-34 From an engineering standpoint, authors have compared foot morphology to both a structured beam as well as a truss, stabilized by a “tie,” which is the plantar aponeurosis.35 Under weightbearing, the plantar aponeurosis prevents the ends of the arch from elongating. This mechanism has been the mainstay of the long held tradition of using “arch supporting orthotics” to treat plantar fasciitis.
Between 1996 and 2001, Kogler and coworkers published three important papers that provide interesting insight into the role that foot orthoses play in decreasing strain in the plantar aponeurosis.36-38 These were cadaveric studies of a static model with the foot flat and application of load equivalent to body weight. The experimental model in all three studies simulates quiet stance and the authors agree that the findings may not predict outcomes in live patients during dynamic gait.
The first Kogler study focused on certain foot orthotic designs to potentially offload the central band of the plantar aponeurosis.36 Custom orthoses significantly reduced strain in the plantar fascia as the researchers applied load on the experimental foot model. However, only those orthoses that had significant contour under the “apical” portion of the arch (i.e. talonavicular joint) provided benefit. The traditional “Root style” custom foot orthosis did not reduce strain in the plantar fascia, presumably because the medial trim line fell lateral to the apex of the medial longitudinal arch.
The second Kogler study evaluated the placement of wedges under the cadaveric foot model, measuring their effects on plantar fascia strain.37 Out of eight different combinations, only a lateral forefoot wedge significantly decreased strain on the plantar aponeurosis. The authors speculated that this lateral forefoot wedge may have augmented “locking” of the calcaneocuboid joint, increasing load on the lateral ligamentous structures of the foot and decreasing load on the medial-central band of the plantar fascia. This study also showed that the forefoot medial wedge increased strain in the plantar fascia, which validates the truss mechanism theory. The distal strut of the truss (the first ray) will have an increased dorsiflexion moment when one places a medial wedge under the forefoot. This will cause increased strain on the medial-central band of the plantar aponeurosis.35
 Finally, Kogler and colleagues studied the effects of heel elevation wedges placed under the cadaveric foot model.38 Surprisingly, heel wedges did not significantly offload tension in the plantar fascia. Only when researchers used a wedge with a contoured “shank profile,” simulating a higher heel shoe, did tension reduce in the plantar fascia. The findings may have been different if the cadaveric model in this study incorporated physiologic tension in the Achilles tendon. Authors have shown that the Achilles provides a twofold greater load on the plantar fascia than body weight alone.39
Finally, Kogler and colleagues studied the effects of heel elevation wedges placed under the cadaveric foot model.38 Surprisingly, heel wedges did not significantly offload tension in the plantar fascia. Only when researchers used a wedge with a contoured “shank profile,” simulating a higher heel shoe, did tension reduce in the plantar fascia. The findings may have been different if the cadaveric model in this study incorporated physiologic tension in the Achilles tendon. Authors have shown that the Achilles provides a twofold greater load on the plantar fascia than body weight alone.39
Ferber and Benson studied prefabricated foot orthoses worn by 20 people and measured kinematic changes in the foot and ankle.40 These devices reduced plantar fascia strain by over 30 percent. Interestingly, the effects were not improved if clinicians heat molded the same devices to the foot of the individual.
In another investigation conducted by Ferber and Benson, they studied three popular over-the-counter prefabricated foot orthotic devices (Powerstep®, Superfeet® and Sole®) to determine their effects on multi-segment foot biomechanics and plantar fascia strain.41 All three devices reduced plantar fascia strain by over 30 percent.
A Closer Look At Patient Outcome Studies On Orthoses For Plantar Fasciitis
There are many published reports of outcomes using different types of foot orthotic devices to treat plantar heel pain. Before evaluating these studies, one has to recognize that foot orthoses can embody many different materials and designs. The definition of an orthosis is “an apparatus used to support, align, prevent, or correct deformities or to improve the function of movable parts of the body.”42 Accordingly, an orthosis to treat plantar heel pain could include arch supports, heel pads or even metatarsal pads. The definition of a custom functional foot orthosis, a mainstay of podiatric biomechanical treatments, is: “An orthotic device that is designed to control abnormal motion or abnormal position of the foot and to control the abnormal motion or abnormal position of the lower extremity that is affected by the position and/or motion of the foot.”43
Recognizing the broad definitions of orthoses, one can understand the difficulty of interpreting the results of studies of these devices treating plantar heel pain. Not only are there differences between custom and prefabricated foot orthoses, there are many differences in materials and design of these devices within each of the two classifications. For the clinician seeking guidance in implementing foot orthotic therapy for treating plantar heel pain, the challenge becomes daunting when evaluating the quality of the published research as well as the unique features of the devices that presumably led to the reported outcomes.
