Improving Care Coordination in Medicaid Managed Care
Alexandria—An increasing number of aging adults and disabled individuals are enrolling in Medicaid partly due to the recent decision by many states to expand Medicaid coverage. The current estimate of enrollees is 17 million. Managed care organizations (MCOs) are now confronted with issues associated with this increase; 1 challenge is ensuring all enrollees receive proper healthcare.
Marcia LeBlanc, BSBA, national long-term services and support (LTSS) director, Aetna Medicaid, and Daniel D. Cave, chief executive officer, consumer care management group, Centene Corporation, discussed best practices for coordinating Medicaid healthcare services during a session at the LSMMC meeting.
“If you asked everyone in the room [what coordinated care means] you would get 100 different answers,” said Ms. LeBlanc, who opened the session. MCOs can utilize care coordination to decrease cost and improve member outcome. Ms. LeBlanc noted that care coordination always starts with a comprehensive needs assessment. To motivate a member to be involved and engaged with their care, Ms. LeBlanc suggested scheduling face-to-face interactions where the member resides. This provides a better understanding of the member’s behavioral, medical, and social needs, while cultivating a trusting relationship.
“Develop along with your member an individualized care plan,” said Ms. LeBlanc. “Ask members for [his or her] permission on things.” Members should be involved in care planning, 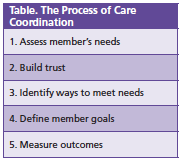 such as giving the care manager permission to enter the home and discussing what goals of care are most important to them. “There may be things more important than medical care for [some] members, particularly those near end-of-life care,” said Ms. LeBlanc. See Table for the care coordination process.
such as giving the care manager permission to enter the home and discussing what goals of care are most important to them. “There may be things more important than medical care for [some] members, particularly those near end-of-life care,” said Ms. LeBlanc. See Table for the care coordination process.
While all Medicaid members would benefit from improved care coordination, there are 7 types of members who would benefit significantly: (1) behavioral health members; (2) certain pharmaceutical members; (3) high cost members; (4) LTSS members; (5) members who experience enrollment gaps; (6) members who frequent the emergency room (ER); and (7) members who have frequent inpatient stays.
MCOs can evaluate how well care coordination is working for their mem- ber by performing standardized health surveys and environmental safety surveys. MCOs should ensure the member’s primary caregiver is not exhausted and has all the resources they need.
Shortfalls often happen during transitions of care. To prevent this, Ms. LeBlanc suggested implementing a nursing facility diversion program and creating partnerships between MCOs and the healthcare facilities where the member is treated. MCOs should also monitor members post-hospitalization and transitions from nursing facilities into the community.
For care coordination to be successful, primary care physicians (PCPs) must be involved. Members should communicate their goals to the PCPs and, in turn, PCPs should be notified of member hospitalizations and ER visits. PCPs, members, and caregivers should work together to monitor the member’s health.
Mr. Cave followed up to discuss how care management could be improved. He noted that managed care has not used technology to its fullest extent. Members and caregivers should be able to use technology to find medical services, make appointments, set scheduling reminders, and communicate with their physicians or Medicaid representatives. Integrating technology into managed care enables remote monitoring of members, and Mr. Cave said this will reduce call volumes, creating improved customer experience, increasing retention of members, and ultimately, helping to close the care gap. “A care gap is an indicator that we can make a difference,” said Mr. Cave.
He noted strategies to engage the mem- ber in a successful manner, including providing relevant and timely information specific to the member’s needs and culture; easing the communication between patient, provider, and physician; understanding patient barriers and cul- ture; providing reminders; interactivity; feedback; and adaptive options. Mr. Cave said looking into a member’s location can allow for better guidance on food options, safe areas to walk and engage in exercise, and communicate clearly to ensure the best care results.
Patient-centered care is the key to successful care coordination. Mr. Cave urged managed care professionals to change their view of enrollees, “Think of the member as a consumer,” said Mr. Cave.—Melissa D. Cooper













