Managing Charcot Foot
San Francisco—Charcot foot is a significant complication that individuals with diabetes develop in relation to peripheral neuropathy of the foot. Research has shown that Charcot foot is a commonly missed diagnosis. During a symposium at the ADA meeting, a panel of world-renowned experts described the clinically challenging condition and the benefits of early diagnosis.
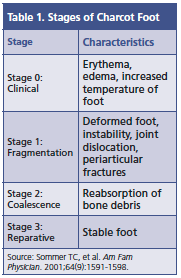 A study by Rogers et al, published in Diabetes Care in 2012, defined Charcot foot, also known as neuropathic osteoarthropathy, as a condition affecting the bones, joints, and soft tissues of the foot and ankle, characterized by inflammation in the earliest stage (Table 1). Along with diabetes, tabes dorsalis, traumatic disease of the spine, trauma to the nerve roots, leprosy, alcohol associated neuropathy, and syringomyelia are conditions complicated by Charcot foot, according to William J. Jeffcoate, MRCP, foot ulcer trials unit, department of diabetes and endocrinology, Nottingham University Hospitals Trust.
A study by Rogers et al, published in Diabetes Care in 2012, defined Charcot foot, also known as neuropathic osteoarthropathy, as a condition affecting the bones, joints, and soft tissues of the foot and ankle, characterized by inflammation in the earliest stage (Table 1). Along with diabetes, tabes dorsalis, traumatic disease of the spine, trauma to the nerve roots, leprosy, alcohol associated neuropathy, and syringomyelia are conditions complicated by Charcot foot, according to William J. Jeffcoate, MRCP, foot ulcer trials unit, department of diabetes and endocrinology, Nottingham University Hospitals Trust.
Although there is no singular cause for the development of Charcot foot, there are factors that predispose individuals to its development in addition to precipitating factors. “Neuropathy is a prerequisite, and then there is an often recognized trigger,” said Dr. Jeffcoate, who cited a study by Game et al published in Diabetologia in 2012 that found 36% of patients experienced trauma to the foot in the preceding 6 months, 12% had surgery to the affected foot, 35% had an ulcer on the affected limb, and 7% had osteomyelitis.
Challenges of Diagnosis
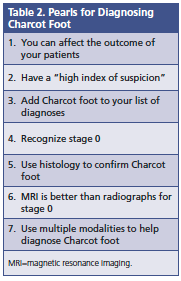 Diagnosing Charcot foot is a challenge, and a majority of the time the diagnosis is missed. Crystal Murray Holmes, DPM, CWS, clinical assistant professor of medicine, University of Michigan Medical School, outlined 7 practical clinical pearls to diagnosing Charcot foot (Table 2).
Diagnosing Charcot foot is a challenge, and a majority of the time the diagnosis is missed. Crystal Murray Holmes, DPM, CWS, clinical assistant professor of medicine, University of Michigan Medical School, outlined 7 practical clinical pearls to diagnosing Charcot foot (Table 2).
She said Charcot foot can be preventable if recognized early. However, it goes undiagnosed by the referring physician 95% of the time, prior to referral to a foot clinic. She referenced a study by Wukich et al published in Diabetic Medicine in 2011 that showed Charcot foot diagnosed at more than 8 weeks post-onset was associated with a 67% complication rate, but Charcot foot identified within 4 weeks had a complication rate of only approximately 14%.
Dr. Holmes noted that literature on Charcot foot underscores the importance of clinicians having a high index of suspicion. When a patient has a red, hot, swollen foot that has peripheral neuropathy, Charcot foot is a diagnosis that needs to be considered.
Clinicians also need to be aware of the risk factors for Charcot foot. Dr. Holmes highlighted a study by Stuck et al that found that obesity, peripheral neuropathy, older age, diabetes duration >6 years, hemoglobin A1c >7%, renal failure, arthritis, and anemia were associated with an increased incidence of Charcot foot. She noted 2 additional risk factors, osteopenia in both type 1 and type 2 diabetes and end-stage renal disease, that are especially common in the setting of renal transplant and renal pancreatic transplant, which should be included as risk factors.
Dr. Holmes told attendees, when thinking about Charcot foot, “Never forget the basic clinical signs or the basic science behind it. ”
Surgical Management of Charcot Foot
George Liu, DPM, FACFAS, assistant professor, University of Texas Southwestern Medical Center, who discussed surgical management of Charcot foot, said it is an intriguing problem because it “involves rapid joint destruction, severe deformity accompanied with instability that leads to ulcerations, and subsequent chronic disability.”
He noted that Charcot foot increases the likelihood for foot and ankle ulceration and, if left untreated, it can lead to an infection, which ultimately may call for amputation. “Ulceration is the pivotal event that allows a patient to be at risk for a limb loss.”
The consensus for initial treatment of acute Charcot foot is nonoperative treatment with strict nonweight-bearing immobilization to prevent further deformity. However, sometimes conservative management is not enough. Surgical intervention is indicated for nonplantigrade, unstable, deformed foot and ankle. Dr. Liu said rigid deformities cannot be offloaded and unstable deformities cannot be braced. He referenced a study by Armstrong et al in Diabetes Care in 1997 that found 25% of patients with a history of acute Charcot foot required surgical intervention.
“As long as you have a stable, plantigrade limb that is ulcer-free, I think you have achieved success,” said Dr. Liu.—Eileen Koutnik-Fotopoulos










