Abstract: Melanoma treatment costs continue to rise. Sunscreen is a photoprotective tool that may reduce the incidence of melanoma but can be cost prohibitive for lower socioeconomic populations. New York State (NYS) Medicaid, the primary insurer for the underserved in NYS, does not provide coverage of sunscreen. We developed a model testing the hypothesis that NYS Medicaid coverage of sunscreen for pediatric beneficiaries is a cost-effective strategy for decreasing the burden of melanoma. Study Design and Methods: A cost-effectiveness analysis was performed using a health state transition Markov model based on data from the published literature. Outcomes measured included health costs, quality-adjusted life-years (QALYs), and incremental cost-effectiveness ratio (ICER). Results: Using a health care willingness-to-pay threshold of $150,000/QALY, frequent sunscreen use is a cost-effective intervention (ICER<$8225/QALY) and preferable to some or no sunscreen use. Conclusion: Sunscreen coverage in the pediatric NYS Medicaid population can be a cost-effective intervention. Sunscreen price is a significant barrier to use but may be overcome by a state and national recommendation for insurers to cover sunscreen for the underserved.
Key Words: skin cancer, melanoma, pediatrics, health economics, primary prevention, sunscreen
Melanoma is a potentially fatal but preventable disease that has seen a dramatic rise in incidence in the last two decades. Today, melanoma is the fifth most common cancer among men and women,1 and recently there has been a substantial increase in the incidence of melanoma affecting individuals aged 15 to 39 years.2 In 2011, the annual cost of treating melanoma in the United States was estimated at $3.3 billion.3 These costs rose significantly in the last 5 years due to new targeted and immunological therapies. In contrast, the cost of photoprotective strategies like sunscreen or protective clothing is far less than the costs of skin cancer treatment.
Recent studies provide evidence of the positive association between sunscreen use in childhood and a reduction in melanoma incidence. In 2011, a randomized clinical trial in Australia found that regular sunscreen use was associated with a lower risk of invasive melanoma.4 Similarly, a study of Australian adults aged younger than 45 years found that both self-reported childhood and lifetime sunscreen use were associated with a lower risk of melanoma.5 Those applying sunscreen most frequently had a reduction in melanoma risk of up to 40%.
However, for many families, including those covered by Medicaid, sunscreen products are cost prohibitive. Sunscreens can amount to as much as 1.1% to 2.3% of the total income of a Medicaid beneficiary.6a The cost of sunscreen should be evaluated in the context of the rising costs of melanoma treatment. Here, we present a model to determine if providing sunscreen for the pediatric population can be a cost-effective primary prevention strategy for New York State (NYS) Medicaid and would reduce the morbidity of melanoma and costs associated with treatment.
Materials & Methods
A cost-effectiveness analysis was performed using data estimates from the published literature to evaluate the impact of sunscreen use in children on reducing lifetime melanoma morbidity. The intervention was proposed for White and non-White children (aged 3-18 years) in the Medicaid population in NYS. Age 3 years was chosen as the starting age due to availability of data on sunscreen usage (Supplemental Text).5 The intervention tested three levels of sunscreen application during childhood: frequent use (almost daily use, ideally re-applying every 2 hours, thickness ~2 mg/cm2, SPF >30), some use (50% frequent use: no re-applications, thickness ~1mg/cm2, and/or SPF<30), and no use. Of note, “some” sunscreen use denotes a lower-than-recommended level of sunscreen protection over the course of the day but assumes that sunscreen would still be applied almost daily as with frequent use. Some sunscreen use would therefore not expose the individual to periodic, brief episodes of high-intensity exposure, which in some studies has been found to increase melanoma risk.7 A lifetime Markov model was constructed to simulate the occurrence of melanoma over a lifetime horizon. The primary outcome was the cost per quality-adjusted life-year (QALY).
