Alternative Payment Models: Where Are We Now?
Health Care Payment Learning and Action Network (HCP LAN) is dedicated to moving the health care system from volume-based, fee-for-service reimbursement, to alternative payment models (APM). While there are a large number of different types of APMs, broadly, all of them shift more financial risk to providers while also linking reimbursement to quality of care. In fact, HCP LAN has the goal of having 100% of reimbursements for traditional Medicare and Medicare Advantage fall under two-sided risk APMs and 50% of commercial and Medicaid reimbursements fall-under two-sided risk APMs by 2025.
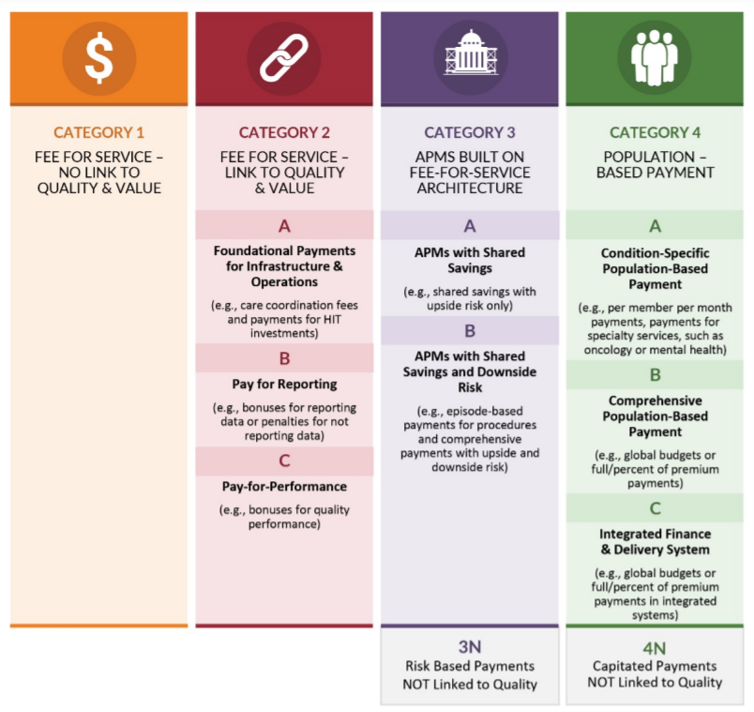
HCP LAN defines APMs as falling under one of four types:
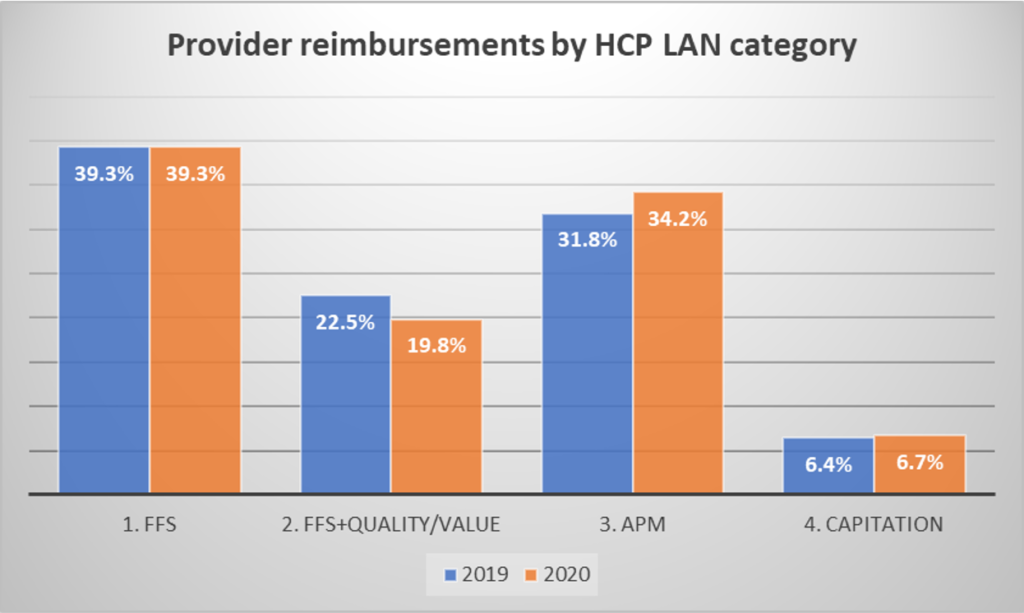
In their 2020-2021 report titled APM Measurement: Progress of Alternative Payment Models, HCP LAN uses data from 2019 and 2020 to examine whether APM are gaining market share. From 2019 to 2020, we do see some shift towards more APM and capitation payment, but FFS payments held steady at 39.3% of reimbursements. It should not be surprising that reimbursement structures did not change much since 2020 was the height of the COVID-19 pandemic.