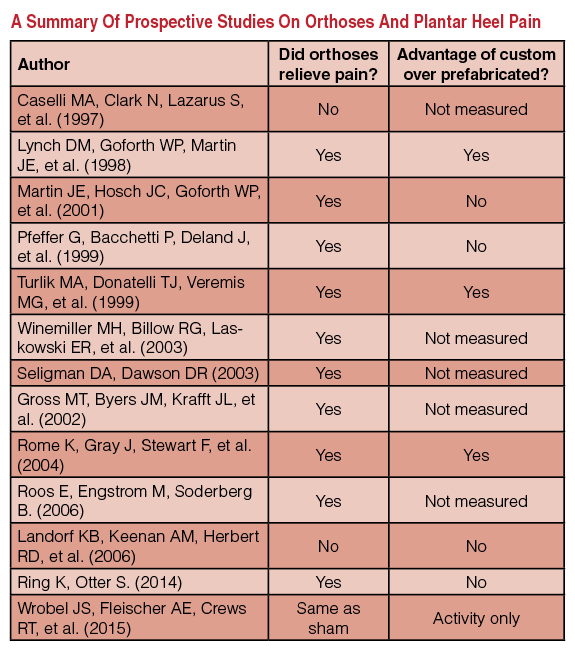
Most studies of foot orthotic treatment of plantar heel pain published before the year 2000 were retrospective case studies that did not follow the current standards of evidence-based research using randomized controlled trials (RCTs). In 2004, Landorf and Keenan examined all of the published studies of foot orthotic therapy and found only six published RCTs studying foot orthoses in the treatment of plantar fasciitis.44 According to the authors, all six studies had methodological flaws including allocation concealment, high dropout rates, a lack of blinding and lack of comparison to control groups.
Notwithsta nding the valid criticism of methodologies, there were six papers that Landorf and Keenan selected as best in demonstrating the current knowledge in 2004.45-50 Two of these studies involved flat, cushioned insoles with and without magnets.45,50 Both of these studies showed no improvement with magnets. Interestingly, one study showed significant improvement in plantar heel pain with the cushioned insoles, regardless of whether magnets were included.50
nding the valid criticism of methodologies, there were six papers that Landorf and Keenan selected as best in demonstrating the current knowledge in 2004.45-50 Two of these studies involved flat, cushioned insoles with and without magnets.45,50 Both of these studies showed no improvement with magnets. Interestingly, one study showed significant improvement in plantar heel pain with the cushioned insoles, regardless of whether magnets were included.50
The remaining four papers reviewed by Landorf and colleagues compared custom versus prefabricated orthoses for the treatment of plantar fasciitis.46-49 Two studies showed the superiority of custom orthoses in comparison to prefabricated orthoses.46,49 One study showed better results with a simple heel pad in comparison to custom functional foot orthoses.48 Another study showed that both prefabricated and custom foot orthoses provided significant relief of plantar heel pain, but found no difference between the two types of devices.47
Recognizing the need for a more robust study comparing custom versus prefabricated orthoses in treating plantar heel pain, Landorf and Keenan conducted a randomized clinical trial that was blinded and included a control group.51 After three months of treatment, patients wearing both the prefabricated and custom foot orthoses showed improvements in pain and function in comparison to a sham orthosis. These improvements were minimal and there was no superiority or difference in improvement when comparing custom versus prefab devices. Furthermore, after 12 months, there was no measurable benefit in outcome with either the custom or prefab orthosis in comparison to the sham device.