Markov Model
A health state transition Markov model was constructed in TreeAge Pro 2018 (TreeAge Software, Inc, Williamstown, MA) (Supplemental Image 1). The cohort model consisted of mutually exclusive health states so that individuals occupy only one health state at a time. The health states included (1) no disease/well; (2) local melanoma; (3) regional melanoma; (4) metastatic melanoma; and (5) dead. The model assumed NYS Medicaid children would receive the intervention starting at age 3 years and continue for 15 years (to age 18 years) based on available literature.5 A yearly cycle length was used to model the costs and effects over the remaining lifetime, up to a maximum age of 79 years (the average life expectancy in the United States). The distribution of NYS Medicaid children population by gender (male, female) and race (White, non-White) was taken into account.8 Background mortality rates were age-dependent in the model, based on NYS population data in 2016.9 The model estimated all health and cost outcomes for children who received the intervention at three different levels: frequent sunscreen use, some use, and no use. Key outcomes of the model include health care costs, QALYs, and the incremental cost-effectiveness ratio (ICER). Recent guidelines for best-practice health economic modeling were adhered to during the study.
Model Inputs and Sources
Table 1 provides detailed information on the data and calculations used in the model. Information on transition probabilities, mortality rates, and health utilities is available in the Supplementary Materials.
Resource use and costs. The study included resources attributed to the health system if the cost of sunscreen was a covered benefit. Cost of sunscreen was based on the study by Johal et al,6 which estimates that an adult applying sunscreen moderately under “actual” use conditions spends $98.18 (generic) to $201.30 (name-brand) per year. We estimated that children on average use half of the adult amount ($49.09-$100.65/year), so our model was based on a range of $48 to $72 with an estimated mean cost of sunscreen of $60/year. We assumed frequent sunscreen use to cost $60/year, some sunscreen use to cost $30/year, and no sunscreen to cost $0/year.