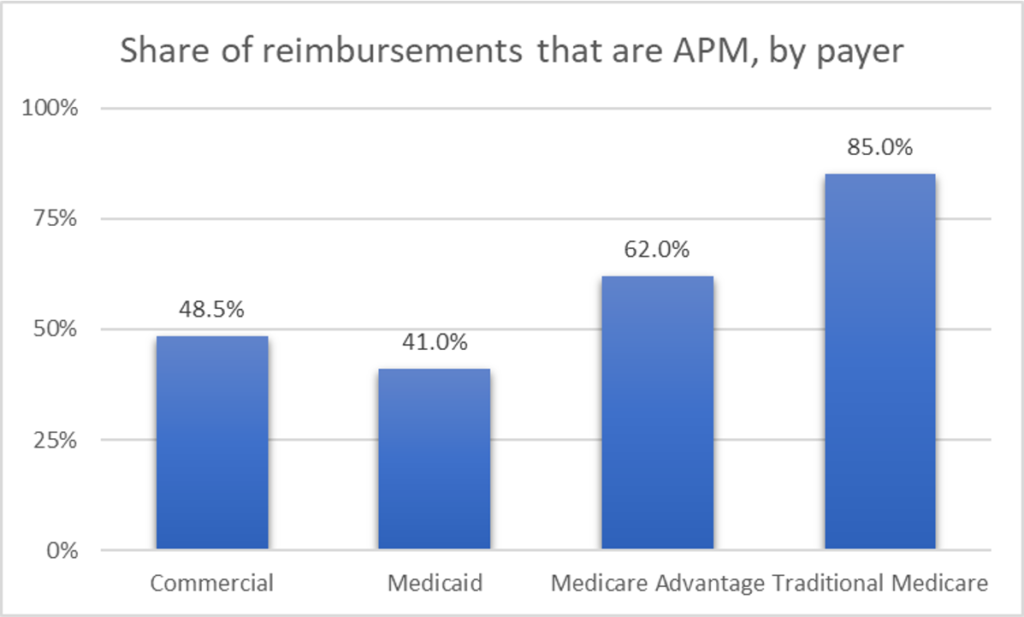
Rates of use of APM also varied across payer types. Traditional Medicare had the highest use of APMs (i.e., reimbursements in the HCP LAN categories 2, 3 or 4), and commercial insurance had the lowest (see figure below). Note that global capitation was fairly uncommon across most payers (3%-6%) with the exception of Medicare Advantage where 21.8% of payments were made via global capitation.
HCP LAN also surveyed payers and found that 87% believed that APM activity will increase in the future. The most interest was in bundled payment (47%) and shared savings (21%) APM types. Of note, about half (44%) of respondents believed that APMs would result in increased provider consolidation.
While payers are excited about increased financial certainty APMs would bring, providers have concerns. The top 3 challenges for implementing APMs were:
- Provider willingness to take on financial risk
- Provider ability to operationalize APM
- Provider interest/readiness
APM have a number of obvious attractive features, but also challenges as well. Clearly, linking reimbursement to quality of care and value is a laudable goal. However, estimating value is easiest in a static setting where expected outcomes and costs are known with reasonable certainty. Due to COVID-19, there was significant uncertainty over costs both due to the cost of COVID-19 directly and its impact on treating other diseases. It goes without saying that global pandemics make implementing APMs challenging. Similarly, as new therapeutic innovations enter the market, quality may improve but so may cost; as treatment paradigms shift notions of value–and corresponding APM structures–may need to evolve over time.
Commentary posted with permission from Dr Shafrin.



















