Increasing Adherence, Patient Engagement with Virtual Health Assistants
Orlando—The number of individuals with at least 1 chronic illness is increas- ing at an alarming rate, according to the Centers for Disease Control and Prevention. A 2012 report from the Agency for Healthcare Research and Quality found that 50% of medications for chronic disease are not taken as prescribed. Non-adherence has been estimated to cost the US healthcare system between $100 billion and $289 billion annually in direct costs. This data illustrates the need for new approaches to patient adherence and outcomes. Advances in computer technology may offer a new way of delivering care that is both patient focused and economical. During a session at the NAMCP forum, Thomas Morrow, MD, chief medical officer, Next IT, discussed patient adherence, the vital role of patient engagement, and how virtual health assistants (VHAs) have the potential to reshape healthcare.
Dr. Morrow cited a study by Nieuwlaat and colleagues that assessed the effects of interventions intended to enhance patient adherence to prescribed medications for medical conditions, on both medication adherence and clinical outcomes [Cochrane Database Syst Rev. 2014;11:CD000011]. Based on the findings, the researchers concluded that “current methods of improving medication adherence for chronic health problems are mostly complex and not very effective, so that the full benefits of treatment cannot be realized.”
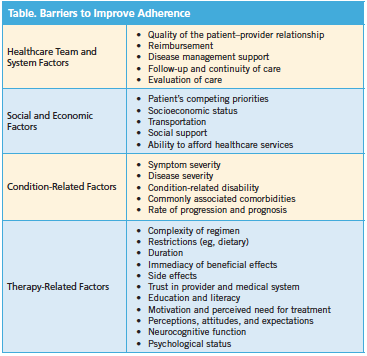
He reviewed barriers that have contributed to the failure to improve adherence (Table). Behaviors of individuals are crucial to health outcomes and behaviors can be changed, said Dr. Morrow, who outlined the science of behavior change. The most popular used theories in behavioral health include:
• Social cognitive theory: Human behavior is a product of dynamic interplay of personal, behavioral, and environmental influences
• Trans-theoretical model/stages of change: Behavior is a process that unfolds over time through a sequence of changes
• Health belief model: People’s actions are dependent upon their feelings of susceptibility, seriousness, benefits and barriers to behavior, triggers to action, and conviction that action will produce expected outcome
Behavior change centers on the relationship between the patient and healthcare professionals, according to Dr. Morrow. Interpersonal communication is one of the most critical factors in changing health behaviors. Motional interviewing is another approach to help change behavior because it is collaborative based, patient-centered, and helps patients to become more self-motivated. Healthcare professionals also need to be cognizant of ambivalence. Patients who are noncompliant are typically ambivalent about changing chronologically unhealthy behavior. By recognizing and discussing patients’ ambivalence in a nonjudgmental way helps them to acknowledge the problem. Empathy is also important. When patients feel understood and not judged, they are more apt to open up, said Dr. Morrow.
Technology Solutions
Adoption of mobile medical apps by clinicians and consumers continues to increase. However, these healthcare apps may be limited in their ability to improve patient care. Dr. Morrow cited a study published in 2013 by the IMS Institute for Healthcare Informatics titled Patient Apps for Improved Healthcare: From Novelty to Mainstream that categorized and analyzed the value of healthcare apps available on iTunes. Of the 43,689 apps available for download as of June 2013, the finding showed that:
• Only 54% are genuine healthcare apps
• Most focus on overall wellness, are simple in design, and do little more than provide information
• Only 159 can track or capture user-entered data
• Fewer than 50 relate to condition management or provide tools and calculators for users to measure vitals
• 90% scored >40 out a possible 100 for functionality
• 50% have been downloaded <500 times
• Patients and physicians have to find and navigate the maze with little guidance
A newer technology gaining momentum in the healthcare arena is VHAs—digital representatives (also known as avatars) that live on websites, smart phones, and other devices. VHAs use a specialized form of artificial intelligence that combines the ability to understand natural—or everyday—language, characterize human intent, deliver resolutions, and facilitate tasks in a highly contextual manner. VHAs can promote patient education, adherence, and outcome; facilitate adverse drug reaction reporting; determine reasons for nonadherence; discuss assistance programs with patients; produce more revenue for the pharmaceutical industry; and promote formulary compliance.
Dr. Morrow cited studies demonstrating the clinical benefits of VHA. One study found that a virtual discharge nurse reduced readmissions at the 30-day mark by 30%. Furthermore, 74% of pilot-study hospital participants would rather interact with an intelligent virtual assistant than an actual human being. Another study examined the use of a VHA to facilitate antipsychotic medication adherence for patients with schizophrenia. The findings showed that antipsychotic medication adherence increased to 89% from the historical rate of 50%, according to Dr. Morrow.
VHAs are not just for clinical interactions, he noted. For example, a virtual case manager call center can replicate 80% of human interactions with 99% accuracy. They can also exponentially expand reach and frequency, personalized engagement, real-time behavior discern- ment and interventions, and monitoring and tracking capabilities, said Dr. Morrow.
He concluded the forum outlining an industry report on the global virtual assistant market from 2012 to 2020. “The global intelligent virtual assistant market is projected to exceed $3 billion USD by 2020. Increased focus in effective client communication, made easy by virtual assistants, is expected to drive the intelligent virtual assistant market over the forecast period,” according to the report.—Eileen Koutnik-Fotopoulos