In 2009, Lee and colleagues published a meta-analysis of six published studies to determine the short, intermediate and long-term effects of foot orthoses to treat pain and function in patients with plantar fasciits.52 They selected only studies that were either RCTs or prospective cohort studies. The previously cited papers from Landorf and Winemiller were included as well as four other studies.50-56 This review showed that all types of foot orthoses (custom, non-custom, functional and accommodative) will decrease pain and improve foot function in patients with plantar fasciitis. Authors measured the results both immediately, during the intermediate six- to 12-week period and long term after 12 weeks. It is important to note that the Winemiller study of magnetic and non-magnetic padded insoles strongly influenced the positive results of this meta-analysis, showing an overall benefit of foot “orthoses.”50
In 2008, a Cochrane Review of 11 RCTs and controlled clinical trials focused on custom orthotics in the treatment of any type of foot pain.57 In this review, authors evaluated five papers relevant to treating plantar fasciitis. These include four previously cited trials as well as a trial published by Dimou and colleagues.47,48,51,55,58 In comparison to other standard treatments for plantar fasciitis, custom foot orthoses showed no superiority. Custom foot orthoses were not superior to prefabricated foot orthoses as both provided improvement in pain and function in treating patients with plantar fasciitis. After this Cochrane Review, a prospective clinical trial published by Ring and Otter compared a custom to a prefabricated foot orthotic and mirrored the same findings, showing that prefab devices provided the same pain relief as custom orthoses.59
 To address previous controversy and shortcomings of research on custom versus prefabricated foot orthotics treating plantar heel pain, the American Podiatric Medical Association (APMA) funded an independent study conducted at the Center for Lower Extremity Research at the Dr. William M. Scholl College of Podiatric Medicine at the Rosalind Franklin University of Medicine and Science in Chicago.60 This was a randomized, prospective, double-blind clinical trial testing the effectiveness of custom functional foot orthoses, prefabricated off-the-shelf orthoses and sham orthoses in the treatment of 77 patients with plantar fasciitis.
To address previous controversy and shortcomings of research on custom versus prefabricated foot orthotics treating plantar heel pain, the American Podiatric Medical Association (APMA) funded an independent study conducted at the Center for Lower Extremity Research at the Dr. William M. Scholl College of Podiatric Medicine at the Rosalind Franklin University of Medicine and Science in Chicago.60 This was a randomized, prospective, double-blind clinical trial testing the effectiveness of custom functional foot orthoses, prefabricated off-the-shelf orthoses and sham orthoses in the treatment of 77 patients with plantar fasciitis.
The results echoed previous studies.60 There was no significant benefit of any type of orthosis, including sham devices, over traditional stretching and icing in terms of reducing morning pain. The custom and prefabricated orthoses did reduce evening pain in comparison to the sham device, but there was no superiority of custom devices. There was no benefit of custom or prefab foot orthoses in comparison to sham devices in terms of overall foot function. The custom foot orthoses did produce a significant improvement in spontaneous physical activity, duration of standing and duration of walking in comparison to the other devices. The researchers suggested that objective measures of activity and weightbearing function may be more sensitive and specific for measuring clinical outcomes of orthotic treatment than traditional clinical outcome measures such as pain and disease-specific quality of life.
Applying The Research Findings To Your Practice
Foot orthoses in many shapes and forms do relieve heel pain on an immediate, intermediate and long-term basis. Based upon the evidence to date, there is no advantage to using custom over prefabricated foot orthoses when treating patients with plantar heel pain. However, most podiatric physicians continue to prescribe custom foot orthoses and rely on them more than prefab devices to treat most chronic foot conditions.61
Many podiatric physicians reading this article or previously published research on the subject would argue that they get better clinical outcomes in their own practices using custom rather than prefab devices. They would ask how robust, Level 1 studies such as those conducted by Landorf, Wrobel and respective colleagues could show no difference in the efficacy of custom devices in comparison to prefab orthoses.51,60 In fact, both of these studies failed to show any significant advantage to using any type of foot orthotic device to treat plantar heel pain.
