Overuse of EGD Observed in Medicare Patients
Esophagogastroduodenoscopy (EGD), once primarily used in a specialized setting, has become an effective procedure in evaluating common symptoms, such as abdominal pain and dysphagia. The expansion of EGD has resulted in the potential overuse of the procedure, in turn increasing patient risk and causing a burden on healthcare resources, according to a recent study [Ann Intern Med. 2014;160:154-160].
The Choosing Wisely® campaign, sponsored by the American Board of Internal Medicine, addresses the general concern of overuse, considered to be the most important contributor to the high cost of US healthcare spending. Overuse of EGD is recognized by the American College of Physicians and the American Gastroenterological Association, both of which have made efforts to minimize the issue.
The study sought to examine the proportion of patients who had ≥1 repeated EGD examination. The test group focused on 103,711 beneficiaries who received Medicare between 2004 and 2009 (excluding patients enrolled in Medicare Part A only or a risk-contract health maintenance organization), were alive for the entire 6-year study period, and underwent their first EGD—referred to as the index EGD—prior to December 31, 2006, to ensure a 3-year follow-up period.
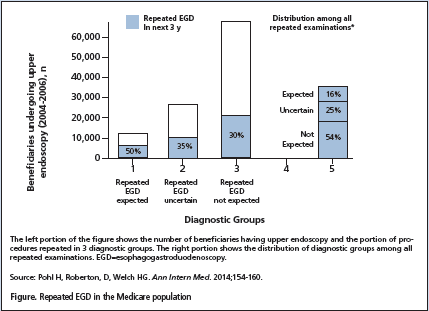
The 103,711 patients were classified into 3 categories: (1) repeated EGD was expected (n=11,370); (2) EGD was uncertain (n=26,034); or (3) EGD was not expected (n=66,307). These classifications were based on the diagnosis of the index EGD. Further analysis focused on patients who received a repeated examination but were classified as a repeated EGD not expected. Of the total number of repeated examinations, 54% were of individuals from the EGD not expected category (Figure - Below).
Within this subgroup of patients, 2 scenarios occurred: (1) the index and repeated EGD resulted in the same diagnosis; or (2) the patient developed a new clinical problem validating the repeated examination. Of the 19,687 patients who unexpectedly had a repeat examination, 32% had the same diagnosis as that of the index EGD. A new diagnosis was found in 20% of these patients. Overall, 43% of repeated EGDs were performed in patients that did not have a diagnosis at initial or repeated endoscopy that justified a repeated procedure.
To further evaluate EGD overuse, the researchers considered 2 broad categories: (1) the procedure was being performed on too many patients; and (2) the procedure was repeated too often on the same patients. While the study focused on overuse of EGD, there was an observed underuse of the procedure as well. Only 58% of patients with Barrett esophagus and 60% of patients with varices—2 EGD diagnoses in which a repeated procedure was expected—had a repeated examination.