ADVERTISEMENT
Specialty Pharmacy and the ACO Model
Tampa—“[Accountable care organizations (ACOs)] are here; they have arrived. We have to deal with them,” said Mike Baldzicki, CRCM, executive vice president, industry relations & advocacy, Armada Health Care, during a session at the AMCP specialty pharmacy conference.
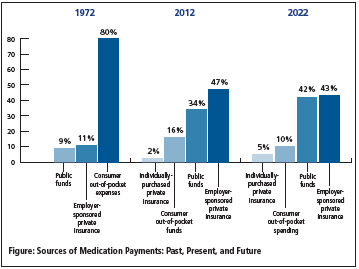
Because of the expanding coverage in both Medicaid and the health insurance exchanges, payment and delivery reforms, including ACOs, are rendered necessary. In addition, the specialty market is becoming sizeable, with 40% of products in the pharmaceutical pipeline categorized as specialty. By 2016, it is estimated that 50% of the top 100 drugs and 8 of the top 10 drugs will be specialty pharmaceuticals. Mr. Baldzicki shared information that showcased how drugs have been paid for in the past, are currently paid for, and how payment is projected for the future (See Figure below).
Currently, there are 488 ACOs in the United States, of which 253 have contracts with the Centers for Medicare & Medicaid Services. More than 40% of Americans live in an area with at least 1 ACO, and as of February 2013, ACOs covered 37 million to 43 million Medicare and commercial patients, according to an Oliver Wyman report. Mr. Baldzicki noted that private payers are also engaging in ACOs, including Cigna, UnitedHealthcare, Aetna, Humana, and WellPoint.
Hospital providers, however, need a new business model for financial sustainability. Due to recent payment reforms, hospitals need to change the way they are thinking about medication spending. Due to reductions in payment, increases in transparency, transfers of risk, and changes in volume and access to care, hospitals will need to aggregate and capture data, work closely with physicians, become responsive to different payment models, select and comply with a core set of clinical guidelines, focus on costs, and identify partners who can offer integrated solutions.
ACOs can help hospitals to leverage the most costly components of healthcare delivery for a lower cost, develop an alternative revenue stream and benefit from risk sharing with lower costs, solidify partnerships with physician groups, develop partnerships with healthcare insurers to increase marketshare of hospital days, and scale ACO concepts to accommodate the cost of the infrastructure buildout.
Mr. Baldzicki noted the “triple aim” of ACOs: (1) reduce costs; (2) increase quality; and (3) improve health in the community at large. These key qualities of the ACO model can help when it comes to specialty medications.
Mr. Baldzicki said the specialty pharmacy channel needs to improve quality and value, and can do so with 3 simple goals: (1) improving the efficiency and appropriateness of biotechnology drug dispensing; (2) reducing costs resulting from inappropriate utilization and billing errors with biotechnology drugs; and (3) improving data capture and the measurement of total healthcare costs and outcomes.
According to the presentation, the following recommendations are beneficial to the health system: (1) manufacturers must demonstrate the value of their medicines through health technology partnerships, payers, hospitals, and ACOs; (2) specialty programs must improve patient compliance and ensure diagnostic criteria is met prior to receiving treatment; (3) emerging drug-delivery technologies will drive changes in benefit designs; (4) more drugs have Risk Evaluation and Mitigation Strategy programs, including patient education, compliance, clinical checkup reminders, and managing side effects; and (5) pharmacy benefit managers need to continue to integrate the medical and pharmacy claims data.