 In regard to evidence-based medicine, relying on randomized controlled trials has driven clinical decision making as well as approved coverage by third party insurance carriers for the past 10 years. However, using these studies as gospel or gold standard is not without certain shortcomings. An article published in Podiatry Today previously focused on this issue.62
In regard to evidence-based medicine, relying on randomized controlled trials has driven clinical decision making as well as approved coverage by third party insurance carriers for the past 10 years. However, using these studies as gospel or gold standard is not without certain shortcomings. An article published in Podiatry Today previously focused on this issue.62
When a large group of patients wear custom or prefabricated foot orthotics to relieve plantar heel pain, researchers pool the results and report them for the specific treatment groups. It is rare in published RCTs to see an analysis of the individual patients or study participants to see who responded to treatment and who did not. Certainly, there were people in the Landorf and Wrobel studies who had significant relief of pain using custom foot orthoses, some individuals who had significant relief with prefab devices, and some who had no relief.51,60
In the Ferber study of “semi-custom” foot orthotics, more than half of those studied demonstrated reduced plantar fascia strain when the orthotic device was heat molded to their foot while the remainder of the study participants did not have any improvement.41 The large variability of the entire study group caused the final statistical analysis to show no advantage to custom molding. Other studies probably had similar variability in response to treatment within each group when comparing custom to prefabricated orthotics although only Ferber provided such an analysis.
In Conclusion
Foot orthoses in various forms provide immediate, intermediate and long-term relief of plantar heel pain. There is weak evidence for any superiority of custom foot orthoses versus prefabricated devices to treat this condition. The challenge for future outcomes research relevant to foot orthotic therapy is to determine which individuals respond best to custom devices, those who respond best to prefabricated devices and those who will not benefit at all. We know that the results which are averaged for a large group of patients show no advantage of custom foot orthotics over prefabricated devices but we need to know how individuals responded and what characteristics we can identify to select the proper treatment.
Dr. Richie is an Adjunct Associate Professor within the Department of Applied Biomechanics at the California School of Podiatric Medicine at Samuel Merritt University in Oakland, Calif. He is a Fellow and Past President of the American Academy of Podiatric Sports Medicine. Dr. Richie is a Fellow of the American College of Foot and Ankle Surgeons. He is in private practice in Seal Beach, Calif. Dr. Richie writes a monthly blog for Podiatry Today. One can access his blog at www.podiatrytoday.com/blogs/doug-richie-jr-dpm/feed .
References
- Al Fischer Associates, Inc. 2002 Podiatric practice survey: statistical results. J Am Podiatr Med Assoc. 2003;93(1):67–86.
- Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004; 25(5):303-10.
- Tong KB, Furia J. Economic burden of plantar fasciitis treatment in the United States. Am J Orthop. 2010; 39(5):227-31.
- Irving DB, Cook JL, Young MA, Menz HB. Impact of chronic plantar heel pain on health-related quality of life. J Am Podiatr Med Assoc. 2008; 98(4):283-289.
- Thomas JL, Christensen JC, Kravitz SR, et al. The diagnosis and treatment of heel pain: a clinical practice guideline - revision 2010. J Foot Ankle Surg. 2010; 49(3Suppl):S1-19.
- Rome K. Anthropometric and biomechanical risk factors in the development of plantar heel pain: a review of the literature. Phys Ther Rev. 1997;2(3):123—34.
- Crawford F, Thomson C. Interventions for treating plantar heel pain. Cochrane Database Syst Rev. 2003;3 (CD000416).
- Rome K. Heel pain: diagnosis and management. Podiatry Now. 2005;8(4):S1-8.
- Barrett P, Black M. In response to: anthropometric and biomechanical risk factors in the development of plantar heel pain—–a review of the literature [Rome, Phys Ther Rev. 1997;2:123-34]. Phys Ther Rev. 1998;3(1):55-6.
- Buchbinder R. Plantar fasciitis. N Engl J Med. 2004;350(21):2159-66.
- Irving DB, Cook JL, Menz HB. Factors associated with chronic plantar heel pain: a systematic review. JSAMS. 2006;9(1):11-22.
- Wearing SC, Smeathers JE, Yates B, et al. Sagittal movement of the medial longitudinal arch is unchanged in plantar fasciitis. Med Sci Sports Exerc. 2004; 36(10):1761-7.
- Taunton JE, Ryan MB, Clement DB, et al. A retrospective case- control analysis of 2002 running injuries. Br J Sports Med. 2002; 36(2):95-101.