The costs to the health care system included resources consumed in the routine diagnosis, treatment, and follow-up of melanoma. Health care costs included visits for a whole-body clinical skin exam, pathology and excision costs for melanoma, and various treatments (eg, cryotherapy, excision, chemotherapy, immunotherapies). Health care cost for diagnosis and treatment of localized melanoma was based on Guy et al,10 whereas the estimated cost of treating advanced melanoma incorporating new therapies (eg, nivolumab and ipilimumab) provided to eligible patients was based on current National Comprehensive Cancer Network treatment guidelines11 and recent cost estimates of advanced melanoma.12 Resources were valued using those reported in the literature and inflated to 2019 US dollars.
Analyses. The model calculated expected values (mean per person), including costs and QALYs (effectiveness) for the three arms. Future costs and benefits were discounted at 3% per year to adjust to present values. A 3% discount rate was chosen in concordance with the current Federal Reserve discount rate in 2019.13 The ICER was calculated as the difference in costs between the frequent or some sunscreen use arms and the no use arm divided by the differences in QALYs. A threshold of $150,000/QALY may be used as the upper-limit benchmark according to the Institute for Clinical and Economic Review of whether a new service is cost-effective and is in line with government reimbursement decisions made in United States.14
Sensitivity. To determine the extent of uncertainty in the modeled estimates, we undertook one-way sensitivity analyses in which each model input was varied through a range of plausible values (Table 1) and changes to the base results were observed. Model parameters were tested between high and low values using the 95% CIs when available. In the absence of CIs, other values reported in the literature or ±30% of the base value were applied (Table 1). We also performed a probabilistic sensitivity analysis by resampling 1000 times at random from assigned probability distributions for each parameter. This approach addresses the uncertainty of data estimates simultaneously using a Monte-Carlo simulation. Gamma distributions were assigned for cost inputs and beta distributions to probabilities and utilities.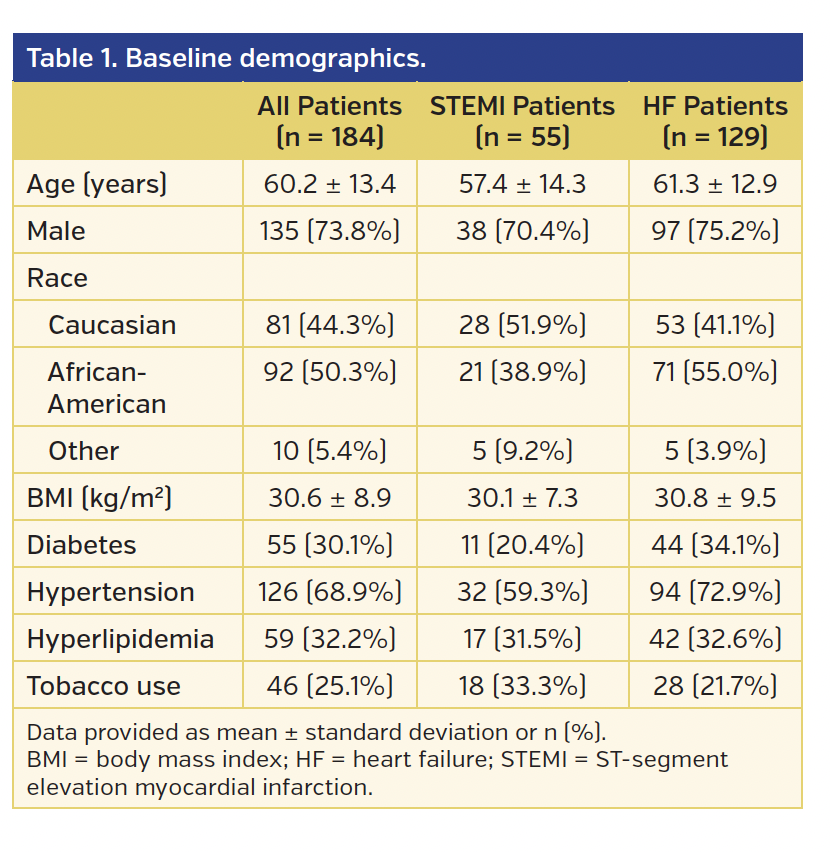
Of note, to take into account the ethnic differences between the Watts and the NYS Medicaid population, NYS Medicaid data on White vs non-White race was used to calculate specific melanoma risks in each subgroup. Likewise, the effect of gender and tanning bed use on melanoma risk were also calculated independently (Supplemental Table 1).
Results
