Prescribing Considerations for Antithrombotic Prophylaxis
Nashville—Disorders that require antithrombotic and antiplatelet therapies are prevalent in long-term care (LTC), but determining the best course of prophylaxis treatment is complicated by the proliferation of new agents and an evolving evidence base.
During an educational session at the AMDA conference, Thomas Lynch, PharmD, department of family and community medicine, Eastern Virginia Medical School, Norfolk, Virginia, and Thomas Grant, MD, department of family and community medicine, Eastern Virginia Medical School, Norfolk, Virginia, discussed updates in current best practices in anticoagulant and antiplatelet therapy and reviewed the “use, misuse, and pitfalls” of the new agents.
Antiplatelet Drugs
Antiplatelet drugs are indicated for the prevention of acute coronary syndrome (ACS), including unstable angina and ST-segment elevation myocardial infarction (STEMI), secondary prevention of stroke, prevention of stroke secondary to atrial fibrillation (AF), treatment of unstable angina, STEMI, non-STEMI, and following coronary stent placement, said Dr. Grant.
Aspirin
Aspirin, or acetylsalicylic acid, is a nonsteroidal anti-inflammatory agent that irreversibly inhibits platelet function. Specifically, it causes inhibition of cyclooxygenase-1, which prevents synthesis of thromboxane A2 by platelets, thereby preventing platelet recruitment. The usual prophylactic dose is 81 mg, and acetylsalicylic acid is used for angina, post-myocardial infarction, and secondary prevention of stroke.
Dipyridamole
Dipyridamole is most often prescribed at a dose of 200 mg with 25 mg acetylsalicylic acid twice daily. It inhibits platelet function by inhibiting platelet phosphodiesterase and increasing plasma adenosine levels, thus increasing intracellular concentrations of cyclic adenosine monophosphate. A treatment drawback is that headache occurs in 40% of patients due to vasodilation. Dr. Lynch noted that dipyridamole is only slightly more effective than aspirin alone, yet it costs about $300 a month. Because it has to be taken twice daily, adherence is an issue.
Thienopyridines
Thienopyridines irreversibly inhibit P2Y12 adenosine diphosphate (ADP) receptors. Clopidogrel, which is available as a generic, is the most widely used thienopyridine, and prasugrel is another example. These drugs are administered orally once daily. Clopidogrel can be used in patients who cannot tolerate acetylsalicylic acid, or it can be used with low-dose acetylsalicylic acid after ACS or stent replacement for up to 1 year. Dr. Lynch cautioned that the bleeding risk is greater when clopidogrel is combined with acetylsalicylic acid compared with either drug alone. Clopidogrel must be discontinued at least 5 days before surgery due to high bleeding risks. Adverse events associated with treatment may include bleeding and purpura. Clopidogrel is dosed at 75 mg daily after a loading dose of
300 mg to 600 mg.
According to Dr. Lynch, clopidogrel, a prodrug, is controversial because metabolism can be affected by inhibitors or inducers of CYP 2C19 and polymorphisms, which occur in 5% of whites and blacks and 20% of Asians. The FDA recommends genotyping patients for CYP 2C19 alleles to predict poor response. Updated guidelines recommend alternative therapy in individuals with ACS or high-risk percutaneous coronary intervention (PCI) who are poor or intermediate metabolizers.
He noted that, theoretically, clopidogrel could fail if combined with omeprazole, esomeprazole, or lansoprazole, although data from prospective trials are conflicting. For patients with dyspepsia and mild gastroesophageal reflux disease, H2 antagonists (except cimetidine) rather than a proton pump inhibitor (PPI) should be used. PPIs should be used for cases involving severe bleeding on clopidogrel. Dr. Lynch said the preferred PPI is pantoprazole.
Prasugrel is similar in structure and mechanism of action to clopidogrel. Although it is also a prodrug, it has a low risk of interactions with PPIs due to its metabolic pathway. Prasugrel is only indicated in combination with acetylsalicylic acid for the prevention of post-PCI events in ACS patients. The drug also carries a Black Box Warning for significant bleeding risk. It is contraindicated in individuals with a history of stroke, transient ischemic attack, and individuals >75 years of age. Treatment must be started during hospitalization, and the drug is expensive, costing approximately $280 per month.
Ticagrelor
Ticagrelor is a reversible inhibitor of P2Y12 ADP receptor. It works faster with more consistent inhibition of receptors than clopidogrel. The drug is indicated for ACS and unstable angina. Ticagrelor carries a Black Box Warning that it should be used with acetylsalicylic acid only at doses <100 mg. It also has significant drug interaction potential since it is predominantly metabolized by CYP3A4. Therefore, strong inhibitors and inducers of CYP3A4 should be avoided. Dr. Lynch noted that adherence is a potential problem because of the twice daily dosing. Also, the cost is high at $130 per month.
New Oral Anticoagulants
For the prevention of stroke in nonvalvular AF, dabigatran, rivaroxaban, and apixaban are FDA-approved agents in this class. Only rivaroxaban is approved for deep vein thrombosis (DVT) prophylaxis after hip and knee replacement, for DVT and/or pulmonary embolism (PE) treatment, and for the reduction of risk of DVT or PE recurrence. Apixaban was approved for prophylaxis of DVT in patients who have undergone hip or knee replacement surgery.
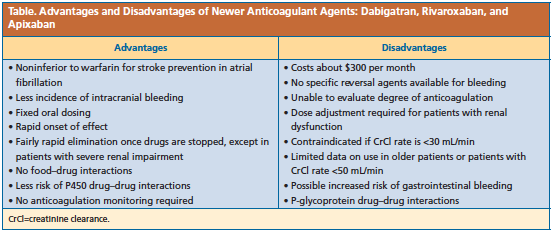
Whereas the existing data are limited by small numbers of older patients included in clinical trials, general advantages and disadvantages of the new agents compared with warfarin have been identified (Table).
Advantages of dabigatran include its ability to be dialyzed and that it does not inhibit or induce metabolism of other medications by P450. Disadvantages include twice-daily dosing, reduced bioavailability with achlorhydria, and increased bioavailability of 75% if capsules are chewed or broken. Advantages of rivaroxaban include once-daily dosing and indication for the treatment and prevention of DVT.
The disadvantages include different doses and dosage forms depending on indication and a Black Box Warning of increased risk of thrombotic stroke if discontinued. The drug interaction potential for these oral anticoagulants should also be considered before prescribing.
Dabigatran and rivaroxaban should be avoided if creatinine clearance (CrCl) rate is <30 mL/min, and apixaban should be avoided if CrCl rate is <25 mL/min.—Eileen Koutnik-Fotopoulos