- Chandler TJ, Kibler WB. A biomechanical approach to the prevention, treatment, and rehabilitation of plantar fasciitis. Sports Med. 1993; 15(5):344-52.
- Cornwall MW, McPoil TG. Plantar fasciitis: etiology and treatment. J Orthop Sports Phys Ther. 1999; 29(12):756-60.
- Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003; 93(3):234-7.
- Rompe JD, Cacchio A, Weil Jr L, et al. Plantar fascia-specific stretching versus radial shock-wave therapy as initial treatment of plantar fasciopathy. J Bone Joint Surg Am. 2010; 92(15):2514-2.
- Astrom M, Rausing A. Chronic Achilles tendinopathy: a survey of surgical and histopathologic findings. Clin Orthop. 1995; 316:151-64.
- Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon: a controlled study of 891 patients. J Bone Joint Surg Am. 1991; 73(10):1507-25.
- Kogler GF, Solomonidis SE, Paul JF. In vitro method for quantifying the effectiveness of the longitudinal arch support mechanism of a foot orthosis. Clin Biomech. 1995; 10(5):245-52.
- Wearing SC, Smeathers JE, Urry SR, et al. The pathomechanics of plantar fasciitis. Sports Med. 2006; 36(7):585-611.
- Sullivan J, Burns J, Adams R. Plantar heel pain and foot loading during normal walking. Gait Posture. 2015; 41(2):688–693.
- Bonanno DR, Landorf KB, Menz HB. Pressure-relieving properties of various shoe inserts in older people with plantar heel pain. Gait Posture. 2011;33(3):385–9.
- Chia KK, Suresh S, Kuah A, et al. Comparative trial of the foot pressure patterns between corrective orthotics, formthotics, bone spur pads and flat insoles in patients with chronic plantar fasciitis. Ann Acad Med Singapore. 2009;38(10):869–75.
- Chang R, Rodrigues PA, Van Emmerik REA, Hamill J. Multi-segment foot kinematics and ground reaction forces during gait of individuals with plantar fasciitis. J Biomech. 2014; 47(11):2571–2577.
- Cheng HY, Lin CL, Wang HW, Chou SW. Finite element analysis of plantar fascia under stretch-the relative contribution of windlass mechanism and Achilles tendon force. J Biomech. 2008; 41(9):1937–1944.
- Brown GP, Donatelli R, Catlin PA, et al. The effect of two types of foot orthoses on rearfoot mechanics. J Orthop Sports Phys Ther. 1995; 21(5):258-267.
- Rodgers MM, Leveau BF. Effectiveness of foot orthotic devices used to modify pronation in runners. J Orthop Sports Phys Ther. 1982; 4(2):86-90.
- Stacoff A, Reinschmidt C, Nigg BM, et al. Effect of foot orthoses on skeletal motion during running. Clin Biomech. 2000; 15(1):54-64.
- Nester CJ, van der Linden ML, Bowker P. Effect of foot orthoses on the kinematics and kinetics of normal walking gait. Gait Posture. 2003; 17(2):180-187.
- Williams DS, McClay IS. Measurements used to characterize the foot and the medial longitudinal arch: reliability and validity. Phys Ther. 2000; 80(9):864-871.
- Hicks JH. The foot as a support. Acta Anat. 1955; 25(1):34-45.
- Hicks JH. The three weight bearing mechanisms of the foot. In: Evans FG, ed. Biomechanical Studies of the Musculoskeletal System. Charles C. Thomas, Springfield, IL, 1961, pp. 161-91.
- Wright DG, Rennels BS. A study of the elastic properties of plantar fascia. J Bone Joint Surg. 1964; 46:482-92.
- Sarrafian SK. Functional characteristics of the foot and plantar aponeurosis under tibiotalar loading. Foot Ankle. 1987;8(1):4-18.
- Kogler GF, Solomonidis SE, Paul JP. Biomechanics of longitudinal arch support mechanisms in foot orthoses and their effect on plantar aponeurosis strain. Clin Biomech. 1996; 11(5):243-252.
- Kogler GF, Veer EB, Solomonidis SE, Paul JP. The influence of medial and lateral placement of orthotic wedges on loading of the plantar aponeurosis. In vitro study. J Bone Joint Surg. 1999; 81(10):1403-1413.