Table 2 provides the primary outputs of the model for the three levels of intervention (ie, frequent, some, no sunscreen use). The net present value cost for frequent, some, and no sunscreen was $1302, $1248, and $973, respectively. In other words, compared with no sunscreen use, the additional cost to Medicaid for frequent sunscreen coverage is $329 per enrollee, for a gain of 0.04 QALYs, at an ICER of $8225/QALY. For some sunscreen coverage, the additional cost is $275 per enrollee, for a gain of 0.02 QALYs, at an ICER of $13,750/QALY. Cost-effectiveness acceptability curves demonstrate that only when the willingness-to-pay is less than $8225/QALY is no sunscreen coverage the preferred option. In all other cases, frequent sunscreen is the most cost-effective and preferred intervention option (Figure 1).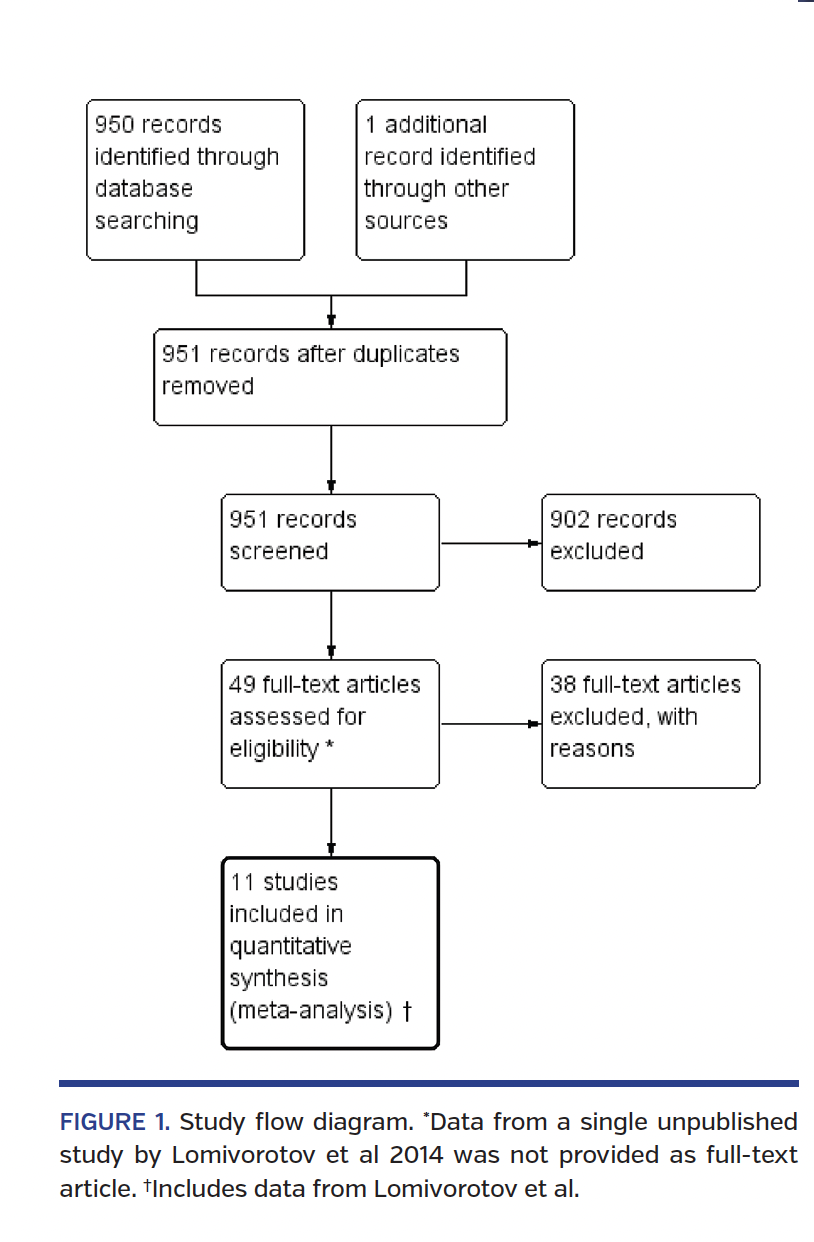
A subgroup analysis was conducted examining the use of sunscreen in a high-risk (all White) population (Table 2). The net present value cost for frequent, some, and no sunscreen in this subgroup was $1456, $1544, and $1219, respectively. The incremental benefit in QALYs was 0.046 for frequent sunscreen as compared to no sunscreen, resulting in an ICER of $5220/QALY. Frequent sunscreen was always the dominant strategy compared to some sunscreen.
Sensitivity Analyses Results
In one-way sensitivity analyses, the key drivers of the model were the cost of sunscreen, probability of melanoma continuing beyond a year, and the cost of metastatic melanoma (due to treatment costs; Supplemental Figure 1). A cost-effectiveness scatterplot based on sensitivity analyses of the three intervention arms demonstrates that frequent sunscreen use is the most effective intervention but is associated with slightly higher costs (Figure 2). Some sunscreen use was less effective but less costly. No sunscreen use is the least effective and least costly intervention.
Notably, in 1000 simulation probabilistic sensitivity analysis, the ICER for frequent sunscreen use ranged from frequent sunscreen being the dominant therapy (more effective and less costly) to $41,338/QALY (still under the acceptable threshold for medical interventions). The likelihood that frequent sunscreen use was the dominant strategy over no sunscreen use was ~10% (113/1000 points in Quadrant IV). The remaining 90% of the time (887/1000 points in Quadrant I), frequent sunscreen use represented a favorable trade-off between increased clinical efficacy and somewhat elevated costs (Figure 3). No sunscreen use was never the dominant strategy.
Additionally, sensitivity analyses were performed for each of the variables used in our model including frequency of sunscreen usage, White vs non-White ethnicity, gender, and tanning bed use >10 or <10. Sensitivity analyses revealed that our model was not sensitive to variations in any of these characteristics.
