Examining Psoriasis and PsA Treatment Landscape
San Diego—In light of new drug developments in psoriatic disease as well as expanding uses of current agents, managed care organizations and payer organizations need to appropriately and effectively design benefits that optimize both cost efficiency and outcomes.
During a satellite symposium at the AMCP meeting, experts discussed current clinical data, pharmacy benefit designs, and management resources for managed care professionals to consider in treating psoriasis and psoriatic arthritis (PsA). Educational grants from Celgene Corporation, Janssen Biotech, Inc., and Novartis Pharmaceuticals Corporation supported the symposium.
Psoriasis Overview
“Psoriasis is a disease that is tremendously unmanaged at this present time,” said Alan Menter, MD, chief, division of dermatology, Baylor University Medical Center, Dallas, TX, who provided an overview of psoriasis.
Psoriasis is the most prevalent immune-mediated disease in the United States affecting approximately 7.5 million Americans. Psoriasis is also associated with comorbidities including obesity and metabolic syndrome, and autoimmune diseases. Furthermore, chronic moderate-to-severe plaque psoriasis remains undertreated. Dr. Menter cited a study by Armstrong and colleagues that looked at undertreament, treatment trends, and treatment discontinuation among 5604 patients with psoriasis and PsA who completed biannual National Psoriasis Foun- dation surveys conducted from January 1, 2003, and December 31, 2011 [JAMA Dermatol. 2013;149(10):1180-1185].
The findings showed that 49.2% of patients with mild psoriasis, 23.6% of patients with moderate psoriasis, and 9.4% of patients with severe psoriasis were undertreated. Among those receiving treatment, 29.5% of patients with moder- ate psoriasis and 21.5% of patients with severe psoriasis were treated with topical agents alone. The treatment of psoriasis also presents a significant financial bur- den on healthcare; the total direct and indirect healthcare costs of psoriasis are $135 billion in the United States [JAMA Dermatol. 2015; DOI: 10.1001/jamader- matol.2014.3593].
Dr. Menter reviewed the factors in- fluencing therapeutic success. Establishing treatment goals are important. The clinical goal of psoriasis treatment is for clinicians to find the most efficient treatment associated with the fewest possible adverse events at a reasonable cost. Goal orientated treatment strategies include establishing clear treatment goals during the discussion of psoriasis therapy, regularly evaluating treatment response, and modifying therapy when results are insufficient. Patient preferences need to be considered when recommending an individualized treatment plan, according to Dr. Menter.
Treatment of PsA in Managed Care
Neal Birnbaum, MD, FACP, MACR, director, division of dermatology, California Pacific Medical Center, continued the session focusing on PsA treatment in a managed care setting.
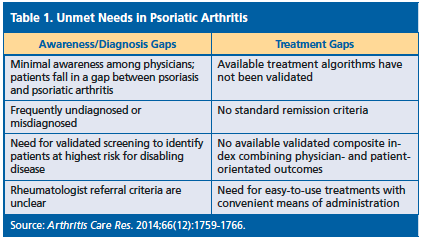
PsA poses a significant clinical and economic burden. Although, considered to be a mild disease, 30% to 40% of patients develop joint complications. Dr. Birnbaum spoke about the healthcare expenditures of PsA, citing a study by Lee and colleagues. The study found that the average annual direct and indirect cost associated with PsA ranged from approximately $8367 to $18,110. Hospitalizations accounted for 60% of direct costs, while disability and loss of productivity accounted for the majority of indirect costs [PT. 2010;35(12):680- 689]. Data has also shown that patients with PsA are often undiagnosed or misdiagnosed (Table 1).
PsA Treatment Recommendations
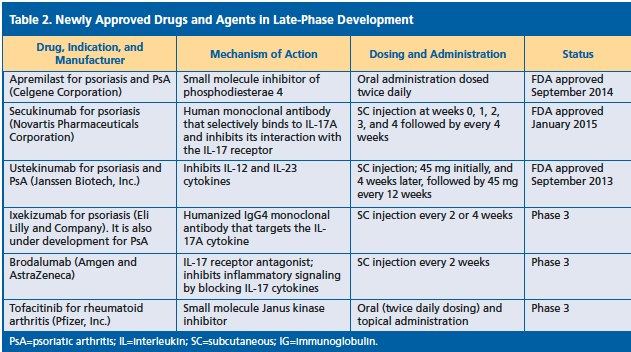
Dr. Birnbaum noted that several newly approved agents have novel mechanisms of action (Table 2). He also outlined goals of treatment, which include to relieve or reduce joint pain, reduce joint inflammation, reduce swelling and tenderness, prevent or delay joint damage, and improve function in daily activities. “Early diagnosis and treatment is associated with remission of symptoms,” he said. “Multidisciplinary care may facilitate the diagnosis of joint disease and offer a more comprehensive treatment approach for patients with psoriatic disease.”
Strategies for Managed Care
Jeffrey Dunn, PharmD, MBA, senior vice president, chief clinical officer, VRx Pharmacy Services, LLC, concluded the symposium discussing the application of comparative effectiveness research (CER) and tips and tools to implement new care models. Providers, patients, and payers are challenged to identify the most effective allocations of agents for optimal psoriatic disease management, he said, noting that little data exists to guide individualization of therapy. CER provides evidence to compare the effectiveness and safety of psoriasis and PsA therapies when head-to-head data is lacking. The results are used to support clinical decision-making and designed to reflect “real-world” settings of day-to-day patient care. While the increasing number of treatment options benefits patients, providers, and payers, these stakeholders are challenged by the acquisition cost of these therapies, according to Dr. Dunn. “New plan designs and care models that emphasize value over volume of care are being implemented to ensure patients continue to have access to these innovative psoriatic disease therapies,” he said. New models of care delivery that share themes consistent with models and tactics used by accountable care organizations to drive value include patient-centered medical homes and payment mechanism focused on “fee-for-value” rather than “fee-for-volume.”—Eileen Koutnik-Fotopoulos