- Kogler GF, Veer FB, Verhulst SJ, et al. The effect of heel elevation on strain within the plantar aponeurosis: in vitro study. Foot Ankle Int. 2001; 22(5):433-439.
- Cheung JT, Zhang M, An K. Effect of Achilles tendon loading on plantar fascia tension in the standing foot. Clin Biomech. 2006; 21(2):194–203.
- Ferber R, Benson B. Changes in multi-segment foot biomechanics with a heat-moldable semi-custom foot orthotic device. J Foot Ankle Res. 2011; 4(1):18.
- Ferber R, Hettinga BA. A comparison of different over-the-counter foot orthotic devices on multi-segment foot biomechanics. Prosth Orth Int. 2015; epub May 26.
- Available at https://encyclopedia.thefreedictionary.com/orthosis .
- PFOLA technical standards document. Available at www.pfola.org .
- Landorf KB, Keenan AM, Herbert RD. Effectiveness of different types of foot orthoses for the treatment of plantar fasciitis. J Am Podiatr Med Assoc. 2004; 94(6):542–549.
- Caselli MA, Clark N, Lazarus S, et al. Evaluation of magnetic foil and PPT insoles in the treatment of heel pain. J Am Podiatr Med Assoc. 1997; 87(1):11.
- Lynch DM, Goforth WP, Martin JE, et al. Conservative treatment of plantar fasciitis: a prospective study. J Am Podiatr Med Assoc. 1998; 88(8):375-80.
- Martin JE, Hosch JC, Goforth WP, et al. Mechanical treatment of plantar fasciitis: a prospective study. J Am Podiatr Med Assoc. 2001; 91(2):55-62.
- Pfeffer G, Bacchetti P, Deland J, et al. Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot Ankle Int. 1999; 20(4):214-21.
- Turlik MA, Donatelli TJ, Veremis MG. A comparison of shoe inserts in relieving mechanical heel pain. The Foot. 1999; 9(1):84.
- Winemiller MH, Billow RG, Laskowski ER, et al. Effect of magnetic vs sham-magnetic insoles on plantar heel pain: a randomized controlled trial. J Am Med Assoc. 2003; 290(11):1474-8.
- Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med. 2006; 166(12):1305–1310.
- Lee SY, Mckeon P, Hertel J. Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis. Phys Ther Sport. 2009; 10(1):12-18.
- Seligman DA, Dawson DR. Customized heel pads and soft orthotics to treat heel pain and plantar fasciitis. Arch Phys Med Rehabil. 2003; 84(10):1564–1567.
- Rome K, Gray J, Stewart F, et al. Evaluating the clinical effectiveness and cost-effectiveness of foot orthoses in the treatment of plantar heel pain: a feasibility study. J Am Podiatr Med Assoc. 2004; 94(3):229–238.
- Roos E, Engstrom M, Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int. 2006; 27(8):606–611.
- Gross MT, Byers JM, Krafft JL, et al. The impact of custom semirigid foot orthotics on pain and disability for individuals with plantar fasciitis. J Orthoped Sports Phys Ther. 2002; 32(4):149–157.
- Hawke F, Burns J, Radford JA, et al. Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst Rev. 2008; 3: CD006801.
- Dimou ES, Brantingham, JW, Wood T. A randomised, controlled trial (with blinded observer) of chiropractic manipulation and achilles stretching vs. orthotics for the treatment of plantar fasciitis. J Am Chiropract Assoc. 2004;41(9):32–42.
- Ring K, Otter S. Clinical efficacy and cost-effectiveness of bespoke and prefabricated foot orthoses for plantar heel pain: a prospective cohort study. Musculoskelet Care. 2014; 12(1):1–10.
- Wrobel JS, Fleischer AE, Crews RT, Jarrett B, Najafi B. A randomized controlled trial of custom foot orthoses for the treatment of plantar heel pain. J Am Podiatr Med Assoc. 2015; 105(4):281-94.
- Donoghue SK. Banding together for practice success. 32nd Annual Practice Management Survey. Podiatry Management, March 2015.
- Smith RJ. Can evidence-based medicine be a reality in practice? Podiatry Today. 2008; 21(5):38-44.