Discussion
Our model focuses on the NYS Medicaid population and suggests that coverage of sunscreen for their pediatric beneficiaries could be a cost-effective strategy to reduce the lifetime burden of melanoma. It is especially important that health systems incorporate the barriers and challenges that patients face in the decision of whether to include a given treatment on a clinical pathway meant to improve care while lowering costs. Currently, the price of sunscreen may be prohibitive to many lower socioeconomic status families, but a large government health insurer like NYS Medicaid has the ability to make this photoprotective strategy accessible to ~2.5 million children.15
The cost of melanoma treatment is estimated to range from $5879/year for local melanoma to $219,536/year for metastatic melanoma (Table 1). While local melanoma costs remain stable, targeted and immunological agents are a new addition to the treatment paradigm, significantly increasing the costs of treatment. Primary prevention strategies such as the use of regular sunscreen use provide a cost-effective alternative. The ICER of frequent sunscreen use is $8225/QALY, which is far below the $150,000/QALY cost-effectiveness threshold, or willingness-to-pay, for many other medical interventions, and leads to a gain of 0.04 QALYs (Table 2). For comparison, statins, ubiquitous cholesterol-lowering drugs that are routinely provided by health insurers, are estimated to have an ICER of $33,495/QALY for a gain of 0.26 QALYs.16
The most significant obstacle to the implementation of this strategy is the high price of sunscreen at the individual level. However, a large government organization like Medicaid has the ability to obtain affordable sunscreen at discount rates using a competitive bidding strategy, whereby manufacturers provide substantial discounts in return for the exclusive right to provide their product to organization participants. The
purchasing power of large government organizations for nonpharmaceutical items has been exemplified successfully by the Supplemental Nutrition Assistance Program (SNAP), School Meals, Women, Infants and Children (WIC) programs,17 and Medicare.18 Using this same strategy, we believe Medicaid could drive current market prices down, obtaining and providing high-quality sunscreen at a discounted cost of $60 to $120/year/child on average. In addition, pediatricians would also play a key role in ensuring that sunscreen is used on its intended recipient, the child, and prevent misappropriation of this resource. Pediatricians, who will likely be the primary sunscreen gatekeepers, will be responsible for prescribing the resource and administering subsequent refills. Parents who place refill requests inappropriately quickly or too slowly may be misappropriating or underusing the resource. Regular check-ins, collecting a detailed history of exposure and travel, assessing patient size and growth, discussions with both child and parent, and education on proper sunscreen use will be important tools in these situations.
Critics of primary prevention interventions may argue that the cost of preventive medicine to such a large population outweighs the benefits of reduction in disease incidence. However, a recent cost-effectiveness study of sunscreen usage in a middle-aged Australian population revealed that regular sunscreen use for 30 years leads to a 38.7% reduction in melanoma deaths vs 30 years of annual whole-body skin examinations, while saving £107.1million in combined health care and societal costs.19 Additionally, specific to this intervention, they might argue that people of non-White descent rarely get melanoma (0.1% for African Americans vs 2.6% for Caucasians20) or are more likely to present with less UV-dependent subtypes, thus not benefitting from sunscreen use. However, while the overall incidence of skin cancer is relatively low in people with skin of color, skin cancer in this population tends to present atypically or at more advanced stages and thus carry a worse prognosis.21,22 When Blacks and Hispanics develop melanoma, they have been consistently shown to have worse 5-year survival rates than Whites (65% for Black patients vs 91% for Whites).23 This difference is largely due to late detection, but an important factor is the misconception that having darker skin confers complete protection against UV rays. While increased melanin in the skin is protective, there is considerable heterogeneity in skin of color. However, like non-Hispanic Whites, people with darker skin experience sunburn, an irrefutable sign of UV damage and proof that all colors of skin require photoprotection. Furthermore, it is predicted that by 2050, 50% of the US population will be Black, Hispanic, or Asian,24 making it crucially important to provide all groups access to photoprotective tools. We suggest that a discussion with the child’s pediatrician may inform and guide usage of this resource.
In our NYS Medicaid model, 32% of enrollees are White, 22% are Black, 28% are Hispanic, and 18% are other.8 In comparison, other states have as many as 98% White enrollees (eg, Idaho). Indeed, when we performed subgroup analysis to the high-risk white NYS pediatric population, the ICER lowered to $5220/QALY (Table 2). These findings suggest that
Medicaid coverage of sunscreen in other states might likewise show even greater effects at lower costs. These findings underscore the importance of making this resource available to all lower socioeconomic status families.
