Prescriber Intervention Program Helps Identify Opioid Abuse
Tampa—Analysis conducted by investigators at the Centers for Disease Control and Prevention in 2013 found that 75.2% of pharmaceutical deaths involved opioids, either alone or in combination with other drugs. Other data from the National Center for Health Statistics show that drug overdose deaths increased for the 11th consecutive year in 2010, an increase largely driven by opioid analgesics.
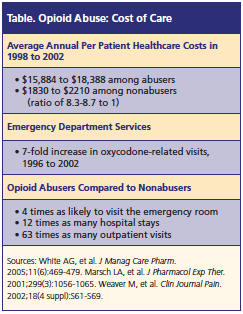
Furthermore, the scope of opioid abuse in the insured population has a significant affect on cost of care (See Table below), according to a session at the AMCP meeting. Session speakers Paul DuBose, PhD, vice president, analytics, Principled Strategies Inc., and Saira Jan, MS, PharmD, director of clinical pharmacy management, Horizon BlueCross BlueShield of New Jersey, reported the outcomes of a multiyear SafeUseNow pilot program designed to reduce behaviors associated with avoidable medical services and costs. The pilot program was first introduced at AMCP’s 2013 meeting.
SafeUseNow Program Details
The SafeUseNow program was designed with a prescriber-centric approach to augment patient-focused efforts already in place. The goals of the program include:
• Identify prescriber factors of inappropriate prescribing
• Coordinate care with behavioral health case managers
• Provide education and resources prescribers perceive as valuable
• Safe use of opioids for patients who require treatment for pain
• No abandonment of “difficult” patients
SafeUseNow has developed a PSI Score, an algorithm based on an advanced analytic model that evaluates prescriber and patient behavior contributing to the risk of misuse, abuse, addiction, and diversion of controlled substances. The score is a prescriber-specific aggregate of 17 behavioral risk factors observed in the prescriber’s patients’ prescription data. Each prescriber’s risk is determined relative to all other prescribers and specialty peers. The PSI score is then used to predict risky prescribers by identifying those who are trending upward. This enables managed care organizations to identify prescribers whose prescribing behaviors may contribute to prescription drug abuse.
Understanding Program Results
In the initial results of the PSI Score, 1200 prescribers were identified for engagement at or above 98th percentile of the PSI Score distribution. The top 3 risk factors (occurring most frequently among prescribers’ top 3 risk factors) were early refills of similar products, excessive use of controlled substances, and dosage and volume of opioids.
“When a prescriber has a high PSI Score, it is likely that there are actions that the prescriber is not doing that they can do to reduce risk and improve patient safety,” according to the session presentation. “The higher the risk level, the greater the opportunity to improve patient safety.”
SafeUseNow interventions for at-risk prescribers included engagement, consultation, and ongoing follow-up. The engagement packet included a welcome letter, risk factor worksheets, clinical advisories specific to each prescriber’s top 3 risks factors, and patient information report. The consultation included 20- to 30-minute 1-on-1 consultation with a PharmD trained in the program protocol either via telephone or office visit. Ongoing follow-up included satisfaction survey within 2 weeks of the appointment, monthly communications (eg, brief survey questions), and quarterly updates on PSI Scores and top 3 risk factor scores.
The speakers highlighted results from each intervention. During the engagement phase, all prescribers who were contacted acknowledged a need to address controlled substances, noting that inclusion of detailed prescription information for the prescriber’s own patients was a major contributor to prescribers’ willingness to participate. For the intervention phase, most prescribers read the engagement before the appointment. While most prescribers expressed concern about being “monitored” by the payer, this resulted in high motivation to discuss the program. Furthermore, when the pharmacist reviewed the program themes, the prescribers’ comfort and collaboration increased.
When pharmacists followed up with prescribers, they learned that many prescribers believed they were already implementing adequate steps and precautions in their practice. Also, many providers where not aware of additional resources and tools to help improve the safe use of controlled substances, such as specific lab tests and referrals for addiction specialists and psychological counseling. The prescriber feedback also highlighted challenges with pain management clinics and centers. For example, the speakers noted that many primary care providers expressed a low comfort level with managing chronic pain patients, but felt they were “left with no other choice.”
Clinical Outcomes
The session concluded with clinical outcomes of the SafeUseNow program. Monthly updates to the PSI Score and risk factor scores enabled the program to:
• Measure change across the prescriber population within each specialty group
• Indirectly measure adoption of clinical recommendations
• Identify prescriber trends as they develop, permitting early-stage intervention per prescriber and the population
• Receive continuous feedback to evaluate the program impact and improve effectiveness
SafeUseNow used a fixed effects panel regression method to determine various risk factor (eg, PSI Score, multiple healthcare providers, multiple pharmacies, and concomitance) and utilization factor (eg, opioid prescription claims and morphine equivalent dose [mg]) end points. Data showed that the cumulative 12-month savings for 1125 prescribers for opioid prescription claims was $2,596,189; and the cumulative 12-month savings for 1125 prescribers for other nonopioid prescription claims was $461,731. For more information, visit www.safeusenow.com.