Additional primary prevention strategies, including education and public health campaigns, used in conjunction with financial coverage of sunscreen, may provide optimal benefit in skin cancer prevention.25 Australia was the first country to successfully implement public health campaigns to reduce the incidence of skin cancer and associated deaths. SunSmart was launched in Australia in 1988 to reduce skin cancer incidence, morbidity, and mortality through a prevention and early detection program. It promotes sun-safe behaviors including use of protective clothing, applying broad-spectrum SPF 30+ sunscreen, avoiding the sun during midday, using shade, and avoiding indoor tanning. This campaign was highly successful and prevented nearly 50,000 cancers and 1400 deaths from skin cancer between 1988 and 2011 with a net savings of $92 million.26 Similarly, sun safety and educational programs have been implemented in the United States. Ray and the Sunbeatables: A Sun Safety Curriculum was initiated by the MD Anderson Cancer Center to teach them sun safe behaviors to young children, parents, and teachers.27 Outcomes of these programs will be followed in the decades to come. Furthermore, authorities at daycares, elementary schools, and high schools can play an important role in the dispersal of this resource in the intended population while also providing education on correct use. Research has shown that schools are an underutilized resource for sun prevention that could benefit from state-sponsored programs that encourage sun-safe behaviors.28
Today, the importance of sunscreen has been gaining attention in health care organizations. The Veterans Health Administration (VHA), a federal government organization, currently allows medical providers to prescribe six different sunscreens with varying SPF coverage and active ingredients.29 Sunscreen is a reimbursable expense via Flexible Spending Accounts (FSA) and Health Spending Accounts (HSA) for employee-sponsored health plans.30 However, while commendable, these policies are limited in scope. For instance, the VHA primarily treats an older population and generally does not cover children and adolescents. Likewise, FSAs and HSAs insure populations that have some disposable income, whereas Medicaid could
provide for those who cannot afford sunscreens routinely.
There are a multitude of other preventive tools that have the potential to significantly impact health and quality of life. For example, providing nutritional food, exercise equipment, housing, and transportation may positively affect long-term health outcomes. That said, due to budget restrictions, it is reasonable that government health care organizations limit coverage to treatments, medications, and related items that can be found in a pharmacy. Moving forward, focusing on external factors such as the social determinants of health as well as access to care and resources must be taken into account when developing patient-centered clinical pathways.31 Given the importance of preventive care, other government branches such as housing or transportation services may also find subsidizing additional services is cost-effective and beneficial for public health. Cost-effectiveness analyses such as the model described above are an important tool for deciding if a currently non-covered treatment should be included in clinical pathways.
Potential Limitations
Potential limitations in our analysis relate to certain parameters for which data are limited. For instance, we began our intervention at age 3 years which is the earliest age for which sunscreen use data was available in Watts et al.5 Younger children may also utilize other sun-protective measures (clothing, hats, etc), spend more time indoors and in the shade, and have a much smaller body surface area, minimizing their sun exposure in infancy. However, in practice, children younger than 3 years should also be offered this benefit as their skin is especially vulnerable and it is important to establish healthy behaviors and practices as early as possible.
Additionally, our model does not differentiate between subtypes of melanoma, and includes subtypes such as acral lentiginous melanoma (ALM) and mucosal melanoma. These subtypes occur in areas which receive less UV exposure and therefore may be less affected by sunscreen application.32 Limited data has been published regarding the impact of sunscreen on these subtypes. However, the overall incidence of these subtypes is very low. For instance, ALM occurs in 1.8/1,000,000 in Blacks and 2.6/1,000,000 in non-Hispanic Whites.33 Thus, these rare, non-UV dependent melanomas overall comprise a very small fraction of the total number of melanomas and thus their inclusion negligibly impact the results of our model.
Another limitation of the model is the lack of information on nonmelanoma skin cancers (NMSCs) and atypical nevi as they are not required to be reported in contrast to melanomas. If the cost of monitoring and treating NMSCs/atypical nevi were included in the model (an additional $4.8 billion/year), this intervention may
significantly increase the value of using sunscreen.
Conclusion
Nationwide, more than 35 million children are insured by Medicaid.15 Providing sunscreen to these children has the potential to be an impactful primary prevention measure to reduce melanoma morbidity and combat rising health care costs. In our model, frequent sunscreen use will lead to an increase in QALYs for enrollees and is a cost-effective intervention. Based on these findings, we recommend adoption of sunscreen coverage by Medicaid. This policy change has the ability to prevent skin cancer by encouraging sunscreen use and compliance especially in younger populations, halting the rising rates and costs of treating melanoma associated with UV exposure.
Supplementary materials cited in this piece can be found with the online PDF of this article.
References
1. American Cancer Society. Cancer Facts and Figures. cancer.org. Published 2019. Accessed March 22, 2021. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2019.html
2. Reed KB, Brewer JD, Lohse CM, Bringe KE, Pruitt CN, Gibson LE. Increasing incidence of melanoma among young adults: an epidemiological study in Olmsted County, Minnesota. Mayo Clin Proc. 2012;87(4):328-334. doi:10.1016/j.mayocp.2012.01.010
3. Chen JT, Kempton SJ, Rao VK. The economics of skin cancer: an analysis of Medicare payment data. Plast Reconstr Surg Glob Open. 2016;4(9):e868. doi:10.1097/GOX.0000000000000826
4. Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol. 2011;29(3):257-263.
5. Watts CG, Drummond M, Goumas C, et al. Sunscreen use and melanoma risk among young Australian adults. JAMA Dermatol. 2018;154(9):1001-1009. doi:10.1200/JCO.2010.28.7078
6. Johal R, Leo MS, Ma B, Sivamani RK. The economic burden of sunscreen usage. Dermatol Online J. 2014;20(6):13030/qt6v0352fw.
7. Fears TR, Scotto J, Schneiderman MA. Mathematical models of age and ultraviolet effects on the incidence of skin cancer among whites in the United States. Am J Epidemiol. 1977;105(5):420-427. doi:10.1093/oxfordjournals.aje.a112400
8. Kaiser Family Foundation. Medicaid & CHIP Indicators. kff.org. Accessed March 22, 2021. https://www.kff.org/state-category/medicaid-chip/
9. Health NYSDo. Table 1: Estimated Population by Age, Sex and Region, New York State – 2016. Updated May 2018. Accessed March 22, 2021. https://www.health.ny.gov/statistics/vital_statistics/2016/table01.htm
10. Guy GP Jr, Machlin SR, Ekwueme DU, Yabroff KR. Prevalence and costs of skin cancer treatment in the U.S., 2002-2006 and 2007-2011. Am J Prev Med. 2015;48(2):183-187. doi:10.1016/j.amepre.2014.08.036
11. NCCN Guidelines for Patients, Melanoma. Published 2018. Accessed March 22, 2021. https://www.nccn.org/patients/guidelines/melanoma/files/assets/common/downloads/files/melanoma.pdf
12. Kandel M, Allayous C, Dalle S, et al. Update of survival and cost of metastatic melanoma with new drugs: Estimations from the MelBase cohort. Eur J Cancer. 2018;105:33-40. doi:10.1016/j.ejca.2018.09.026
13. Current Discount Rates. Federal Reserve; Discount Window/Payment System Risk. Accessed March 22, 2021. https://www.frbdiscountwindow.org/Pages/Discount-Rates/Current-Discount-Rates.aspx
14. Institute for Clinical and Economic Review Releases Final Value Assessment Framework for 2017 - 2019. Accessed March 22, 2021. https://icer.org/news-insights/press-releases/vaf-update-2017-2019/
15. September 2020 Medicaid & CHIP Enrollment Data Highlights. Accessed March 22, 2021. https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html
16. Lin L, Teng M, Zhao YJ, et al. Long-term cost-effectiveness of statin treatment for primary prevention of cardiovascular disease in the elderly. Cardiovasc Drugs Ther. 2015;29(2):187-197. doi:10.1007/s10557-015-6584-7
17. Carlson S, Greenstein R, Neuberger Z. WIC’s competitive bidding process for infant formula is highly cost-effective. Center on Budget and Policy Priorities. Updated February 17, 2017. Accessed March 22, 2021. https://www.cbpp.org/sites/default/files/atoms/files/6-26-15fa.pdf
18. Center for Medicare & Medicaid Services. Medicare’s DMEPOS Competitive Bidding Program. April 2013. Accessed March 22, 2021. https://www.cms.gov/outreach-and-education/outreach/partnerships/downloads/dmepospartnerfaqsrevised4813508.pdf
19. Gordon L, Olsen C, Whiteman DC, Elliott TM, Janda M, Green A. Prevention versus early detection for long-term control of melanoma and keratinocyte carcinomas: a cost-effectiveness modelling study. BMJ Open. 2020;10(2):e034388. doi:10.1136/bmjopen-2019-034388
20. Apalla Z, Lallas A, Sotiriou E, Lazaridou E, Ioannides D. Epidemiological trends in skin cancer. Dermatol Pract Concept. 2017;7(2):1-6. doi:10.5826/dpc.0702a01
21. Bradford PT. Skin cancer in skin of color. Dermatol Nurs. 2009;21(4):170-177, 206; quiz 178.
22. Projections of the resident population by race, Hispanic origin, and nativity: middle series, 2025 to 2045. Population Projections Program, Population Division, US Census Bureau. January 13, 2000. Accessed March 22, 2021. https://www2.census.gov/programs-surveys/popproj/tables/2000/2000-national-summary-tables/np-t5-f.pdf
23. c2019 Pharmacy Benefits Management Services. U.S. Department of Veterans Affairs. Accessed March 22, 2021. https://www.pbm.va.gov/nationalformulary.asp
24. Eligible Health Care FSA (HC FSA) Expenses. US Office of Personnel Management. Accessed March 22, 2021. https://www.fsafeds.com/explore/hcfsa/expenses
25. Trager MH, Queen D, Samie FH, Carvajal RD, Bickers DR, Geskin LJ. Advances in prevention and surveillance of cutaneous malignancies. Am J Med. 2020;133(4):417-423. doi:10.1016/j.amjmed.2019.10.008
26. Shih STF, Carter R, Heward S, Sinclair C. Skin cancer has a large impact on our public hospitals but prevention programs continue to demonstrate strong economic credentials. Aust N Z J Public Health. 2017;41(4):371-376. doi:10.1111/1753-6405.12679
27. MD Anderson joins CATCH Global Foundation to boost child health, prevent cancer in later years. News release. MD Anderson Cancer Center; February 18, 2015. Accessed March 22, 2021. https://www.mdanderson.org/newsroom/md-anderson-joins-catch-global-foundation-to-boost-child-health-.h00-158985078.html
28. Everett Jones S, Guy GP Jr. Sun safety practices among schools in the United States. JAMA Dermatol. 2017;153(5):391-397. doi:10.1001/jamadermatol.2016.6274
29. Stern RS. Prevalence of a history of skin cancer in 2007: results of an incidence-based model. Arch Dermatol. 2010;146(3):279-282. doi:10.1001/archdermatol.2010.4
30. Thieden E, Philipsen PA, Sandby-Møller J, Heydenreich J, Wulf HC. Proportion of lifetime UV dose received by children, teenagers and adults based on time-stamped personal dosimetry. J Invest Dermatol. 2004;123(6):1147-1150. doi:10.1111/j.0022-202X.2004.23466.x
31. Stefanacci RG, Guerin S. Truly patient-centered clinical pathways. J Clin Pathways. 2017; 3(6);42-43.
32. Hoppe RT, Phillips TL, Roach M. Leibel and Phillips Textbook of Radiation Oncology. 3rd ed. Saunders; 2010:1459-72.
33. Bradford PT, Goldstein AM, McMaster ML, Tucker MA. Acral lentiginous melanoma: incidence and survival patterns in the United States, 1986-2005. Arch Dermatol. 2009;145(4):427-434. doi:10.1001/archdermatol.2008.609

















